11. Interstitial lung diseases
advertisement

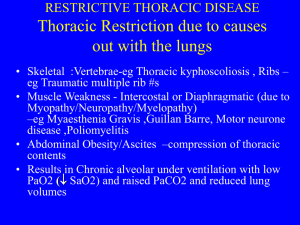
Interstitial Lung Diseases (ILD) Diffuse Parenchymal Lung Diseases (DPLD) Edit Csada, MD 29.10.2014. 1 Interstitial lung disorders (ILD) The interstitial lung disorders are chronic, nonmalignant, noninfectious diseases of the lower respiratory tract characterized by inflammation and derangement of the alveolar walls. Secondary fibrosis and pulmonal hypertension may develop Prevalence: 7-20/100 000 2 Etiology (ATS/ERS 2002) 1. Known origin Drugs (busulfan, nitrofurantoin, bleom., amiodaron) Pneumoconiosis Connective tissue diseases Irradiation Malignant diffuse infiltr. lung diseases 2. Granulomatous origin Sarcoidosis Hypersensitive pneumonitis 3 Etiology 3. Other DPLD Langerhans-cell histiocytosis Lymphangioleiomyomatosis Alveolar proteinosis Wegener granulomatosis 4. IIP UIP (IPF) DIP/RBILD NSIP AIP COP LIP 4 According to the pathogenesis I. Acute DPLD allergy (drugs) toxin (gas) vasculitis/hemorrhage (Goodpasture, idiopathic hemosiderosis) ARDS (trauma, septicaemia) unknown (COP, BOOP) 5 According to the pathogenesis II. Episodic DPLD eo pneumonia vasculitis, hemorrhage Churg-Strauss sy Hypersensitive pneumonitis COP 6 According to the pathogenesis III. Chronic DPLD (exposition) inorganic dusts (silicosis, asbestosis) organic dusts (bacteria, fungi, animal proteins) drugs 7 According to the pathogenesis IV. Chronic DPLD (systemic diseases) sarcoidosis connective tissue diseases malignant diseases (lymphoma, lymphangitis cc) vasculitis (Wegener) hereditary diseases others ( bone marrow transplantation, inflammatory intestine diseases, amyloidosis) 8 According to the pathogenesis V. Chronic DPLD (without systemic disease and without exposition) Idiopathic interstitial pneumonitis (IIP) alveolar proteinosis chronic aspiration LAM Langerhans-cell histiocytosis venoocclusive disease idiopathic pulmonal haemosiderosis bronchioloalveolar cc. 9 Morphologic changes Loss of pulmonary capillaries Alterations of alveolar epithelial cells Fibrosis of alveolar walls Pathogenesis Total number of inflammatory cells increases The proportions of inflammatory cells change The inflammatory cells are activated Mediators release – toxic oxygen radical, proteases Fibrosis Impairment of O2 transport 10 Normal cell content of BAL 90% 7% 1% alveolar macrophages lymphocytes polymorph leucocytes 11 •Neutrophyl alveolitis : cryptogenic fibrotic alveolitis •Lymfocytic alveolitis : sarcoidosis, hypersensitive pneumonitis, beryllosis •Eosinophil alveolitis •Mixed-cell alveolitis: amiodaron fibrosis (eosinophil+lymphocyte) 12 Clinical features in ILD I. Symptoms Dyspnea during exercise Fatigue Nonproductive cough Physical finding Dry, crackling rales Wheezing Tubular breath sounds Digital clubbing 13 Clinical features in ILD II. Laboratory changes ERS can be elevated Hypoxaemia Chest X-ray, HRCT scan Reticular Nodular Reticulonodular Ground glass haziness Honeycombing 14 Clinical features in ILD III. Lung function tests Scintigraphic findings Tc99, Xe133 Reduction in VC, TLC FEV1/FVC is normal, or supranormal Decrease in diffusing capacity, transfer factor (DLCO) Oxyergospirometry (exercise test) Patchy abnormalities BAL Various mixtures of inflammatory cells 15 16 17 18 19 20 21 Diagnosis of ILD Clinical features Transbronchial biopsy VATS Open lung biopsy 22 Therapy of ILD Known etiology Remove the individual from exposure to the causative agents Known and unknown etiology Suppress inflammatory process Oral corticosteroids (1mg/kg0,25 mg/kg) CPA (cyclophosphamide) Imuran (azathioprine) Late stage O2 therapy Supportive treatment Transplantation 23 Idioptahic pulmonary fibrosis (IPF) Hamman-Rich sy (acute IP) Cryptogenic fibrosing alveolitis (COP) Desquamative intersitial pneumonitis (DIP) Usual interstitial pneumonitis (UIP) Respiratory bronchiolytis-associted IP (RBILD) Nonspecific interstitial pneumonitis (NSIP) Lymphoid interstitial pneumonitis (LIP) 24 Idioptahic pulmonary fibrosis (IPF) The cause of condition is not clear. Chr. inflammatory process initiated by immune complexes derangement of the lung parenchyma The clinical features are similar to other ILD 25 Radiologic changes of IPF Ground glass haziness Streaky wisps of shadow Generalized micronodular mottling Honeycomb lung 26 Diagnosis of IPF Clinical features X-ray CT scan Diffusing capacity, transfer factor decreased (DLCO) BAL (neutr.) Transbronchial biopsy VATS Open lung biopsy 27 ATS/ERS diagnostic criteria of IPF (biopsy) Major criteria There is no known cause of ILD (drug, environmental exposition) Impaired lung function, restriction, decreased diffusion capacity Bilateral basal reticular, streaky shadow, minimal granulomas There is no other diseases with similar symptoms Minor criteria Age > 50 There is no other cause of dyspnoe Duration of disease > 3 month Bilateral basal subcrepitatio AJRCCM 2002;165:277-304 28 Therapy of IPF (ATS) No treatment Early and combined treatment CS+ azathioprine CS+ cyclophosphamide CS+ azathioprine+ N-acetylcysteine Restaging after 3-6-9-12-18 month Age > 70 years Extreme obesity DM, hearth disease, osteoporosis Severe impaired lung function Honeycomb lung Symptoms, radiology, lung function, side effects PR, transplantation Best supportive care, O2 treatment 29 Therapy of IPF (ATS) New drugs Interferon Bosentan Etanercept Pirfenidon 30 Sarcoidosis (Morbus Boeck) It is clinically well defined, systemic, granulomatous disease of unknown origin. Histology Altered immune response 31 Clinical features of sarcoidosis 32 Radiological appearances of sarcoidosis Stage/form I Stage/form II Stage/form III BHL sy pulmonary dissemination with or without BHL pulmonary fibrosis 33 34 35 36 Diagnosis of sarcoidosis BHL accompanied by erythema nodosum (Löfgren-sy) Tuberculin test: negative Lung function tests Se ACE (angiotensin converting enzyme) increases Transbronchial biopsy, perbronchial biopsy (TBNA) BAL (ly) Gallium scan Mediastinoscopy 37 Treatment of sarcoidosis Stage I: no treatment is necessary Indication of steroid treatment: Progressive pulmonary disease Severe uveitis Hypercalcaemia Neurological involvement 38 Histiocytosis X (Langerhans) This is a disorder of the mononuclear phagocyte system characterized by the accumulation of mononuclear phagocytes is various organs. In pediatric patients Letterer-Siwe disease Hand-Schüller-Christian disease In adults Histiocytosis X Eosinophilic granuloma 39 Clinical features of histiocytosisX 20-40 years of age (smoking) Nonproductive cough Dyspnea Chest pain Ptx – 10% of all cases 40 Characteristics of histiocytosisX X-ray changes Lung function tests Large number of mononuclear phagocytes Histology Mixed restrictive-obstructive pattern Decreased diffusing capacity BAL Reticulonodular shadow Small cystic spaces X bodies (Birbeck) in the cytoplasm There is no known treatment. Corticosteroids may be given. 41 Langerhans-cell histiocytosis 42 Rheumatoid arthritis Treatment If the disease is mild, no specific therapy is used. If the ILD is progressive, corticosteroids are administered. 43 Other immunological diseses SLE Sjögren sy Scleroderma Bechterew Dematomyositis, polymiositis Periarteritis nodosa Neurofibromatosis 44 Alveolar proteinosis Primary-secondary (myeloid leukaemy, dust) PAS positive lipoprotein X-ray: butterfly shape infiltration Therapy: BAL 45 Eosinophylic pneumonias The eosinophylic pneumonias are characterized by eosinophilic pulmonary infiltrates and commonly peripherial blood eosinophylia. Known and unknown etiology 46 Eosinophylic pneumonias Known etiology Allergic bronchopulmonary aspergillosis (ABPA) Parasitic infestations (ascaris, toxocara,etc) Drug reactions (nitrofurantoin, sulphonamides) Idiopathic (unknown etiology) Löffler’s sy Benign, acute eosinophilic pneumonia (AEP) with migrating pulmonary infiltrates and minimal clinical manifestation. Chr. eosinophilic pneumonia (CEP) Symptoms: cough, sweats, fever, anorexia, weight loss, chills X-ray: Peripherial infiltrates Allergic granulomatosis of Churg and Strauss Hypereosinophilic sy (HES) Therapy: corticosteroids 47 PNEUMOCONIOSIS Etiologic agents: inhalation of inorganic dusts metal dusts free silica coal dusts 48 HYPERSENSITIVE PNEUMONITIS (Extrinic allergic alveolitis) It is an immunologically induced inflammation of lung parenchyma involving alveolar walls and terminal airways secondary to repeated inhalation of a variety of organic dusts and other agents by susceptible host. Manifestations: Farmer’s lung (1932) – thermophylic actinomycetes Bird fancier’s breeder’s or handler’s lung Miller’s lung Bagassosis Byssinosis Air conditioner’s lung Coffee worker’s lung 49 Thank you for your attention! 50