Inflammatory and Infectious
Disorders of the Skin
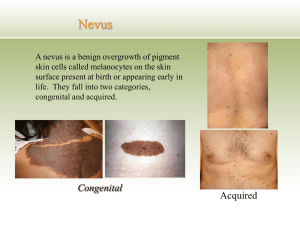
Objectives
1. Describe and discuss, Dermatitis, Acne Vulgaris , Urticaria,
Psoriasis, Seborrheic Keratosis. Scleroderma, Systemic Lupus
Erythematous, Shingles,scabies, and impetigo as to definition,
etiology, pathophysiology, signs and symptoms, diagnosis, medical
and nursing management.
2. Apply the nursing process for clients with inflammatory and
infectious disorders of the skin.
3. Recognize systemic disorders with dermatologic symptoms.
Dermatitis
A general term used to describe inflammation of the
skin.
Description
Most types of dermatitis are characterized by an itchy
pink or red rash
Pruritus: itching
May be localized or generalized
Types of Dematitis
1. Allergic or contact dematitis is an allergic
reaction to something that irritates the skin and is
manifested by one or more lines of red, swollen,
blistered skin that may itch or seep.
It usually appears within 48 hours after
touching or brushing against a substance to
which the skin is sensitive.
More common in adults than in children.
Etiology: in patients with allergies, sensitized mast cells in
the skin release histamine, causing a red rash, itching,
and localized swelling
Types of Dermatitis
2. Irritant dermatitis is a localized reaction that occurs
when the skin comes into contact with a strong
chemical such as a detergent
Etiology: the caustic quality of the substance damages
the protein structure of the skin or eliminates
secretions that protect it.
Dermatitis
Contact dermatitis of the (left) face and
(right) wrist
Dermatitis
Contact dermatitis
Vesiculation: blister formation and oozing
Can occur on any part of the body, but it usually affects
the hands, feet, and groin.
Contact dermatitis usually does not spread from one
person to another, nor does it spread beyond the area
exposed to the irritant unless affected skin comes into
contact with another part of the body.
Contact dermatitis
Medical Management: Remove the source of irritation
Flushing the skin with cool water
Burow’s solution wet dressings
Topical lotions such as calamine
Antihistamines such as Benadryl (diphenhydramine)
Corticosteroids: topically or orally
POISON IVY
Poison Ivy/Oak
Poison Ivy Rash
Atopic Dermatitis
This form of dermatitis, commonly referred to as eczema, is a
chronic condition that causes itchy, inflamed skin.
Most often, it occurs in the folds of the elbows, backs of the knees
or the front of the neck.
It tends to flare periodically and then subside for a time, even up
to several years.
The exact cause of this skin disorder is unknown, but it may result
from a malfunction in the body's immune system.
Atopic Dermatitis: Eczema
Eczema: Atopic Dermatitis
Dermatitis
Pathophysiology and Etiology
Types: Allergic contact; primary irritant
Assessment Findings
Blood vessel dilation; itching; vesiculation
Skin patch test; visual examination
Acne Vulgaris
Acne of (left) the face and (right) the
chest
Acne Vulgaris
Condition which coincides with puberty; believed to be
related to hormone levels that occur when secondary sex
characteristics are developing.
An inflammatory disorder that affects the sebaceous glands
and hair follicles
Severity of the condition varies from minimal to severe
Acne Vulgaris
Pathophysiology and Etiology
Overproduction of sebum
Assessment Findings
Comedones (blackhead); oily scalp
Visual examination
Medical Management
Gentle facial cleansing; drying agents containing benzoyl
peroxide
Topical and oral drugs and antibiotics
Removal with instruments
Acne
Develops as a result of blockages in follicles. Hyperkeratinization
and formation of a plug of keratin and sebum (a microcomedo) is
the earliest change.
Enlargement of sebaceous glands and an increase in sebum
production occur with increased androgen production .
The microcomedo may enlarge to form an open comedo
(blackhead) or closed comedo (whitehead).
Increased sebum production provides an environment for the
overgrowth of Propionibacterium acnes.
Acne
Severe cases can cause permanent scarring
Medical Management: Gentle facial cleansing and non-
prescription agents
Drug therapy: Retin-A (tretinoin) topically or Accutane
(isotretinoin) orally
Antibiotics: tetracycline and erythromycin
Acne Vulgaris
Surgical Management
Dermabrasion for surface scarring
Nursing Management
Client teaching
Cleanliness: Face and hair
Avoid cosmetics, Manipulation of lesions
Precautions for pregnant women: Risk associated with
systemic oral Retin - A (isotretinoin) for birth defects
Rosacea
A chronic skin disorder that manifest in a variety of ways
Usually characterized by a rosy appearance
Cause is unknown: possible genetics, immunological factors,
exposure to UV light, bacterial skin infection with
Helicobacter pylori
or a mite infestation of the facial hair follicles
Over time, continued dilation of facial capillaries and
arterioles causing visible streaks on the skin called
telangiectases
Rosacea
Rosacea
S/S: Flushing of skin, like a persistent sunburn, face appears
swollen and baggy, facial pores enlarge, nose becomes
enlarged (rhinophyma)
Medical Management:
Antibiotics, topical medications
Laser treatments; pulsed light treatments
Nursing management: patient teaching re: reduce sun
exposure, gentle cleansing, stress-management
Furuncles, Furunculosis and
Carbuncles
Furuncle: a boil
Furunculosis: multiple furnuculosis
Carbuncle: a furuncle which drains pus
Causes: skin infections caused by bacteria which normally live
harmlessly on the skin
Predisposition by: diabetes, poor diet and general health,
immunodepression
Furuncle - Boil
Furuncle - Treatment
C&S of pathogen
Hot wet soaks, antibiotics, surgical incision and drainage (I &
D)
Strict aseptic technique when changing dressings to avoid
spreading the infection to other parts of the body
Question
Is the following statement true or false?
Furuncles, furunculosis, and carbuncles are treated with antibiotic
therapy.
Answer
True.
Furuncles, furunculosis, and carbuncles are the result of skin
infection or diabetes mellitus. A culture and sensitivity lab result
indicates the proper antibiotic to use in treatment.
Psoriasis
Pathophysiology, Etiology: Likely genetic predisposition;
Keratinocytes; Plaque
Assessment Findings: Signs and Symptoms
Erythema with silvery scales; Lesions
Diagnostic Findings: Visual examination; Skin biopsy
Medical Management: Symptomatic treatment; Drug
therapy; Biologic therapy;
Photochemotherapy
Psoriasis
Named for the Greek word psōra meaning "itch," psoriasis is
a chronic, non-contagious disease characterized by inflamed
lesions covered with silvery-white scabs of dead skin.
Psoriasis
Psoriasis
Psoriasis on
the elbows
Psoriasis
Pathophysiology
Normal skin cells mature and replace dead skin every
28–30 days.
Psoriasis causes skin cells to mature in less than a week.
Because the body can't shed old skin as rapidly as new
cells are rising to the surface, raised patches of dead skin
develop on the arms, back, chest, elbows, legs, nails,
folds between the buttocks, and scalp.
Psoriasis is considered mild if it affects less than 5% of the
surface of the body; moderate, if 5–30% of the skin is
involved, and severe, if the disease affects more than 30% of
the body surface.
Nursing Process:
The Client With Psoriasis
Assessment
Skin integrity; appearance
Family history of psoriasis
Triggering factors
Diagnosis, Planning, and Interventions
Impaired skin integrity
Disturbed body image
Nursing Process:
The Client With Psoriasis
Evaluation of Expected Outcomes
Improved integrity and appearance of skin
Reduced itching; copes effectively with altered appearance
Pediculosis
DIAGNOSIS
Head and pubic lice infestations are diagnosed by finding
lice or viable eggs (nits) on examination. Excoriations
and pyoderma (any pus-containing skin infection) also
may be present.
Pediculosis - Treatment
Topical Agents - Over-the-counter agents approved by
the U.S. Food and Drug Administration (FDA) belong to
the pyrethrum group of insecticides (pyrethroids). Both
4 percent piperonyl butoxide0.33 percent pyrethrins
(e.g., Rid, Pronto) and 1 percent permethrin (Nix) are
safe and effective. Experts consider permethrin as the
treatment of choice.
Oral Agents. Ivermectin (Stromectol), in an oral dose of
200 mcg per kg, effectively kills nymphs and lice, but not
eggs. To kill newly hatched nymphs, a second dose should
be given seven to 10 days after the first dose..
Scabies
Pathophysiology, Etiology: Itch mite; Spread by skin-to-skin contact
Assessment Findings: Signs and Symptoms
Itching; Excoriation
Diagnostic Findings: Visual examination; Ink or mineral oil test
Medical Management: Scabicide application; Thorough bathing, clean
clothing, avoiding contact with those infected
Nursing Management
Scabies Mite
Scabies
Treatment
Apply a mite-killer like permethrin (brand name: Elimite).
These creams are applied from the neck down, left on overnight, then
washed off.
This application is usually repeated in seven days. An alternative
treatment is 1 ounce of a 1% lotion or 30 grams of cream of lindane,
applied from the neck down and washed off after approximately eight
hours.
Since lindane can cause seizures when it is absorbed through the skin,
it should not be used if skin is significantly irritated or wet, such as
with extensive skin disease, rash, or after a bath.
As an additional precaution, lindane should not be used in pregnant or
nursing women or children younger than 2 years old.
Lindane is only recommended if patients cannot tolerate other
therapies or if other therapies have not been effective.
2. An oral medication, ivermectin, is an effective scabicide that
does not require creams to be applied.
3. Antihistamines, such as diphenhydramine (Benadryl) can
be useful in helping provide relief from itching.
4. Wash linens and bedclothes in hot water. Because mites
don't live long away from the body, it is not necessary to
dry-clean the whole wardrobe, spray furniture and rugs,
and so forth.
5. Treat sexual contacts or relevant family members (who
either have either symptoms or have the kind of
relationship that makes transmission likely).
Dermatophytoses
Dermatophytose: Tinea: Caused by a parasitic fungi; which invade
skin, scalp, and nails
Ringworm; Athlete’s foot; Jock itch
Assessment Findings: Rings of papules or vesicles; Sore skin
Medical Management: Oral, topical antifungal agents
Burow’s solution, Micatin (miconazole)
Nursing Management: keeping skin day, avoid excessive heat and
humidity, dry socks, don’t go barefoot in locker rooms
Ringworm - fungus (tinea corporis)
Ringworm - fungus
Athelete’s foot - fungus (tinea pedis)
Dermatophytoses
Tinea named after the location on the body
Tinea pedis - foot
Tinea capitis - head
Tinea corporis - body
Tinea cruris - groin
Shingles - Viral infection
Also called Herpes Zoster: Varicella-zoster virus; Inflammation in
dermatome
Virus remains dormant in the nerve roots
More common in older adults and people who are
immunocompromised
Assessment Findings: Signs and Symptoms
Fever; Headache; Vesicles; Itching, pain
Medical Management: Oral or topical Zoviraz (acyclovir);
Corticosteroids
Nursing Management : warm soaks, avoid contact with
immunocompromised patients
Shingles - Herpes Zoster
Shingles
Patient is placed on AIRBORNE PRECAUTIONS:
(particles are less than 5 mcg)
Private room or cohort room; Masks, gowns and gloves for
all patient care
Door to room should remain closed
Should be negative air pressure room
Pregnant health care personnel who have not had chickenpox
probably should not care for the patient
Shingles
Herpes Simplex - A recurrent viral disease caused by
the herpes simplex virus
a. type one - marked by the eruption of fluid-containing vesicles on the
mouth, lips, or face.
b. type two - marked by the eruption of fluid-containing vesicles on the
genitals
Treatment
Acyclovir (Zovirax) is the drug of choice for herpes infection and can be
given intravenously or taken by mouth or ointment but is not very
useful in this form. A liquid form for children is also available.
Herpes Simplex
Urticaria
A vascular reaction pattern of the skin marked by the
transient appearance of smooth, slightly elevated patches
that are more red or more pale than the surrounding skin
and are accompanied by severe itching.
Also called hives.
Non-allergic urticaria
Mechanisms other than allergen-antibody interactions are
known to cause histamine release from mast cells. For instance,
a diverse group of signaling substances called neuropeptides
have been found to be involved in emotionally induced
urticaria.
Urticaria
Uticaria - Hives
Urticaria
An acute or chronic condition characterized by the
appearance of itchy weals on the skin.
The cause may be an allergy to certain foods ,
drugs, emotional stress, or local skin irritation
resulting from contact with certain plants.
Athletes sometimes develop hives while exercising
(exercise-induced urticaria). The hives are small
and seem to develop in response to the release of
histamines associated with the increase in body
temperature produced by exercise.
Urticaria
Treatment & Management
Most treatment plans for urticaria involve being aware
of one's triggers.
If one's triggers can be identified then outbreaks can
often be managed by limiting one's exposure to these
situations.
Drug treatment
Typically in the form of Antihistamines such as diphenhydramine,
hydroxyzine, cetirizine and other H1 receptor antagonists. These
are taken on a regular basis to protective effect, lessening or
halting attacks.
For some people, H2-receptor antagonists such as cimetidine
(Tagamet) and ranitidine (Zantac) can also help control symptoms
either protectively or by lessening symptoms when an attack
occurs.
When taken in combination with a H1 antagonist it has been
shown to have a synergistic effect which is more effective than
either treatment alone.
Seborrheic Keratosis
A superficial, benign, verrucose lesion consisting of
proliferating epidermal cells enclosing horn cysts, usually
appearing on the face, trunk, or extremities in adulthood.
Seborrheic Keratosis
Sign And Symptoms
The growths resemble flattened or raised warts, but
have no viral origins and may exhibit a variety of
colors, from pink or yellow through brown and black.
Because only the top layers of the epidermis are
involved, seborrheic keratoses are often described as
having a "pasted-on" appearance.
Etiology
A mutation of a gene coding for a growth factor receptor
(FGFR3), has been associated with seborrheic keratosis.
Treatment
Because the tumors are rarely painful, treatment is not
often necessary.
If a growth becomes excessively itchy, or if it is irritated
by clothing or jewelry, cryosurgery has been found to be
highly effective in their removal.
With resemblance to malignant melanomas, which has
sometimes led to a misdiagnosis of the cancerous
lesions. If there is any doubt, a skin biopsy will allow a
physician to make a correct diagnosis.
Scleroderma
Scleroderma is a progressive disease that affects the
skin and connective tissue (including cartilage, bone,
fat, and the tissue that supports the nerves and blood
vessels throughout the body).
There are two major forms of the disorder. Localized
scleroderma mainly affects the skin. Systemic
scleroderma, which is also called systemic sclerosis,
affects the smaller blood vessels and internal organs
of the body.
Scleroderma
SCLERODERMA
Scleroderma
Is an autoimmune disorder, which means that the body's
immune system turns against itself. In scleroderma,
there is an overproduction of abnormal collagen (a type
of protein fiber present in connective tissue). This
collagen accumulates throughout the body, causing
hardening (sclerosis), scarring (fibrosis), and other
damage.
Therapy
There is no cure for every patient with scleroderma, though there
is treatment for some of the symptoms, including drugs that
soften the skin and reduce inflammation. Some patients may
benefit from exposure to heat.
A range of NSAIDs (nonsteroidal anti-inflammatory drugs) can be
used to ease symptoms, such as naproxen. If there is esophageal
dysmotility .Care must be taken with NSAIDs as they are gastric
irritants, and so a proton pump inhibitor (PPI) such as
omeprazole can be given in conjunction.
Treatment
Immunosuppressant drugs, such as mycophenolate
mofetil (Cellcept®) or cyclophosphamide are
sometimes used to slow the progress.
Digital ulcerations and pulmonary hypertension can be
helped by prostacyclin (iloprost) infusion. Iloprost
increases blood flow by relaxing the arterial wall.
Sytemic Lupus Erythematous
Lupus is a condition characterized by chronic inflammation
of body tissues caused by autoimmune disease.
Autoimmune diseases are illnesses that occur when the body's
tissues are attacked by its own immune system.
SLE - NECK
Systemic Lupus Erythematosus
• Medical Management: Producing remission; Prevent/Treat
exacerbations; Medications
– Renal, Cardiac, GI, CNS symptomatic treatment
• Nursing Management
Systemic Lupus Erythematosus (SLE)
Pathophysiology, Etiology: Unknown triggering mechanism;
Destruction of diffuse connective tissues; Affects multiple body
systems; Autoimmune; Great imitator
Assessment Findings: Signs and Symptoms
Clinical signs; Facial rash; Behavioral disturbances; Fluid retention;
Proteinuria; Hematuria; Many others
Diagnostic Findings: Presenting symptoms; Blood tests; Renal
biopsy; Urinalysis
Etiology
The precise reason for the abnormal autoimmunity that
causes lupus is not known.
Inherited genes, viruses, ultraviolet light, and drugs may all
play some role.
What is drug-induced lupus?
Dozens of medications have been reported to trigger SLE;
however, more than 90% of this "drug-induced lupus" occurs as a
side effect of one of the following six drugs: hydralazine (used for
high blood pressure), quinidine and procainamide (used for
abnormal heart rhythm), phenytoin (used for epilepsy), isoniazid (
used for tuberculosis), d-penicillamine (used for rheumatoid
arthritis). These drugs are known to stimulate the immune system
and cause SLE.
Criteria used for diagnosing SLE:
Molar rash (over the cheeks of face) “butterfly rash
Discoid skin rash: patchy redness that can cause scarring
Photosensitivity: skin rash in reaction to sunlight exposure
Mucus membrane ulcers: ulcers of the lining of the mouth, nose or
throat
Arthritis: two or more swollen, tender joints of the extremities
Kidney abnormalities: abnormal amounts of urine protein or
clumps of cellular elements called casts
Pleuritis/pericarditis: inflammation of the lining tissue around
the Heart or lungs, usually associated with chest pain with
breathing
Brain irritation: manifested by seizures (convulsions) and/or
psychosis
Blood count abnormalities: low counts of white or red blood
cells, or platelets
Immunologic disorder: abnormal immune tests include anti-DNA
or anti-Sm (Smith) antibodies, falsely positive blood test for
syphilis, anticardiolipin antibodies, lupus anticoagulant, or
positive LE prep test
Treatment
There is no permanent cure for SLE.
The goal of treatment is to relieve symptoms and protect organs
by decreasing inflammation and/or the level of autoimmune
activity in the body.
Many patients with mild symptoms may need no treatment or
only intermittent courses of anti - inflammatory medications.
Damage to internal organ(s) may require high doses of
corticosteroids in combination with other medications that
suppress the body's immune system.
Scalp and Hair Disorders: Seborrhea,
Seborrheic Dermatitis, Dandruff
Pathophysiology, Etiology: Pityrosporum ovale
Assessment Findings: Signs and Symptoms
Oily hair; Red or scaly patches on scalp; White flakes from hair;
Itching
Diagnostic Findings: Laboratory blood work; Skin biopsy
Medical Management: Medicated shampoos; Corticosteroids
Nursing Management
Alopecia
Pathophysiology, Etiology: Alopecia areata; Androgenetic alopecia
(male pattern baldness)
Assessment Findings: Signs and Symptoms
Thinning hair
Diagnostic Findings: Determined by suspected physical disorder
Medical, Surgical Management: Treating the underlying medical
disorder; Drug therapy; Hair replacement surgery; Hair grafting;
Scalp reduction; Skin flap transfer
Nursing Management
Patterns of Hair loss
Head Lice
Pathophysiology, Etiology: Transmitted through direct contact
Assessment Findings: Signs and Symptoms
Itching of scalp; Small, yellowish-white ovals (nits) attached to
hair shafts; Small grey nymphs; Silvery eggs (nits) attached to
hair shafts
Diagnostic Findings: Scalp, hair inspection
Medical Management: Pediculicides; Mechanical removal
Nursing Management
Head Lice
Head Lice
Head Lice
Nail Disorders: Onychomycosis
Pathophysiology, Etiology: Fungal infection
Assessment Findings: Signs and Symptoms
Thick, distorted;Yellow, friable nails
Diagnostic Findings: Visual inspection; Microscopic examination
Medical, Surgical Management: Prolonged systemic drug therapy;
Nail removal; Surgery
Nursing Management
Onychomycosis - fungal infection of
toenails
Onychocryptosis - Ingrown toenail
Pathophysiology, Etiology: Inherited trait; Fungal nail infections
Assessment Findings: Signs and Symptoms
Swelling; Pain; Purulent drainage; Odor
Diagnostic Findings: Physical examination
Medical, Surgical Management: Local, systemic antibiotic therapy;
Surgery
Nursing Management
Onychocryptosis
Onychomycosis and
Onychocryptosis
Both conditions usually treated by a podiatrist
May require surgery
Nursing Management: foot-soaks, wear wide shoes and loose
socks; keep feet clean and dry
INFECTIOUS
DISORDERS OF THE SKIN
Bacteria, viruses, fungi, or parasites can cause infectious
disorders of the skin.
Treatment includes topical and systemic medications.
Preventing the spread of infection to others is important.
Impetigo
Bacterial Infection- Impetigo
Impetigo : caused by the bacteria Staphylococcus aureus, (staph), and
less frequently, by group A beta-hemolytic streptococci, (strep)
Highly contagious. Spreads quickly from one part of the body to
another through scratching. It can also be spread to other people if
they touch the infected sores or if they have contact with the soiled
clothing, diapers, bed sheets, or toys of an infected person.
Such factors as heat, humidity, crowded conditions, and poor
hygiene increase the chance that impetigo will spread rapidly
among large groups.
Diagnosis
Observation of the appearance, location and pattern of sores
is the usual method of diagnosis. Fluid from the vesicles can
be cultured and examined to identify the causative bacteria.
Treatment
Uncomplicated impetigo is usually treated with a topical antibiotic
cream such as mupirocin (Bactroban).
Oral antibiotics are also commonly prescribed.
Patients are advised to wash the affected areas with an antibacterial
soap and water several times per day, and to otherwise keep the
skin dry.
Scratching is discouraged, and the suggestion is that nails be cut or
that mittens be worn—especiallly with young children.
Ecthyma is treated in the same manner, but at times may require
surgical debridement, or removal of the affected area.
Exfoliative Dermatitis
Exfoliative dermatitis is widespread scaling of the skin, often
with itching (pruritus), skin redness (erythroderma), and
hair loss. It may occur in severe cases of many common skin
conditions, including eczema, psoriasis, and allergic
reactions.
A person with erythroderma or exfoliative dermatitis often
needs hospital care or admission to an intensive-care burn
unit.
EXFOLIATIVE DERMATITIS
Localized symptoms include erythema, severe pruritis,
extensive scaling, skin sloughing.
Affects the entire body.
Chills, fever, and malaise.
Treatment includes fluids, corticosteroids, antibiotics,
medicated baths, analgesia.
Exfoliative Dermatitis
Exfoliative Dermatitis
Stevens Johnson Syndrome
Stevens Johnson Syndrome
A severe, occasionally fatal, inflammatory disease of children
and young adults
A form of toxic epidermal necrolysis in which the epidermis
separates from the dermis, leaving the client with a skin loss
similar to a second degree burn
Characterized by fever, bullae of the skin, and ulcers of the
mucous membranes of the nose, mouth, eyes, and genitalia.
May occur from a hypersensitivity reaction to drugs