Anti-Inflammatory Drugs - Macomb
advertisement

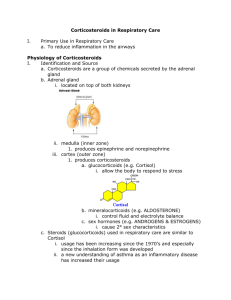
Anti-Inflammatory and Anti-asthmatic Agents MODULE F Objectives • • • • • List two mast cell stabilizers. Describe and diagram the antigen/antibody reaction on mast cells Explain which antibody is elevated in allergic asthma. List three mediators that are released with inflammation. Explain the effects of chemical mediators such as histamine and leukotrienes on airway epithelium. Objectives • • • • • • Given signs and symptoms, differentiate between the early and late phase of an inflammatory response. Describe how cromolyn sodium and nedocromil are anti-inflammatory agents. State the generic and trade names, modes of action, adverse reactions, routes of administration, dosages, and adverse reactions for cromolyn sodium and nedocromil sodium. State the origin of corticosteroid secretion. Describe why corticosteroids are now considered first line drugs in the treatment of asthma. Describe the pathway for the release and control of corticosteroids in the body. Objectives • • • • • • Define HPA insufficiency. Differentiate between systemic and inhaled corticosteroids. List three actions of steroids on inflammation. Describe the process of weaning a patient from steroids. List four side effects or adverse reactions of steroid administration. State the trade and generic names of the inhaled steroids discussed in class. Objectives • • • • • • • Describe how a RCP can decrease the incidence of oral fungal infections when administering aerosolized steroids. List three leukotrienes inhibitors discussed in class. State two side effects of leukotrienes. State how leukotrienes are administered. Describe the cellular mechanism for leukotriene production. State three medication types that are used for upper-airway congestion. State the IgE inhibitor used to treat asthma. Anti-Inflammatory Drugs • Non-Steroidal Anti-inflammatory • Mast Cell Stabilizers or anti-asthmatics • Leukotriene Antagonists (antileukotrienes) • Adrenocorticosteroid Antiinflammatory • Corticosteroids or Steroids Mechanism of Inflammation • Mast Cells, eosinophils, macrophages, basophils are found in submucosa. • The cells contain granules that are storehouses of the chemical mediators of lung inflammation. • Antigen-Antibody reactions causes the influx of Ca+2 into the cells and release of mediators. • IgE primary antibody Mechanism of Inflammation • Mediator Release • Bronchospasm • Vasodilation resulting in mucosal edema • Increased vascular permeability • Increased mucus gland secretion Mediators of Inflammation • Histamine • Platelet Activating Factor • Eosinophil Chemotactic Factor of Anaphylaxis (ECF-A) • Neutrophil Chemotactic Factor of Anaphylaxis (NCF-A) • Leukotrienes (formerly known as slow-reacting substance of anaphylaxis – SRS-A) • Prostaglandins • Explanation of Mast Cell rupture (Degranulation) • Figure 7-1, p. 132 • Mast cells are found throughout the body and their sensitization explains the watery eyes, runny nose, etc. that accompanies an allergic reaction. Phases of Inflammatory Response in Asthma • Early phase - Immediate • Late phase – 6 to 8 hours after exposure Early Phase • • • • • • • • Local vasodilation Increased vascular permeability Redness Bronchoconstriction Wheezing Coughing Dyspnea Hypoxemia Late Phase • Effect of WBC (lymphocyte) and other mediators • Hypersecretion of mucus and mucosal swelling • Traffic Jam • Breakdown of Mast Cell releases Arachidonic Acid • Production of leukotrienes • Prostaglandin FIGURE 7-2, page 134 Goal of Therapy • Stop Mast Cell from degranulating • Prophylactic Anti-asthmatics • Stop specific inflammatory processes • Corticosteroids • Broad spectrum response • Leukotriene Inhibitors • Antihistamines • Prostaglandin Inhibitors Mast Cell Stabilizers • Prevent Ca+2 influx into the cell, thereby preventing mediator release. • cromolyn sodium • Intal, Nasalcrom • nedocromil sodium • Tilade • Ketotifen (Experimental) • Zaditen • These medications do not operate through the C’AMP system and do not stimulate b or a receptor sites • Best used in limited populations and mild asthma Indications for Mast Cell Stabilizers • Prophylactic management of Asthma. • Pre-treatment for expected exposure. • Prevention of exercise induced asthma • Allergic rhinitis • Do not use to treat an asthmatic attack cromolyn sodium (1973) • Small Volume Nebulizer • Concentration: 1% • Supplied in a 2 mL ampule (unit dose) containing 20 mg (20 mg/2 mL). • Give one ampule QID; may need to add additional diluent (2 mL may nebulize too quickly). • MDI: • 0.8 mg/inhalation • 2 inhalations QID • Ophthalmic and Nasal solutions available Hazards/Adverse Reactions • Generally well tolerated • • • • • • • Nasal congestion Throat irritation Hoarseness Dry mouth Cough Feeling of chest tightness Wheezing/Sneezing/Epistaxis • Give b2 agonist prior to administering Cromolyn nedocromil sodium (1992) • Tilade • MDI: • 1.75 mg/inhalation • 2 inhalations QID • Side Effects similar to cromolyn Adrenocorticosteroids • Secreted from the adrenal cortex. • Epinephrine secreted from adrenal medulla. • Multiple functions of medication. • Anti-inflammatory. • Orally, parenterally, aerosol. • First line drugs in the management of asthma. • Reliever and controller medication. • Given to control allergies. Adrenal Gland ADRENAL CORTEX HPA Axis • Hypothalamic Pituitary Adrenal Axis • Low blood levels of steroids. • Hypothalamus is stimulated. • Sends impulse to Anterior Pituitary Gland which stimulates Corticotropin Releasing Factor (CRF). • This stimulates the formation of Adrenocorticotropin hormone (ACTH ). • ACTH in bloodstream stimulates Adrenal Cortex to produce and release Corticosteroids. • Increases blood levels of corticosteroids. FIGURE 7-3, page 137 HPA Axis • Diurnal or Circadian Rhythm • Levels are highest around 8:00 a.m. • Off-shift workers. • Giving a patient steroids can suppress the body’s HPA axis (Body stops producing steroids). • If you stop the added steroids abruptly, the patient will experience HPA insufficiency and death can occur. HPA Insufficiency • Once adrenal suppression has occurred, the patient must be weaned slowly from systemic steroids. • This will allow for recovery of the body’s own secretion. • HPA insufficiency begins 1 day after use of systemic steroid administration. Prevention of HPA Insufficiency • Low dose steroid for 5 days or less. • Take steroids in the morning when natural levels are high. • High dose tapered regimen lasting 5-6 days. • Alternate day therapy. Buffalo Hump & Moon Face FIGURE 7-5, page 139 Cushing's Syndrome • Increased secretion of corticosteroids caused by a tumor of the adrenal glands • Cushingoid appearance • Central obesity • Moon face • Buffalo hump Aerosolized Steroids • Advantage is that aerosolized steroids do not increase the blood levels of steroids • Does not cause HPA insufficiency • Less side effects • Goal is to try to gain control of asthma with the aerosolized steroids • May take 4-8 weeks for maximum improvement Oral vs. Aerosol Corticosteroids Common Inhaled Steroids Page 140 Adverse Reactions of Aerosolized Steroids • Fungal Infections may occur after aerosol • Rinse mouth and use spacer • Throat irritation, hoarseness, dry mouth and coughing have occurred • HPA insufficiency may occur during transfer from systemic to aerosol steroids • Severe asthma may occur following withdrawal of oral/IV steroids Adverse Reactions/Precautions • Aerosolized steroids may not be adequate to control asthma during periods of stress and systemic administration may be necessary Leukotriene Modifiers Anti-Leukotrienes Leukotriene Antagonists Leukotriene Inhibitors Leukotriene Inhibitors • Indications • Prophylactic treatment of asthma • “Controllers” • Not to be used to treat an asthma attack • zileuton • Zyflo • zafirlukast • Accolate • montelukast • Singulair Leukotriene Inhibitors • zileuton (Zyflo) • • • • • 12 years of age or older Works well in aspirin-sensitive asthmatics 600 mg orally QID Elevate liver enzymes Interaction with • • • • Warfarin Seldane Theophylline Propanolol • 5 - Lipoxygenase inhibitor Leukotriene Inhibitors • zafirlukast (Accolate) • • • • 12 years of age or older 10 or 20 mg orally BID Elevates liver enzymes Interactions • Warfarin • Theophylline • Blocks the leukotriene receptor site (leukotriene receptor antagonist) Leukotriene Inhibitors • montelukast (Singular) • Daily dosing • 4 mg packet of granules (6 to 23 months ) • 4 mg chewable tablet or 4 mg packet of granules (2 to 5 years of age) • 5 mg chewable tablet (child) • 10 mg tablet (adult) • Side effects: headache, influenza, abdominal pain • Blocks the leukotriene receptor site (Leukotriene receptor antagonist) Disadvantage of Antileukotrienes • Inhibit one mediator pathway • Asthma involves multiple mediators • 50 – 70% of patients respond to the medication • Trial & Error Upper Airway Congestion • Allergic Rhinitis • Antihistamine • Prevents release of histamine. • Significant side effects • Newer generation are more “forgiving” • Intranasal Medications • Mast Cell Stabilizers (Nasalcrom) • Nasal Steroids • Decongestants • a-adrenergic agents • Vasoconstriction • Table 7-14 (page 140) ciclesonide Omnaris IGE Inhibitors • omalizumab (Xolair) Dosing • http://www.xolair.com/hcp/dosing_calculato r2.jsp