CORTICOSTEROIDS
advertisement

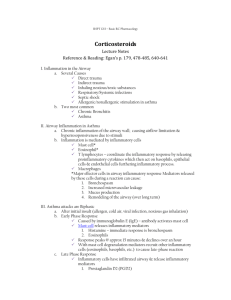
Corticosteroids in Respiratory Care I. Primary Use in Respiratory Care a. To reduce inflammation in the airways Physiology of Corticosteroids I. Identification and Source a. Corticosteroids are a group of chemicals secreted by the adrenal gland b. Adrenal gland i. located on top of both kidneys ii. medulla (inner zone) 1. produces epinephrine and norepinephrine iii. cortex (outer zone) 1. produces corticosteroids a. glucocorticoids (e.g. Cortisol) i. allow the body to respond to stress b. mineralocorticoids (e.g. ALDOSTERONE) i. control fluid and electrolyte balance c. sex hormones (e.g. ANDROGENS & ESTROGENS) i. cause 2° sex characteristics c. Steroids (glucocorticoids) used in respiratory care are similar to Cortisol i. usage has been increasing since the 1970’s and especially since the inhalation form was developed ii. a new understanding of asthma as an inflammatory disease has increased their usage II. The Hypothalamic-Pituitary-Adrenal Axis a. Sequence of glucocorticoid secretion i. Stimulation of the hypothalamus causes impulses to be sent to the median eminence 1. Injury 2. Disease 3. Exercise 4. Hypoglycemia (hunger) ii. Corticotropin releasing factor (CRF) is released from the median eminence iii. CRF circulates through the portal vessel to the anterior pituitary gland iv. Adrenocorticotropic hormone (ACTH) is released from the anterior pituitary gland into the bloodstream v. ACTH stimulates the adrenal cortex to secrete glucocorticoids (Cortisol) b. Function of Glucocorticoids i. Regulation of metabolism to increase blood glucose for energy 1. carbohydrates 2. fats 3. proteins ii. Lipolysis iii. Redistribution of fat stores iv. Breakdown of tissue protein stores III. Hypothalamic-Pituitary-Adrenal Suppression With Steroid Use a. When the body produces endogenous glucocorticoids, there is a normal feedback mechanism within the HPA axis to limit production i. As glucocorticoid levels rise, release of CRF and ACTH is inhibited, and further production is stopped ii. Similar to the way a thermostat regulates room temperature b. The body can’t distinguish between endogenous and exogenous corticosteroids. c. Administration of exogenous steroids can cause a decrease in the production of endogenous steroids called adrenal suppression d. Adrenal suppression begins after one day of systemic administration and is significant after one week i. This is a problem because if exogenous steroids are stopped suddenly, it takes a few days for the natural HPA cycle to start up again ii. The body is unable to deal with stresses 1. this is called adrenal shutdown a. nausea b. dizziness c. fatigue d. weakness e. salt craving e. If systemic exogenous steroids have been administered long enough to cause adrenal suppression, they cannot be stopped abruptly f. Three strategies have been developed to administer corticosteroids without causing adrenal shutdown i. Wean patients off systemic steroids with a tapered dose ii. Administer oral steroid therapy QOD 1. Adrenal glands are not suppressed iii. Use inhaled steroids 1. there is little or no systemic absorption, so no adrenal suppression 2. cannot abruptly switch from oral to inhaled steroids a. the oral dose must be tapered IV. The Diurnal Steroid Cycle a. The production of the body’s own glucocorticoids follows a rhythmical cycle, termed a diurnal or circadian rhythm b. There is a daily rise and fall of levels in the body i. Cortisol levels are normally highest in the morning at about 8:00 a.m. ii. During the day plasma levels gradually fall and are lowest at around midnight iii. “Jet Lag” and the delay in adjusting to night shift is caused by the inability of the body to quickly adjust the levels to the new time zone Nature of the Inflammatory Response One of the major therapeutic benefits of exogenous glucocorticoids (steroids) is for their anti-inflammatory action I. Inflammation a. The response of vascularized tissue to injury i. Increased vascular permeability 1. exudate in surrounding tissues ii. Leukocytic infiltration 1. movement of white blood cells to the area iii. Phagocytosis 1. WBCs and macrophages ingest and process foreign material such as bacteria iv. Mediator cascade 1. release of chemical mediators of inflammation II. Inflammation in the Airways a. Inflammation can occur in the lungs due to: i. direct trauma 1. gun-shot wound 2. stabbing ii. indirect trauma 1. blunt chest injury iii. inhalation of noxious or toxic substances 1. chlorine gas 2. smoke iv. respiratory infections v. systemic infections causing septic shock 1. ARDS vi. chronic bronchitis vii. asthma 1. allergic 2. non-allergic b. Inflammation in Asthma i. See text, page 214, figure 11-4 ii. Asthma is a disease in which there is chronic inflammation of the airway wall, causing airflow limitation and hyperresponsiveness to a variety of stimuli iii. The airway inflammation is mediated by inflammatory cells 1. mast cells 2. eosinophils 3. T lymphocytes 4. macrophages Inflammation in the lungs results in 5. bronchospasm 6. increased mucus secretion 7. mucosal edema (swelling of the airways) iv. Symptoms of asthma 1. wheezing 2. dyspnea 3. coughing 4. chest tightness Corticosteroids Agents I. Systemic (oral and IV) a. Prednisone b. Methylprednisolone (Solu-medrol) c. Cortisone d. Hydrocortisone II. Corticosteroids Available for Inhalation Drug Beclomethasone dipropionate Triamcinolone acetonide Flunisolide Fluticasone propionate Budesonide Fluticasone propionate / Salmeterol Brand Name Beclovent Vanceril Azmacort AeroBid AeroBid-M Flovent Flovent Rotadisk Pulmicort Turbuhaler Pulmicort Respules Advair Diskus Formulation MDI MDI MDI MDI DPI DPI SVN DPI Pharmacology of Corticosteroids I. Mode of Action a. Inhibit many of the cells involved in airway inflammation b. Reduce the number of mast cells in the airways c. Inhibit plasma exudation d. Inhibit mucus secretion II. Effect on White Blood Cell Count a. Reduces the accumulation of neutrophils at inflammatory sites and increases the number in circulation i. Causes an overall increase in the white blood cell count b. Reduces the number of monocytes, basophils and eosinophils i. Asthmatics who would otherwise have a higher than normal eosinophil count will have a low count after initiation of steroids c. Constrict the microvasculature to reduce leakage of cells and fluids into inflammatory sites III. Effect on ß Receptors a. Restore responsiveness to ß-adrenergic stimulation i. Increase the number of ß2 receptors ii. Increase the affinity of the receptors for ß-agonists b. Effect is seen 1-4 hours after IV administration c. IV bolus is given in status asthmaticus for this effect Hazards and Side Effects of Steroids I. Side effects seen with systemic administration a. These effects are caused by the high levels of circulating glucocorticoids caused by exogenous administration as compared to normal endogenous levels i. H-P-A suppression ii. Immunosuppression 1. Increased risk of infection iii. Psychiatric reactions 1. Insomnia 2. Mood changes 3. Manic-depression 4. Schizophrenia iv. Cataract formation v. Myopathy of skeletal muscle vi. Osteoporosis vii. Peptic ulcer viii. Fluid retention ix. Hypertension x. Increased WBC count xi. Dermatologic changes 1. Thinning of the skin xii. Redistribution of subcutaneous fat 1. Cushingoid appearance a. central obesity b. hump back c. moon face xiii. Growth restriction xiv. Increased glucose levels II. Side effects seen with inhaled aerosol a. Oropharyngeal fungal infection i. Caused by the immunosuppressive properties of steroids ii. Common organisms 1. Candida albicans (thrush) 2. Aspergillus iii. Treat with topical antifungal agents iv. Prevention 1. use reservoir device 2. rinse mouth after use b. Dysphonia i. Hoarseness ii. Change in voice quality c. Cough d. Bronchoconstriction III. Precautions a. Cannot switch from oral or IV to inhaled without tapering i. not enough systemic absorption b. Not indicated for acute asthma attack i. Steroids don’t treat bronchospasm c. Inhaled steroids may be inadequate during times of increased stress (infections) i. may need systemic steroids d. Incorrect use of metered dose inhaler can prevent adequate amount of drug delivery Clinical Application of Aerosol Steroids I. Use in Asthma a. Acute episodes i. inhaled steroids are not of use in acute episodes ii. IV large bolus for status asthmaticus with follow up drip or oral 1. fairly slow action, but given ASAP so antiinflammatory effects start sooner 2. may help in ER by enhancing ß2 effects of sympathomimetic drugs like albuterol iii. Chronic Asthma 1. inhaled steroids are first line drugs for maintenance of mild, moderate and severe asthma 2. these patients may need a dose pack of oral steroids periodically for infections or other stresses a. dose pack i. a packet of oral steroids with specific instructions for tapering off (e.g. take 4/day for two weeks, then 3 per day for two weeks, etc) 3. for chronic asthma, use in the following order a. inhaled b. qod oral c. daily oral 4. Oral steroids are usually the last drug to try and first to discontinue in treating asthma due to side effects II. Use in Chronic Obstructive Pulmonary Disease (COPD) a. regular treatment with inhaled glucocorticosteroids is appropriate for symptomatic COPD patients with an FEV1 < 50% predicted (Stage III: Severe COPD and Stage IV: Very Severe COPD) and repeated exacerbations i. This treatment has been shown to reduce the frequency of exacerbations and improve health status ii. Inhaled glucocorticosteroid combined with a long-acting ß2-agonist is more effective than the individual components b. Long-term treatment with oral steroids is not recommended in COPD i. Steroid myopathy contributes to muscle weakness, decreased functionality and respiratory failure in patients with advanced COPD ii. Oral steroids may be used intermittently for times of stress Androgenic (Anabolic) Corticosteroids I. Testosterone a. endogenous sex hormone secreted by adrenal cortex in both men and women (less in women) b. produces secondary male sexual characteristics, including increase in muscle mass (anabolic effects). c. Derivatives have been developed which minimize masculinizing effects and maximize anabolic effects II. Medical Uses a. Treatment of anemia i. increases RBC production b. hypogonadism i. stimulates sexual development III. Use by Athletes a. controversial due to many side effects b. increase body weight and mass i. increase performance, endurance and strength