The Primary Care Consultation
and Sexual Health
Aims of today
•
•
•
•
•
Why is it important?
Overcoming barriers
Assessing risk
Reducing risk
Scenarios
Which symptoms might be caused
by a STI
• Vaginal/urethral
discharge
• Dysuria
• Abdominal pain
• Conjunctivitis
• lymphadenopathy
• Pharyngitis
• Weight loss
• Post-coital bleeding
•
•
•
•
•
•
•
•
Uveitis
Seborrhoeic dermatitis
Arthritis
Aortic regurgitation
Diarrhoea
Pelvic pain
Genital ulcer
Flu-like illness
Which symptoms might have a
cause other than a STI
• Vaginal/urethral
discharge
• Dysuria
• Abdominal pain
• Conjunctivitis
• lymphadenopathy
• Pharyngitis
• Weight loss
• Post-coital bleeding
•
•
•
•
•
•
•
•
Uveitis
Seborrhoeic dermatitis
Arthritis
Aortic regurgitation
Diarrhoea
Pelvic pain
Genital ulcer
Flu-like illness
Beware!
50-80% chlamydia is
assymptomatic
What are the risk factors for STIs
•
•
•
•
•
•
•
<25
Single
2 or more sexual partners in the last 6 months
No condoms
Sexual orientation
City dwellers
Ethnicity
How is Primary Care different from
GUM?
Not everyone is at risk of an STI
Patients may not see themselves as being at risk
Patients may not expect questions about sex
They come with several unrelated problems
What are the barriers to taking a
sexual health history
• Patients accompanied
• Under 16
• Patient may not want to
talk about it.
• Fear of inclusion on
records
• Fear of others seeing
records
• May not be on the
patient’s agenda
• Clinician anxiety or
embarressment
• It will take too long…
• Patient doesn’t see
themselves at risk
Why is it important?
• Being assymptomatic doesn’t stop
transmission
• May not be recognised as STI if symptoms are
mild or unrelated to the genital area
• Untreated STI’s have serious consequences
When is it appropriate to talk
about STI risk?
•
•
•
•
•
New patient registration
Contraception
Pre- IUD/IUS
Travel clinic
Any symptoms which are suggestive of an STI
If we don’t ask, they won’t tell
What are your barriers to talking
about sexual health in a
consultation?
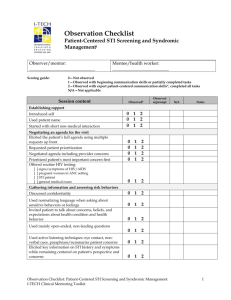
PRINCIPLES OF DOING A SEXUAL
RISK ASSESSMENT
WHO IS AT RISK?
•
•
•
•
•
•
•
•
Youth
Sexual inexperience
Beliefs system
What patients believe about you
What you believe about patients
Time
Unsure what to say
????
Reasons for doing a risk
assessment
If no apparent risk
stops unnecessary tests
If at risk
increases positivity
More specific education
Repeat testing if new risk
good management of positive results
“so you’re in a stable relationship
aren’t you?”
General
•
•
•
•
•
•
•
•
Be matter of fact
Practice some scripts
Consider the patient’s beliefs & barriers
Work with the patient so that decisions are
collaberative
Counsel patients appropriately
Maintain confidentiality
Be non-judgmental
Seek their consent to explore furhter
Move to a shared understanding
Does the patient think they are at risk?
Do you think they are at risk
Raising the issue out of the blue
In the symptomatic patient
An STI is one possible diagnosis of many
Make it clear that you do not know if the patient
is at risk until you have established their risk
“ sometimes people who present with
symptoms like this may have a sexually
transmitted infection. Would it be OK if I asked
you a few questions to see if you might be at
risk?”
Out of the blue
- The assymptomatic patient
Depersonalise & routine
• “ as part of our contraception checks, we
normally ask patients if they might be at risk
of a sexually transmitted infections so that we
can offer appropriate testing. Would it be OK
if I asked you a few questions to see if you are
at risk?”
Share knowledge
“As you’re probably aware, Chlamydia is a
common sexually transmitted infection in
people of your age.
Would it be OK if I asked you a few questions to
see if you might be at risk?”
Accompanied patients
1. 18 year old girl with her friend
2. 15 year old girl with her mother
3. 17 year old girl with mild learning difficulties
with her mother
Accompanied patients
“ I need to ask some quite sensitive questions
which are easier if you are by yourself. Would it
be OK if your friend/partner/spouse waited
outside?”
Remember
Not everyone is at risk……
…….but some are.
We won’t know an individual’s risk if we don’t
ask.
Partner history
•
•
•
•
Do you have a sexual partner at the moment?
Is that a man/woman/both?
How long have you been together?
Have you or your partner had any other
partners in that time?
• When was the last time you had sex?
HIV questions
• Have you ever had a sexual partner who
comes from another country? Which country?
• Have you ever wondered if any partners were
at risk of HIV?
Avoid apportioning blame
“ if a result is positive, it doesn’t tell us where
the infection came from – just that the infection
is in the relationship.
Many infections can cause no symptoms and
you have both had previous partners, so all we
can say is that at some point it has been
introduced into the relationship.”
Condom use
• Do you use a condom?
• Do you always use a condom?
• Have you ever had problems using condoms?
Don’t make assumptions
May be appropriate to explore additional risks
– sex with those overseas
– internet contacts
– overseas travel
– ivdu
– sex workers
– Specific sexual practices
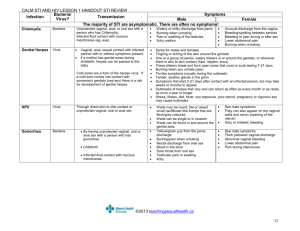
THE INFECTIONS
Chlamydia
Women
• Symptoms
–
–
–
–
–
80% asymptomatic
PCB/IMB
Purulent vaginal discharge
Lower abdominal pain
Dysuria
• Signs
– Normal
– Cervicitis, muco-purulent
discharge
– Local complications eg
Bartholin’s cyst
Men
• Symptoms
–
–
–
–
–
>50% asymptomatic
Urethral discharge
Dysuria
Testicular/epididymal pain
Proctitis
• Signs
– Normal
– Urethral discharge
– Local complications eg
epididymitis
Chlamydia testing
• Nucleic acid amplification tests (NAAT)
replacing PCR
• Male
– First void urine vs swab
• Women
– Self-taken lower vaginal swab or endocervical
swab
Chlamydia treatment
Recommended
• Azithromycin 1g stat (assess
risk vs benefit if pregnancy
possible)
Alternative
• Pregnancy/breastfeeding
– Erythromycin 500mg for 14/7
• Alternative
• Doxycycline 100mg bd for7
days (not if
pregnant/breastfeeding)
– Erythromycin 500mg qds 7
days
– Ofloxacin 200mg bd or 400mg
od for 7 days
Patient information
• Chlamydia is sexually transmitted
• Often assymptomatic, but left untreated has
potentially serious complicaitns
• Need to see and treat sexual partners
• Abstain from intercourse, until completion of
therapy or 7 days after azithromycin
• Need to complete treatment
• Advice on safer sexual practice
Do I need to retest?
Not pregnant
Routine test of cure are not indicated in >25’s
Pregnant/ Rx with erythromycin
5 weeks after Rx or 6 weeks if given erythromycin
Under 25’s
Gonorrhoea
Men
• Symptoms
– Urethral infection-85%
symptomatic within 10 days
– Rectal infeciton – 80%
assymptomatic
– Pharyngeal infection – 90%
assymptomatic
Women
• Symptoms
– Cervical infection
assymptomatic – 50%
• vaginal discharge –50%
• lower abdo pain <25%
– Rectal infection- 80%
assymptomatic
– Pharyngeal infeciton – 90%
assymptomatic
Men
• Mucoid-> purulent urethral
discharge
• Meatitis
• Non- genital signs
– eg rectal discharge,
pharymgitis,
– Disseminated infectino
Women
• Cervicitis
• Mucoid -> purulent
discharge
• Cervical excitation
• Signs PID
• Non genital signs
Tests
Men
• Urine
– First pass urine for NAAT
• Urethral swab
• Self taken LVS
– for NAAT
• Endocervical swab – NAAT
& culture
Treatmetn
Onward referral to GUM
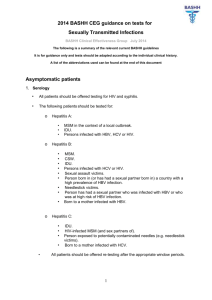
HIV
Why screen?
•
•
•
•
•
•
33% patients in Cumbria present late
Incidence rising in heterosexual population
HIV is a treatable disease
Early treatment improves length & quality of life
Reduction of onward transmission
Reduction in vertical transfer
Medical benefits outweigh negatives eg life insurance
Approx third of HIV positive patients
are unaware they are positvie
Many are attending GP surgeries and
not being offered appropriate tests
HIV
related
Asymptomatic illnesses
Acute infection –
sero-conversion
AIDS
defining
illness
Death
Window period to seroconversion
• Modern tests will detect majority of infected
individuals at one month
• A negative result at 4 weeks post exposure is
reassuring
• Further test at 12 weeks
Common presentaitons
• Sero-conversion
– `50-80% of patients develop self-limiting flu-like
illness, sometimes with a rash 2-4 weeks after
infection
HIV risk history approached sensitively may help
identify those at greatest risk
• Symptomatic HIV disease
– “weight loss and sweats”
– “cough and SOB”
– “intractable skin conditions eg seborrhoeic
dermatitis, eczema, psoriasis
– HIV associated conditins
Key to diagnosis is clinical suspicion based on risk
factors, so we need to be asking about possible risk
of HIV
2008 guidelines
•
•
•
•
•
Patients with an STI
Sexual partners of those known to be positive
MSM and female sexual contacts
IVDU’s
People from countries of high prevalence, people
who have sex with individuals from high
prevalence
• Those who present with a health problem likely
to be HIV related
Guidelines for screening
•
•
•
•
•
Be confident!
Have a script ready
HIV is treatable illness
Risk assessment of susceptible groups
Explain how result will be given
Over to you