The Last 24 Hours of Life
advertisement
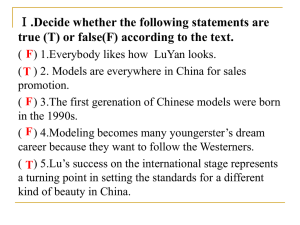
The Last 48 Hours of Life James L Hallenbeck, MD Assistant Professor of Medicine, Stanford University Director of Palliative Care Services, VA Palo Alto HCS Topics to Discuss Signs and Symptoms in Last 48 hours Coaching of Family A physician’s checklist Death Pronouncement Self-assessed Knowledge Rating Study N=27 Most physicians lack knowledge about the physical changes of dying On a scale of 1-5, the mean self-assessed knowledge rating of interns on physical changes of dying was 1.70 The lowest score of 6 items rating clinical expertise Hallenbeck and Bergen, 1999 J. Palliative Medicine N=100 Cancer pts. Signs of Impending Death Respiratory Secretions (Death rattle) Median time PTD 23h (82h SD) Respirations with mandibular movement Time PTD 2.5h (18h SD) Cyanosis/mottling Time PTD 1.0h (11 SD) Lack of radial pulse Time PTD 1.0h (4.2 SD) Morita 1998 Symptoms and Signs in the Last 24-48 Hours • • • • • • • • • • • Symptom Noisy, moist breathing Urinary incontinence Urinary retention Pain Restlessness, agitation Dyspnea Nausea, vomiting Sweating Jerking, twitching Confusion Percent 56 32 21 42 42 22 14 14 12 08 N = 200 cancer patients in hospice Lichter and Hunt, 1990 Differences Between Cancer and Non-Cancer Diagnoses Cancer Pain 40-100% Dyspnea 22-46% More predictable dying trajectory Non-Cancer Pain ~ 42% Dyspnea ~ 62% Less predictable dying trajectory Sense/desire Family loss Coaching Hunger Nurturing Other ways to nurture Mouth moist Thirst Nurturing Speech Communication Can still hear… Vision Being seen Hearing Being heard Touch Physical presence May be conscious Can still feel… Transition to ‘non-physical’ relationship Terminal Syndrome Characterized by Retained Secretions Lack of cough Multi-system shut-down Not always associated with dyspnea Vigorous hydration may flood lungs Deep suctioning is generally ineffective Role of IV and antibiotics is controversial Physician Checklist Treatment Switch essential medications to non-oral route Stop unnecessary medications, procedures, monitoring Evaluate for new symptoms Pain, dyspnea, urinary retention, agitation, respiratory secretions Family: Contact, engage, educate, facilitate relationship with dying patient, console Yourself Bear witness Death Pronouncement Death – not a difficult diagnosis No need for “pupil exam, assessment for pain” Pronouncement – more than a set of bureaucratic tasks – a cultural ritual Rarely modeled by senior staff or attending physicians Teachable skills exist Death Pronouncement Skills Anticipate impending death and prepare family If called, inquire re circumstances family present/not, anticipated/not If family present, assess ‘where they are’ Already grieving or need ritual to believe person has died ‘Sacred silence’ Console Next steps Self-care Death Pronouncement by Phone Avoid if possible Identify where recipient of news is home, on freeway, alone or not Often, like bad news, ‘advance alert’ Slow recipient DOWN, NOT – “you must come right in away” Identify contact person at hospital “Ask for Dr. … or Nurse … Summary “Don’t worry, you will all die successfully!” Sogyal Rinpoche If there is a sacred moment in the life-cycle, other than a birth, it is a death As with a birth, families will long remember, how a person died and how we helped or did not We need to re-learn how to coach patients and families through their last 24 hours