final days - harlos - Canadian Virtual Hospice
advertisement

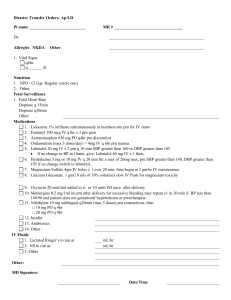
THE FINAL DAY(S) Keeping the Promise of Comfort Cancer Stroke Post-99 Ischemic Encephalopathy Discontinued Dialysis End-Stage Lung Disease • Bedridden • Can’t clear secretions Pneumonia Dyspnea, Congestion, Agitated Delirium NeuroDegenerative Main Features of Approach to Care • Perceptive and vigilant regarding changes • “Proactive” communication with patient and family » anticipate questions and concerns » available » don’t present “non-choices” as choices • Aggressive pursuit of comfort • Don’t be caught off-guard by predictable problems Patient Care Challenges in the Final Days • Functional decline- transfers, toileting • Can’t swallow meds- route of administration • Terminal pneumonia » dyspnea » congestion » agitated delirium • Concerns of family and friends Concerns of Patients, Family, and Friends • How could this be happening so fast? • What about food & fluids? • Things were fine until that medicine was started! • Isn’t the medicine speeding this up? • Too drowsy! • Too restless! • We’ve missed the chance to say goodbye • What will it be like? How will we know? Functional Decline difficult transfers bedridden completely dependent increasingly drowsy comatose Which Came First.... The Med Changes or the Decline? Steady decline Accelerated deterioration begins, medications changed Rapid decline due to illness progression with diminished reserves. Medications questioned or blamed The Perception of the “Sudden Change” When reserves are depleted, the change seems sudden and unforeseen. However, the changes had been happening. Melting ice = diminishing reserves Day 1 Day 2 Day 3 Final Family / Friends Wanting to Intervene With Food and / or Fluids • distinguish between prolonging living and prolonging dying • parenteral fluids not needed for comfort • pushing calories in terminal phase does not improve function or outcome • “We can’t just let him die” “Not letting him die” implies that you can “make him live”, which is not the case. The living vs. dying outcome is dictated by the disease, not by what you or the family decides to do. Time that death would have occurred without intervention Patient’s Lifetime Extending the final days in terminal illness: Prolonging life or prolonging the dying phase? Consider the rationale of trying to prolong life by adding time to the period of dying OBTAINING SUBSTITUTED JUDGMENT You are seeking their thoughts on what the patient would want, not what they feel is “the right thing to do”. PHRASING REQUEST: SUBSTITUTED JUDGMENT “If he could come to the bedside as healthy as he was a year ago, and look at the situation for himself now, what would he tell us to do?” Or “If you had in your pocket a note from him telling you that to do under these circumstances, what would it say?” Usual response is for comfort care only; emphasize then that we have no right to do otherwise. TALKING ABOUT DYING “Many people think about what they might experience as things change, and they become closer to dying. Have you thought about this regarding yourself? Do you want me to talk about what changes are likely to happen?” First, let’s talk about what you should not expect. You should not expect: – pain that can’t be controlled. – breathing troubles that can’t be controlled. – “going crazy” or “losing your mind” If any of those problems come up, I will make sure that you’re comfortable and calm, even if it means that with the medications that we use you’ll be sleeping most of the time, or possibly all of the time. Do you understand that? Is that approach OK with you? You’ll find that your energy will be less, as you’ve likely noticed in the last while. You’ll want to spend more of the day resting, and there will be a point where you’ll be resting (sleeping) most or all of the day. Gradually your body systems will shut down, and at the end your heart will stop while you are sleeping. No dramatic crisis of pain, breathing, agitation, or confusion will occur - we won’t let that happen. Basic Medications in The Final Day(s) SYMPTOM Pain Dyspnea Secretions Restlessness MEDICATION Opioid Opioid Scopolamine Haloperidol + Midazolam or Lorazepam Methotrimeprazine National Hospice Study Dyspnea Data Reuben DB, Mor V. Dyspnea in terminally ill cancer patients. Chest 1986;89(2):234-6. • n = 1764 • prospective • Dyspnea incidence: 70 % during last 6 wks. of life National Hospice Study Dyspnea Prevalence Prevalence of Dyspnea (%) 75 Reuben DB, Mor V. Dyspnea in terminally ill cancer patients. Chest 1986;89(2):234-6. 65 55 45 35 # Days Prior to Death 25 42 21 7 HOW WELL ARE WE TREATING DYSPNEA IN THE TERMINALLY ILL? Addington-Hall JM, MacDonald LD, Anderson HR, Freeling P. Dying from cancer: the views of bereaved family and friends about the experience of terminally ill patients. Palliative Medicine 1991 5:207-214. • n = 80 Last week of life • severe / very severe dyspnea: 50% less than ½ of these were offered effective treatment Basic Medications in The Final Day(s) 1. Opioid - pain, dyspnea 2. Antisecretory - congestion 3. Sedative - restlessness, confusion Examples of Opioid Prescription / Orders In Absence of a Protocol Example 1 Morphine 5 - 20 mg po/SL/pr q4h. - Start with 5 mg dose. Titrate or by 5 mg . - Breakthrough = the current q4h dose given q1h prn. Example 2 Hydromorphone 0.5 - 2 mg/hr IV/SQ sage. - Start with 0.5 mg/hr. Titrate or by 0.1- 0.2 mg/hr - Breakthrough = the current hourly dose q30 min prn. Sedation in Delirium if No SQ Route Available or if Not Necessary Mild: haloperidol 0.5 – 2 mg po or (injectable) SL bid + q6h prn OR risperidone 0.5 – 1 mg po bid plus q6h prn OR methotrimeprazine (elixir or injectable) 6.25 – 12.5 mg po/SL q6-8h + q4h prn [NB:Taché Pharm. makes 40mg/ml elixir) Moderate: methotrimeprazine 12.5 - 25 mg po/SL OR haloperidol 2.5 - 5 mg po/SL +/- q4h plus q1h prn lorazepam 1 - 2 mg SL Severe: methotrimeprazine 25 - 50 mg po/SL OR haloperidol 5 mg po/SL AND lorazepam 2 mg SL q4h plus q1h prn (Also consider chlorpromazine supps 50 - 100 mg pr q4h) Sedation via SQ Route in Delirium Mild: haloperidol 0.5 - 2 mg SQ bid OR methotrimeprazine 6.25 – 12.5 mg SQ 6 - 12h Moderate: haloperidol 2.5 - 5 mg OR methotrimeprazine 25-50mg + SQ q4h plus q1h prn midazolam 2.5 - 5 mg Severe: haloperidol 5 mg OR methotrimeprazine 50mg + SQ q4h plus q1h prn midazolam 10 – 20 mg OR: SQ infusion of: methotrimeprazine 6.25 - 12.5 mg/hr + midazolam 1.25 - 5 mg/hr CONGESTION IN THE FINAL HOURS “Death Rattle” • Positioning • ANTISECRETORY: Scopolamine 0.3 - 0.6 mg SQ q1h prn Transdermal Gel (Taché Pharm.) 0.25 mg/0.1ml Give 0.5 mg q4h and q1h prn. Try 2-3 Transderm-V® Patches • Consider suctioning if secretions are: distressing, proximal, accessible not responding to antisecretory agents A COMMON CONCERN ABOUT AGGRESSIVE USE OF OPIOIDS IN THE FINAL HOURS How do you know that the aggressive use of opioids doesn't actually bring about or speed up the patient's death? SUBCUTANEOUS MORPHINE IN TERMINAL CANCER Bruera et al. J Pain Symptom Manage. 1990; 5:341-344 100 90 80 Pre-Morphine 70 Post-Morphine 60 50 40 30 20 10 0 Dyspnea Pain Resp. Rate (breaths/min) O2 Sat (%) pCO2 Typically, with excessive opioid dosing one would see: • pinpoint pupils • gradual slowing of the respiratory rate • breathing is deep (though may be shallow) and regular COMMON BREATHING PATTERNS IN THE FINAL HOURS Cheyne-Stokes Rapid, shallow “Agonal” / Ataxic DON’T FORGET...For death at home • Advance Directive: no CPR • Letters (regarding anticipated home death) to: » Funeral Home » Office of the Chief Medical Examiner » Copy in the home • physician not required to pronounce death in the home, but be available to sign death certificate