Advance Care Planning
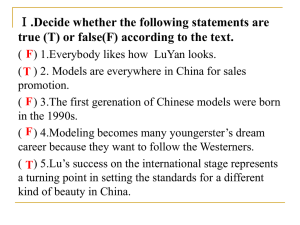
advertisement
Dying with Dignity Advanced Care Planning and Patient Rights and Advocacy Margo Holland & Gregory Robinson January 2013 Welcome and Introduction • • • • Allan to introduce and house keeping Overview of the Day (schedule) Safe Space Contract Objectives Safe Space Contract • • • • • • • • • • Confidentiality Step up; Step back Not a therapy group Passing is permitted Active Listening Respect diversity and value our differences I will not interrupt Listen and speak from our heart Take care of yourself, be gentle and break if needed Others? • And, The Quiet Room (to take a breath and ponder when needed) Objective of Workshop • • • • Educate Provide skills and tools Clarify Terms Create your own Advanced Directive Video Presentation • Speak Up Video (CHPCA Front page online Speak Up Video – YouTube) • Advance Care Planning Conversations (CHPCA video – YouTube) • You may also wish to listen to “Do Not Resuscitate”, With Dr. Brian Goldman, While Coat Black Art. (noting the importance of having thought out an Advanced Directive before tragic illness strikes) • www.cbc.ca/whitecoat/popupaudio.html?clipIds =2313383178 Can you describe or tell a story about a difficult death experience you may have lived through, witnessed or heard about? • Can you describe or tell a story about a good death experience you may have lived through, witnessed or heard about? Dying with Dignity 5 Critical Planning Steps There is much more to writing an Advance Care Plan than simply filling in a form. The most important part of the planning process is to take time for reflection and discussion to ensure your Plan reflects your values, beliefs and wishes. Step 1 Understand all Your Choices. Step 2 Reflect and Discuss Step 3 Make Your Decisions Step 4 Document Your Decisions Step 5 Communicate Your Decisions and review yearly Small Group Discussions • What are some of the circumstances, health conditions, and interventions (medical treatments) that we see at the end of life? • What choices do we have for care at end of life? • What would you wish to have happen at the end of your life? • Can you create a list of a few principles for “A Good Death”? Sample ADP DWD • Walking through DWD’s Advanced Directive • Case Example for this: 67 year old with terminal cancer; less than a few months to live; relentless nausea and vomiting (early bowel obstruction); excruciating abdominal pain not relieved by narcotics or other pain medications • Home at this point with husband of 42 years Patient Rights and Advocacy Dying with Dignity While the wording of the applicable legislation varies by province, in general, as a Canadian you have the following rights and options: • Right to be Fully Informed of all Treatment Options • Right to have Advance Care Directives Recognized • Right to have Substitute decision-maker recognized • Right to Change Doctors • Right to Discontinue/Refuse Treatment. • Right to refuse Cardiopulmonary Resuscitation (CPR) • Right to Refuse Food and Drink (VSED) • Right to end your own life Video Presentation • DWD Blog – Aimee Doolittle (DWD video online – YouTube) • Australian clip on choice (DWD Site)/Banned Euthanasia Ad http://www.dyingwithdignity.ca/watch/index.ph p Patient Rights and Advocacy • • • • First do no harm! When to use? To do what? How to accomplish and with whom? Patient Advocacy Scenarios 1) ICU setting - intubation of comatose post trauma young patient (doctor/wife); 2) Intractable pain from cancer at the end of life (palliative care nurse/son [daughter])* 3) Home care patient dying of AIDS with family stretched to cope (family doctor/lover [parent?])* 4) Someone dying of a neuromuscular disease who wishes assisted dying [doctor/friend (patient has no supports for care)] *Note: jointly vs. independently appointed SDM Closing and Wrap Up • Final thoughts (Margo) • Evaluation (Margo) NUMBERS COUNT! YOUR VOICE FOR CHOICE IS CRITICAL! WORKSHOP EVALUATION 1. 2. 3. 4. 5. 6. 7. 8. 9. Where did you hear about this session? For you, what was the most valuable part of the workshop? Was the content or information sharing for this workshop what you expected? How was the process and flow to the day for you? Can you provide feedback about the roles of the facilitators? On a scale of 1 (lowest) to 5 (highest) this presentation met my expectations: Improvements I would suggest are: What other seminars/topics on death and dying would you like to see presented? Do you have any other comments? Thank-you You can make a difference in your own unique way.