hand – foot – mouth disease
advertisement

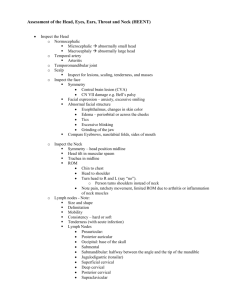
HAND – FOOT – MOUTH DISEASE Prepared by: Dr. NGUYEN QUANG DIEN Emergency Department HAND – FOOT – MOUTH DISEASE HFM disease is a viral syndrome with a distinct exanthem – enanthem. This clearly recognizable syndrome is characterized by vesicular lesions on the mouth and an exanthem on the hands and feet (and buttocks) in association with fever. HAND – FOOT – MOUTH DISEASE The lower lip has an ulcer with an erythematous halo. The tongue has an ulcer with an erythematous halo. A typical cutaneous lesion has an elliptical vesicle surrounded by an erythematous halo. The long axis of the lesion is oriented along the skin lines. HAND – FOOT – MOUTH DISEASE Pathophysiology Hand-foot-and-mouth disease is caused by a group of RNA viruses called enteroviruses. The most commonly implicated enterovirus is coxsackievirus A16.[1] However, coxsackieviruses A5, A9, A10, A16, B1, and B3; human enterovirus 71 (HEV71); as well as herpes simplex viruses (HSV) can cause the illness. HEV71 is of the most care because HEV71 has been recently implicated in several large outbreaks with severe complications and deaths. Pathophysiology Cases are commonly spread via the fecal-oral or oral-oral route. Respiratory droplet transmission also may occur but is less likely. Typically, the virus seeds the GI tract via the buccal mucosa or the ileum. Over the next 72 hours (accounting for the incubation period), a viremia is established via spread through nearby lymph nodes. In Vietnam , the peak incident is in April & May . HAND – FOOT – MOUTH DISEASE Mortality/ Morbidity Severe complications may occur when CNS or cardiopulmonary involvement is present . Age More common among infants and children younger than 5 years. History The usual incubation period of hand-foot-and-mouth (HFM) disease is 4-6 days. The prodrome is associated with the following: Low-grade fever Malaise Anorexia Abdominal pain Sore mouth The prodrome precedes the development of oral lesions, followed shortly by skin lesions, primarily on the hands and feet and occasionally on the buttocks. Physical Hand-foot-and-mouth disease is the most common cause of mouth sores in pediatric patients. Physical Yellow ulcers surrounded by red halos characterize the oral lesions These primarily occur on the labial and buccal mucosal surfaces but may be observed on the tongue, palate, uvula, anterior tonsillar pillars, or gums. Unlike herpetic gingivostomatitis, perioral lesions are uncommon. Coxsackie A virus also causes herpangina, mostly described as palatal and posterior oropharyngeal lesions without any associated exanthem. The oral ulcers are painful. Children younger than 5 years are predominately more symptomatic than older patients. Physical The exanthem typically involves the dorsal surfaces but frequently may include the palmar, plantar, and interdigital surfaces of the hands and feet. These lesions may be asymptomatic or pruritic. They usually begin as erythematous macules that rapidly progress to thick-walled grey vesicles with an erythematous base. In young infants, these lesions may also be observed on the trunk, thighs, and buttocks. The rash is usually self-limited, lasting approximately 3-6 days. Case reports have documented subacute, chronic, and recurring skin lesions. Complications Neurologic complications : 1. Encephalitis aseptic : Wake up with a start Myoclonal jerk Limbs trembling Nystagmus Cerebellar ataxia Transverse myelitis >> limbs weakness 2. Cranial nerves paralysis 3. Convulsion , coma coupled with respiratory failure , cardiovascular failure . Complications Cardiopulmonary complications: Pulse > 150 bpm , mottled skin , capillary refill > 2s BP : normal or increasing RR increasing , laboured breathing , rose froths , wet rales Cyanosis Diagnosis Positive : Clinical exam. is the cornerstone with Exanthem – Enanthem ( oral ulcers & skin lesions ) Diagnosis Severity degrees : 1. Buccal ulcers +/- skin lesions : recovery in 01 week , no sequelae 2. Encephalomyelitis risk: Myoclonal jerk , restlessness , hands reaching up repeatedly , flounder . Diagnosis Severity degrees : 2a/. Less starts : not found on exam. 2b/. More starts : > 2times / min or found on exam, frequent starts coupled with : Hands reaching up repeatedly Trembling Flounder Somnolence P> 150bpm Fever > 39 dC not relieved Limbs weakness / paralysis Diagnosis Severity degrees : 3. Diaphoresis , RR increasing , P > 170bpm , BP increasing , convulsion , coma (glasgow <10) 4. Respiratory failure , Cardiovascular failure. TREATMENT : Symptomatic treatment Close monitoring Complications treatments Early sedations >> decreasing irritation >> treat increased ICP TREATMENT I – Outpatient: (stage 1st and 2nd a ) Fever relief Oral higiene Recs immediately if : Fever >39dC Laboured breathing Starts , trembling , crying , hands reaching up repeatedly Convulsion , coma Limbs weakness Mottled skin Rest and prevent irritation Recs everyday or every other day in 7 days TREATMENT II – Admission: ( Degree 2b backwards ) if meet one of following criteria: Fever : < 3yos : > 38dC w/o time mentioned >=3yos : > 38dC and > 3 days HR : < 3yos : > 150 bpm >= 3yos : > 120bpm RR : < 3yos : >40 / min >= 3yos : > 30/min TREATMENT II – Admission: ( Degree 2b backwards ) if meet one of following criteria: Any of : Signs of : ○ Refuse to eat ○ Meningitis ○ Vomiting all the time ○ Myocarditis ○ Fatigue ○ Encephalitis ○ Mottled skin ○ Acute limbs weakness / ○ Look bad . paralysis Indications for Immunoglobulin at Peadiatric N.1 Hospital: Neurologic Complications: Mental status disorder : Glasgow<10. Frequent starts , restlessly exciting . Neurologic deficit (limbs weakness / paralysis, cranial nerves paralysis). Convulsion (febrile convulsion ruled out). Indications for Immunoglobulin at Peadiatric N.1 Hospital: Cardiorespiratory complications : Abnormal RR (rapid RR , Irregular RR , and no pneumonia signs / chest Xray ). Pulmonary Edema . Tachycardia, HR >150 bpm, Capillary refill > 2 s. HTN. Immunoglobulin is not effective in severe shock, deep coma THANKS FOR YOUR ATTENTION! Dr NGUYEN QUANG DIEN