Cryptococcus neoformans
advertisement

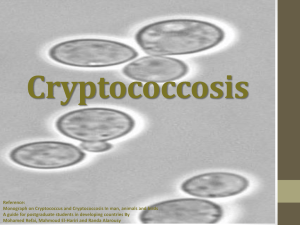
Cryptococcus neoformans and other Yeast Dr Sharon Walmsley University Health Network Toronto Organism • Encapsulated • Heterobasidiomycetous fungi • Asexual stage – simple narrow based budding • Sexual – bipolar system, in-vitro • 19 species Identification • • • • Routine laboratory media 48-72 hours, 30-35ºC May be inhibited by cycloheximide White/cream opaque colonies which become mucoid with prolonged incubation Rapid identification • India ink • Urease test (ureaammoniapH) • Laccase activity (diphenolic compoundsmelanin) – niger seed agar Rapid Urease Test Histopathology • • • • Prominent capsule Spherical narrow based budding yeast May have hyphae or pseudohyphae 5-10 mm diameter • 4 serotypes based on capsule Ecology • Saprobe in nature – fruit, trees, rotting wood, soil • Bird guano – pigeons, turkey, chickens Epidemiology • • • • • • • • • • • • HIV Lymphoproliferative disroders Sarcoidosis Corticosteroids Hyper IgM or IgE syndrome Monoclonal antibodies (infliximab) SLE CD4 T-cell lymphoma (idiopathic) Diabetes Organ transplant Peritoneal dialysis Cirrhosis • 20% without HIV have no underlying comorbidity Spectrum of Disease Colonization Asymptomatic Disease Rates of Disease Pre-AIDS 1992 HAART Africa/HIV .8/10 6/ year 5/10 6/year 1/10 6/year 15-45% Rates in Transplant • 18/100,000 • Increased with cell mediated immune inhibitors • Highest in kidney and liver • Rarely carried in through transplanted organ Serotypes - Cryptococcus neoformans • • • • A-D Commercially available antibody tests Biochemical tests PCR Serotypes - Cryptococcus neoformans Serotype A – 80% clinical cases B – tropical, subtropical – S. California, Hawaii, Brazil, Australia, SE Asia C – rare D – Europe – Denmark, Germany, Italy, France, Switzerland Pathogenesis • Inhalation • Traumatic inoculation • Human – human – contaminated transplant tissue • Zoonosis? Pathogenicity • Capsule – polysaccharide • Melanin • High temperature growth (37ºC) Host Response • Cellular immune response, granulomatous inflammation • Th – 1 polarized • Cytokines – TNF, 1F-8, 1L-2 • Proinflammatory 1L-12, 1L-18, MCP-1, MIP • NK cells Pathogenesis Host defense Size of Inoculation Virulence of strain Clinical Manifestations Lung - Portal of entry - asymptomatic (1/3) life threatening pneumonia (ARDS) - Endobronchial colonization underlying chronic lung disease - Single pulmonary nodule - Symptomatic – acute, subacute Pulmonary Cryptococcus Clinical Manifestations CNS - Subacute meningitis or meningo-encephalitis - Headache, fever, cranial nerve palsies, lethargy, coma - Subacute (days) months HIV - Higher yeast burden - incidence raised intracranial pressure - Often disseminated - Immune reconstitution disease Cryptococcal meningitis Cryptococcus- Oral Lesions Clinical Manifestations Skin - Papule with ulcerated center - Cellulitis, abscess - Rarely underlying bone lesions Prostrate - Asymptomatic (sanctuary) - Penile, vulvar lesions Cryptococcus, skin lesions Cryptococcus, skin lesions Clinical Manifestations Eye - Ocular palsy, papilledema, optic neuritis - Retinal exudates +/- iritis - endophthalmitis Diagnosis Microscopic – – – – India Ink (50-80% + CSF) Gram Calcoflur white Silver stain Culture – Blood agar – Routine blood culture Cryptococcus, India Ink Diagnosis Serology – Latex agglutination, EIA, 90% sensitive & specific Radiology – CXR – infiltrates, nodules, lymphadenopathy, cavitation, effusion – CT/MRI – 50% normal, hydrocephalus, nodules In vitro susceptibility testing • Low MICs – amphotericin, flucytosine, azole • High MICs – caspofungin • In vitro R demonstrated but most refractory cases are relapses Therapy – Cryptococcal meningitis • Amphotericin B +/- flucytosine • Fluconazole • Amphotercin x 2 wk then fluconazole 400800 mg/d x 8-10 wk • Chronic suppression fluconazole 200 mg/d Raised ICP • • • • CSF OP > 250mm Rapidly progressive cerebral edema Repeated LP, shunt Corticosteroids not useful Prognosis • Need to be able to control underlying disease – – – – immunosuppression prednisone HAART ? Adjunctive cytokines – interferon, GCSF Poor prognosis Burden of organism ( + India Ink, crypto Ag > 1:1024, poor CSF inflammatory response < 20 cells/uL) Sensorium Mortality 10-25% Prevention • Fluconazole prophylaxis • Active immunization- cryptococcal GXMtetanus toxoid conjugate vaccine- in animal models, no human trials • Monoclonal antibodies- would require repeated injections • Avoid high risk environments Cryptococcus neoformans (var gattii) • Initially described in Australia • Cultured from vegetation around river red gum trees, eucalyptus trees • Recent outbreak Vancouver Island Cryptococcus neoformans var gatti • Outbreak Vancouver Island, January 02 • N = 59, 2 deaths Cryptococcus neoformans var gatti • • • • • • • 75% primarily pulmonary disease 25% CNS 58% male, 5.3% Asian Mean age 60 Certain geographic locations Never cultured from bird guano May be associated with certain trees Cryptococcus neoformans Cryptococus neoformans var grubii var gatti (now C.gatti) var enoformans C.gatti Vancouver Island • 1999-2003 – 8.5 – 37/10⁶/year • Australia - endemic – 94 cases/million/year C.gatti • • • • Usually restricted to tropical, subtropical Now in temperate zone Able to identify an environmental reservoir Identified in sea animals Cryptococcus • • • • • • • Global epidemiology Study – Canada 1984 N = 78 7.7% C.gatti 79.5% C.neoformans v grubii 6.4% C.neoformans v neoformans (serotype D) 6.4% C.neoformans v neoformans (hybid AD)