Histology of GIT I & II
advertisement
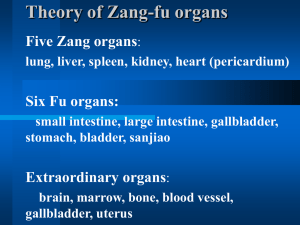
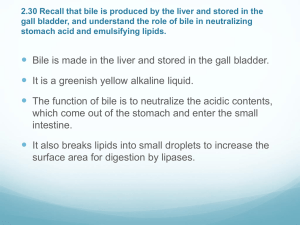
Histology of GIT II PROF. DR. FAUZIAH OTHMAN DEPT OF HUMAN ANATOMY FPSK Content Histology of the: - spleen - pancreas - liver & extra hepatic biliary apparatus spleen Spleen spleen posses only efferent lymphatic vessels. Spleen is surrounded by a capsule of dense connective tissue from which emerge trabeculae, which divide the parenchyma/splenic pulp, into incomplete compartment. Splenic pulp Has two compartment 1 white pulp( white spot; lymphoid nodules) 2.red pulp (dark red tissue, red blood cells) White pulp consist= periarterial lymphatic sheath and the lymphoid nodules. Red pulp consist= splenic cords (Billroth’s cords) & blood sinusoids. Spleen Red Pulp: Clusters of Macrophages and Red Blood Cells. White Pulp: Lymphocytes suspended on reticular Fibers The spleen is a fist-sized, spongy organ located behind the stomach (removed in this illustration), just under the diaphragm. Part of the lymphatic system, the spleen is composed of two types of tissue. White pulp produces lymphocytes, which release antibodies into the bloodstream to combat infection. More prominent is the red pulp, in which macrophages filter broken cells, parasites, bile pigments, and other useless substances from the blood. Iron from broken red blood cells is stored in the spleen for later use. Despite this variety of functions, an injured or diseased spleen can be removed in adults without great consequence. Spleen, flattened, oblong organ that removes disease-producing organisms and worn-out red blood cells from the bloodstream. The spleen is situated in the upper left abdominal cavity, in contact with the pancreas, the diaphragm, and the left kidney. It is supported by bands of fibers that are attached to the peritoneum (the membrane lining the abdominal cavity). The spleen varies in size but, in adult humans, it is about 13 cm (about 5 in) long, up to 10 cm (4 in) wide and 3.8 cm (1.5 in) thick, and weighs about 200 g (about 7 oz). The spleen is fed by the splenic artery, and venous blood from the spleen enters the liver. The spleen removes iron from the hemoglobin of red blood cells for use in the body. It also removes such waste materials as bile pigments for excretion as bile by the liver. The spleen produces antibodies against various disease organisms and manufactures a variety of blood cells. In some mammals (but not in humans) it stores red blood cells and feeds them into the circulation to maintain the volume of blood in cases of hemorrhage. In the unborn child, the organ functions primarily to produce red blood cells, a function that is normally taken over by the bone marrow after birth. However, if diseases slow down this function in the bone marrow, the spleen may again start to produce red blood cells. Pancreas Both endocrine (pancreatic islets of Langerhans – secretes insulin & glucagon) & exocrine gland (pancreatic acini – secretes pancreatic juice) Stomach Tail Body Under a microscope, stained sections of the pancreas reveal two different types of parenchymal tissue.[2] Lightly staining clusters of cells are called islets of Langerhans, which produce hormones that underlie the endocrine functions of the pancreas. Darker staining cells form acini connected to ducts. Acinar cells belong to the exocrine pancreas and secrete digestive enzymes into the gut via a system of ducts. Structure Appearance Function Islets of Langerhans Lightly staining, large, spherical clusters Hormone production and secretion (endocrine pancreas) Pancreatic acini Darker staining, small, Digestive enzyme berry-like clusters production and secretion (exocrine pancreas) Pancreas Small cluster of glandular epithelial cells= Acini A distinction between the two glands can be made based on the absence of striated ducts and the presence of the islets of Langerhans in the pancreas. Another characteristic detail is that in the pancreas the initial portion of intercalated duct penetrate the lumens of the acini. Nuclei, surrounded by a pale cytoplasm, belong to centoacinar cells that constitute the intraacinar portion of the intercalated duct. These cells are found ONLY in pancreatic acini Functions of Liver Storing glycogen (fuel for the body) which is made from sugars. Helping to process fats and proteins from digested food. Making proteins that are essential for blood to clot (clotting factors) Processing many medicines which you may take; helping to remove poisons and toxins from the body The liver also makes bile. This is a greenish-yellow fluid which contains bile acids, bile pigments and waste products such as bilirubin. Liver cells pass bile into bile ducts inside the liver. The bile flows down these ducts into larger and larger ducts, eventually leading to the common bile duct. The gallbladder is like a 'cul-de-sac' reservoir of bile which comes off the common bile duct. After you eat, the gallbladder squeezes bile back into the common bile duct and down into the duodenum (the first part of the gut after the stomach). Bile in the gut helps to digest fats. Liver & extra hepatic biliary apparatus Lobules comprised of rows of Hepatocytes arranged radially around a central vein Hepatocytes surround blood sinusoids (capillary structures) which are partially lined with phagocytic Kupffer cells ( stellate reticuloendothelial). Gallbladder The gallbladder is a sac located under the liver. It stores and concentrates the bile produced in the liver Gallbladder The wall of the gallbladder -mucosa that is composed of a simple columnar epithelium of absorptive cells and a lamina propria, a thin irregular layer of smooth muscle cells (responsible for the contraction and expulsion of the stored bile in response to cholecystokinin), a well developed perimuscular connective tissue layer, and the serosa. The mucosa is extensively folded when the gallbladder is contracted and modestly folded when it is relaxed. However, it does not contain villi or tubular glands (crypts). The underlying connective tissue is richly vascularized. A tall columnar epithelium modified for absorption. The cells have an apical brush border through which water and ions are absorbed. Cholecystitis Inflammation of the gallbladder wall and nearby abdominal lining. Cholecystitis is usually caused by a gallstone in the cystic duct, the duct that connects the gallbladder to the hepatic duct. Symptoms of Cholecystitis intense and sudden pain in the upper right part of the abdomen recurrent painful attacks for several hours after meals pain (often worse with deep breaths and extends to lower part of right shoulder blade) Nausea Vomiting rigid abdominal muscles on right side slight fever chills jaundice - yellowing of the skin and eyes. itching (rare) loose, light-colored bowel movements abdominal bloating How is cholecystitis diagnosed? 1. 2. 3. Ultrasound (Also called sonography.)Endoscopic retrograde cholangiopancreatography (ERCP) Computed tomography scan (CT or CAT scan) -