Randomised Clinical Trial: Lactobacillus
reuteri DSM 17938 vs. Placebo in Children
With Acute Diarrohea
Aliment Pharmacol Ther 2012:36 (4):363-369
R. Francavilla et al
16th July 2013
Shamshad Shah
Question
Is there clinical evidence supporting the therapeutic effects
of probiotics in children with acute diarrhoea?
Background
• Viewed from a global perspective gastroenteritis in
children is of great public health importance
• The use of ORT contributed to a marked reduction in
death rates globally
• In developed countries 30% hospital admissions for
gastroenteritis due to rotavirus
• Probiotics are live micro organisms which when
administered in adequate amounts confer a health
benefit to the host
• Cochrane review; 56 trials concluded specific probiotics
reduce duration diarrhoea 24 hours and frequency stools
Literature Search
[clinical trial]
AND [diarrhoea]
AND [probiotics]
AND [children].
Limited to [child 0 – 36 months AND English
language]
Aim of Study
• To test the efficacy and safety of a new strain
Lactobacillus reuteri DSM 17938 derived from L reuteri
ATCC 55730 in children with acute diarrhoea
• Primary outcomes were the rate of unresolved diarrhoea
after 3 days of treatment and duration of diarrhoea.
Event Title If Required (Change Text in Footer)
Method
• Children 6 – 36 months old were recruited from
3 wards across 3 hospitals in S Italy from
Jan –July 2009
• Diagnosed with acute diarrhoea with clinical
signs dehydration
• Randomised to receive in a double blind fashion
either L reuteri or a placebo
• Symptoms were recorded in a diary 1 week
Method
Inclusion Criteria
• Children 6-36 months old hospitalised with acute
diarrhoea
• Clinical signs of mild to moderate dehydration
• No clinical features of hypovolaemic shock
Event Title If Required (Change Text in Footer)
Method
Exclusion criteria
• Included underlying chronic disease
• Bloody stools at first examination
• Current use of probiotic/antibiotics
• Demonstration of bacterial cause for diarrhoea
• Use of parenteral rehydration.
Event Title If Required (Change Text in Footer)
Method
• Approved by ethics committee
• Randomly assigned to receive either L reuteri or placebo
• All enrolled children were entered sequentially to receive
the assigned treatment
• First dose was given immediately after informed consent
• The study preparation was administered for 7 days
• At start of treatment stool sample to test for rotavirus
/adenovirus was collected
• Dehydration was corrected in line with WHO
recommendations
Event Title If Required (Change Text in Footer)
Method
• The active L reuteri and placebo preparation were based
in mixture of sunflower oil and MCT
• Both mixtures were presented in same shaped bottles
• Dose 5 drops bd administered by nurse
• Study was blinded for investigators and patients
• Group assignments were concealed from participants
and investigators
• Codes were revealed after the study
Event Title If Required (Change Text in Footer)
Outcome Measures
Primary Outcomes
• The rate of unresolved diarrhoea after 3 days
treatment
• Duration of diarrhoea
Secondary outcomes
• Duration of hospitalisation
• Total intake of oral rehydration solution
Statistics
• Calculated a sample of 34 children per group required
for study to have 80% power with a type 1 error =0.05
(two tailed test)
• Assumption is based on similar trials (references not
quoted)
• SPSS
• Variables were tested for normal distribution and
compared using Mann-Whitney U test
• Intention to treat analysis was performed
• Statistical significance accepted at p<0.05
Event Title If Required (Change Text in Footer)
Results
•
•
•
•
•
•
•
•
96 children enrolled
Out of 64 children
10 children prompt recovery
43 children identified with rotavirus
10 children identified with adenovirus
11 children – no aetiology found
Baseline characteristics similar in both groups
L reuteri significantly reduced the duration of watery
diarrhoea compared with placebo p<0.03
• Effect of L reuteri mostly seen day 2 or 3 of treatment
Event Title If Required (Change Text in Footer)
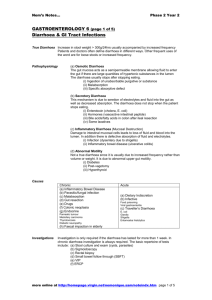
Enrolled Assigned Intervention and Follow up
% patients with persisting watery diarrhoea in the groups
receiving placebo (grey) and L reuteri (white)
Conclusion
• L reuteri is efficaceous and safe alongside rehydration
therapy shortening the duration and reducing stool
frequency in acute infectious diarrhoea in young children
Event Title If Required (Change Text in Footer)
CASP RCT Appraisal Tool
Event Title If Required (Change Text in Footer)
Are the results of the trial valid?
Did the trial address a clearly
focused issue?
An issue can be 'focused' in terms of
- the population studied
- the intervention given
- the comparator given
- the outcomes considered
Yes
PICO
Was the assignment of patients to
treatments randomized?
Yes randomly assigned to receive
L reuteri or placebo
Were all of the patients who entered
the trial properly accounted for at
its conclusion
Was follow up complete?
Were patients analysed in groups to
which they were randomised?
Yes 27 children became ineligible
due to non compliance or refused
to participate or had commenced
antibiotics
Clinical Question
Population
Children under 3 years old with
acute infectious diarrhoea
Intervention
Probiotic L reuteri DSM 17938
and ORT
Comparison
A placebo and ORT
Outcome
Reduce duration and stool
frequency in acute infectious
diarrhoea.
Detailed Questions
Were patients, health workers and
study personnel ‘blind’ to
treatment?
- were the patients
- were the health workers
Yes
Study was blinded for
investigators and patients
- were the study personnel
Were the groups similar at the start
of the trial?
In terms of other factors that might
effect the outcome such as age, sex,
social class
Aside from the experimental
intervention, were the groups
treated equally?
Results are reported on
those that completed the
trial not the number
recruited
Not specifically stated
What are the Results?
How large was the treatment effect?
Not stated numerically in paper
What outcomes are measured?
NNT 10 people
Experimental Event Rate 40%
Control Event Rate
50%
Absolute Risk Reduction 10%
How precise was the estimate of the No confidence limits reported
treatment effect?
P< 0.03
What are its confidence limits?
Will the results help locally?
Can the results be applied to the local
population?
Do you think that the patients covered
by the trial are similar enough to your
population?
Applicable to local
community
Were all clinically important
outcomes considered?
Yes
If not, does this affect the decision?
Are the benefits worth the harms and
costs?
This is unlikely to be addressed by the
trial. But what do you think?
Cost ORT £2.52 for 20
sachets
Cost Biogaia £11.10 bottle
Cost LF formula £12 /week
Discussion
• Results relevant to Biogaia .Conflict of Interest ?
• Small sample size but strong power 80% and no
confidence intervals quoted – reliable recommendation
to change practice in hospital setting?
• If used in primary care setting would it reduce hospital
admissions and costs?
• Would a shorter duration of diarrhoea episode prevent
secondary lactose intolerance?
• Subgroups needed 6-12 months & 13-36 months?
• Unable to compare results with other studies (probiotics
species specific in each study)