Parturition and Foal
Neonatal Care
LACP pg. 163
Gestation Length
Average 335-340
days.
Variable- breed,
season, sex of foal,
plane of nutrition, fetal
genotype
Equine Gestation Hormones
Progesterone/Progestogens
Progesterone initially rises, followed by a slight ↓ then ↑ to a peak at d 80,
then gradually ↓ to 1-2 ng/ml during mid-late gestation (d 150).
Second ↑ associated with formation of accessory & secondary CL.
Late gestation progesterone rises (last month of pregnancy)
Once embryo enters uterus, it migrates
throughout the uterine body and both horns
until 16-17d (becomes to big to pass through
horn.
This migrations signals the dam that she is
pregnant. (contacts endometrial surface
repeatedly) FIXATION
Embryo – 40d
Fetus – after 40d
60d-7 months- fetus develops slowly
(fetal organ development)
8 months- increase in size to about 60% of its
weight in the last 3 months.
Placenta
Placenta takes over
progesterone production ~d
100 until foaling.
Complete placental
formation is done at 150
days.
DAY 150 - Firm
placental attachment
Placenta
Attachment of placenta to endometrium
begins around day 40 of gestation and not
complete until 120d.
Endometrial cups (day 25) fetal in orgin, form
from girdle cells, and invade the dam’s
endometrium . Forms horseshoe like ring of
white cups. Produce ECG that stimulates CL
to produce progesterone. Cups degenerate
at day 70.
Loss after day 40- no return to heat for 3-4
months.
Epitheliochorial and noninvasive (materanal
and fetal epithelium contact)
Attachement- diffuse in that the membranes
are attached to all portions of the uterus with
the exception of the cervix- no attachement
Chorioallantois- outer fetal membrane, chorionic
side attaches to dam- red and velvety, allantoic
side- fetal side bluish grey in color.
Amnion is thin, white membrane covers the fetus
Impending Birth
Vaccinate & Deworm
30 day prior
Most Obvious
Hypertrophy mammary
glands obvious from 8th
month
Maiden may display little
until just before foaling
Distention of the teats
4-6 d pre-foaling
Waxing of the teats
1-72 hrs pre-foaling
An increase in milk Ca
1-3 d pre-foaling
Fescue Toxicity
Pull mare off fescue
at least 1 month
before foaling.
(endophyte-infected)
Calcium concentration rise sharply as the time of foaling
approaches
Foaling Facilities
Stall14x14 for light mares
Disinfect between foaling
Good air circulation
Safe, solid construction
Straw bedding
Paddock“clean” grassy paddock
Safe, good fencing
Other horses?
Impending Birth
More Subtle Signs
Softening and flattening of
the muscles in the croup
Vulva becomes relaxed &
elongated. Maximal hours
before parturition
Visible changes in the
position of the foal
Vulva – thick & puffy with
edema and may elongate
Pear shaped abdomen
Stages of Parturition
Stage 1
Onset: initial uterine contractions
End: rupture of chorioallantois
(water bag “water breaks”)
2-4 hr
Mare may stand up, pacing, lie
down, roll, pace, look or bite at
flanks, sweat, frequent urination
Foal is being pushed toward the
cervix
Stages of Parturition
Stage 2
Onset: rupture of
chorioallantois (8-20L)
End: delivery of fetus- cord is
broken
Timeline 20-30 min
Contractions occur in groups
of 3-4 followed by a rest
period of 3 to 5 minutes
Forefeet visable, soles
pointing down
Oxytocin release, uterine
contractions reinforced
Ensure a clear airway by clearing
membranes and fluids from the nostrils
When the chest is
through the vulva the
foal can breathe on
its own. May go in &
remove the amniotic
sac.
Not breathing – rub
foal, take straw and
put in nose, breath
into nose
Foaling Emergencies
May Need Assistance
Red mass evident at vulva
(placenta seperation)
Strong straining & no feet evident
at vulva within 5 min
Heavy straining with feet in vulva
but no further progress in 10 min
One foot missing
No progress for more than 15 min
after first water breaks
Rectovaginal perforation occurs
Mare foals while standing
“Red Bag”
Foaling Emergencies
May Need Assistance
If the chorioallantois does not
break and the velvety-red
surface of the chorioallantois is
presented at the vulva, it should
be immediately ruptured
because this indicates that the
placenta is separating from the
endometrium and that fetal
oxygenation will be impaired
- cut placenta and pull foal (fescue
toxicity)
Stages of Parturition
Stage 3
End: passage of the fetal
membranes
Expel placenta 30minuets -4
hrs post-foaling
If no passed within 4-6 hours,
the placenta is considered to
be retained– metritis, necrotic
uterine wall, septicemia,
laminitis
Can tie placenta in knot
above hocks
•Examine Placenta
http://video.google.com/videosearch?q=horse
+breeding&hl=en&emb=0&aq=f#q=foaling&hl
=en&emb=0
Placenta Examination
•Arrange the membranes in a
capital "F" position, with the
pregnant horn uppermost and the
body forming the vertical bar of
the "F"
•Tip of the nonpregnant horn is
the most likely part of the
placenta to be retained
•Placenta Examination
•Weight
•Length of umbilical cord &
location
•Appearance of gross
lesions, missing pieces
Retained Placenta: Treatment
After 2 hrs
Oxytocin
Infusion of fluid into allantoic cavity
Antibiotics
Non-sterioidal anti-inflammatory drugs
Frog support pads
Deeply bedded stall
Abortions
No common, greater in mares over 14yrs
Twins- 90% abort,
Abortion in mid to later gestation may occur
in single horse, or many “abortion storm”
(viral or bacterial)
If this happens fetus should be placed on ice
and examined by vet within 12 hours.
Abortion time
Control
EHV
6+ mo
Vaccine
EV arteritis
6+ mo
Vaccine
Lepto
5+ mo
Isolation
Mare Repro. Loss
Syndrome
45-120d
10+ mo
Eastern Tent caterpillars
Placentitis
5-9 mo
Caslick
Umbilical torsion
Anytime
None
Twins
5+ mo
None
Stress
Anytime
Decrease stress
Endotoxemia
Anytime
Determine cause and
avoid
Postpartum Mare & Foal Care
Umbilical Cord Care
Allow foal to break fetal membranes.
Never cut the cord.
Spray or dip umbilical cord stump with antiseptic
solution 3-4X per day for 3-4 days
Ascending placentitis
Premature seperation
Umbilical cord is made of
Umbilical vein, 2 umbilical arteries, and urachus
Vein becomes the falciform ligament
Arteries become the round ligaments of the
bladder
Best to let the cord rupture naturally
Neonatal Care
The neonatal period is the period
following birth, which most clinicians
consider the first 4 to 5 days
This period is one of susceptibility to
many diseases and conditions that can
be threatening to the immediate and
long-term health of the foal
Good neonatal care is a combination of
sound management practices and
recognition of normal and abnormal
conditions
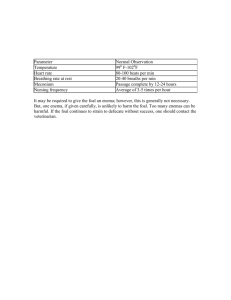
Foal Facts
Newborn foal should exhibit a suckle reflex at 20
minutes after birth, stand within 30-60 min.and
nurse within 60 to 180 min.
The first urination occurs within 10 hours and the
meconium should be passed by 24 hours after
parturition. (Meconium is the first fecal material
that the newborn foal normally evacuates. It
appears in pelleted form, brown to black in
coloration. They must pass this or become
impacted.)
LACP pg. 165
Colostrum
First milk secreted by a mare coming into
lactation (poor lactation can be supplemented
with domperidone)
Production
During last 2-4 weeks of gestation
Under hormonal influences
Importance
Transfer of passive immunity to the suckling
foal (“Liquid Gold”) Specificity of protection
achieved by vaccinating pregnant mares 30-60
days before parturition
Produced only once – beware of leakage!
Provides energy to foal
Encourages passage of meconium
Colostrum
Quality
Relates directly to antibody content
Good quality:
≥ 50 (70) g/L IgG and specific gravity > 1.060
Thick, sticky, yellow secretion
All foals should have IgG measured between 8-24 hours
Colostrum
Evaluating Colostrum Quality
When?
Assess before foal suckles
How?
Physical appearance
Thick, sticky, yellow secretion indicates good quality
Dilute, white or translucent secretion indicates poor quality
Stall Side Tests
Banking of Colostrum
Only good quality colostrum
Storage at - 20ºC:
IgG concentration stable for 12 months
Other immune components (complement, etc) and
nutritional components decrease significantly
Storage at -70ºC:
Permanent maintenance of all components
Colostrum
Evaluating Colostrum Quality
ARS Refractometer
Designed for measurement of sugar
concentration of
solutions (BRIX type)
1-2 drops of colostrum needed
Results in less than 1 minute
http://www.arssales.com/equine/html/refractometer.html
Colostrum
Evaluating Colostrum Quality
ARS Refractometer - Results
Foal Immune Status
Evaluation of serum IgG status
When?
Typically at 12-24 h after birth
Peak serum levels of IgG achieved by 18h
Absorption of immunoglobulins from small intestine essentially
complete
If failure of passive transfer: treat with IV plasma
Can measure early at 6-12 h
IgG first detected in foal’s serum at 6 h of age
If no IgG or very low level at 6-12 h: can give colostrum to
increase levels
Foal Immune Status
Evaluation of serum IgG status
Snap Foal IgG Test
ELISA
Use whole blood, serum, or plasma
Calibrator spots indicate IgG
levels of 400 and 800 mg/dl
Sample color is proportional to
IgG content
Results in 10-15 min.
Expensive but convenient
Foal Aftercare: within 1st 24 hours
Give enema to prevent Meconium
impaction
Give Tetanus antitoxin
Check for presence of suckle reflex
Check for any malformations or
deformities
Take blood sample from foal.
Perform a physical
Neglected foals
Milk can be expressed from the mammary
gland by use of an inverted 60-ml dosing
syringe to apply suction
Common Foal Diseases
Sepsis
Perinatal Asphyxia
Prematurity
Neonatal Diarrhea
Respiratory Disease
Sepsis
Common in foals
Fever, elevated heart rate, or respiratory rate
Causes: improper umbilical care, failure of
passive transfer, poor sanitation, maternal
illness such as placentitis
Treatment: intensive nursing care,
immunoglobulin therapy, antimicrobial
treatment
Perinatal Asphyxia
Lack of oxygen
“dummy foal syndrome” cerebral edema and
ischemia and necrosis of the brain
48 hours after birth foal my lose the affinity
for the mare, become unable to suckle,
wander aimlessly, and potential for seizures.
Prognosis is good if there are no seizures
Prematurity
Equal to or less then 320 days
Low birth wt, weakness, short hair coat,
increased joint motion, rear limb flexural
laxity, take longer to stand, suckle reflex may
lack vigor, domed forehead, floppy ears
Survival depends on degree of complication
Diarrhea
Common
Frequency of diarrhea, suckling of foal,
weather other foals are affected
Cause: Foal heat diarrhea, rotavirus,
coronavirus, septicemia, salmonella,
clostridium, Strondyloides westeri, lactose
intolerance.
Iv fluid therapy, probiotics, analgesics,
plasma
Respiratory Disease
Can be hard to diagnose: restlessness and
agitation, increased respiratory rate or
distress.
Diagnosis- thoracic radiograph, arterial blood
gas, pulse ox, ultrasound
Cough is rarely seen, nasal discharge
uncommon, respiratory rate and rhythm can
be unreliable, mucous membrane won’t
reflect mild to moderate pulmonary disease,
Thoracic auscultation can be misleading
Bacterial pneumonia
Viral pneumonia
Fungal pneumonia
Milk aspiration
Acute respiratory distress syndrome
Persistent pulmonary hypertension
Fractured rib
Pneumothorax
Pleural effusion
Examination of the inner ear reveals
petechiation
The critically ill neonatal foal should be
placed on a warm, well-padded surface in
semisternal recumbency
The jugular groove is widely clipped and
prepared with sterile solutions before
intravenous catheter placement
Proper restraint of the foal is achieved by
gently cradling one hand under the neck and
grasping the base of the tail with the other
hand.
Limb Deformities
Angular- Varus, Valgus, Windswept
Axial- off set knees
Rotational- muscular
Spiral- toed in
Flexor – week or contracted flexors
Most are congenital, premature, dietary, blunt
trauma to the growth plate, uneven hoof
balance
Angular
Valgus
Varus
Windswept
Treatment
Stall rest
X-rays
Medial extensions
Self correction (valgus)
Surgical correction
Therapeutic trimming
Axial- off set knees
No treatment, undesirable in race horses, can
lead to unsoundness
Rotational- toed out
Self correction
Muscular development of thoracic muscles
Spiral – toed in
Fetlock is in normal
alignment
No treatment, corrective
shoeing masks problem
Flexor- contracted
Bone is longer then the surrounding tendons
treatment
Tetraclycine- shown to relax the
muscle/tendon unit
Bandaging
Passive extension stretching
Air splints
PVC splints
surgery
Flexor- laxity
rest
Bone growth catches up with tendons
Swimming
Care for soft tissues if damaged