Placenta Accereta
advertisement
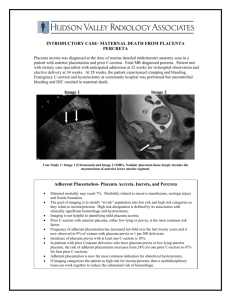
Placenta Accreta-Lessons Learnt Dr LeenaWadhwa Associate Professor ESI-PGIMSR,Basaidarapur,Delhi Maternal Mortality-Magnitude and Causes About 28 million pregnancies and 67,000 maternal deaths per year in India Other Conditions, 34% Haemorrhage, 38% Source: RGI-SRS 2001-03 Abortion, 8% Obstructed Labour, 5% Sepsis, 11% Hypertensive disorders, 5% * Other Conditions includes Anemia. Source: RGI-SRS 2001-03 Placenta accreta/ increta/ percreta Significant cause of maternal morbidity and mortality significant maternal hemorrhage at delivery Mortality rate -7 -10% (O brien et al AM J Obstet Gynecol 1996) Most common reason for emergency postpartum hysterectomy. Incidence -increasing(secondarily to the rise of Caesarean section) 1970 1/7000 1985 - 1994 1/ 2,510** 1992 - 20021/ 533 *** **(Miller- Am J Obstet Gynecol 1996 ) ***(Wu et al Am J Obstet Gynecol 2005) Case 1 Unbooked, G4P2L2A1, 26 weeks, previous LSCS, fever dysuria USG:Placenta antr,covering os Em laprotomy (GA) : hematuria ? Rupture uterus Per-operative details Hemoperitoneum (1 litre+) Posterior wall of bladder found adhered to LUS Bladder lying open (3cm) Clots presents inside the bladder removed. large bleeders present on the posterior bladder wall , clamped & sutured Case 1 hysterotomy done and fetus delivered fails to recognize percreta going into bladder & anticipate complications tries partial MRP hysterectomy with difficulty by 2 consultantsuncontrollable hgg from bladdercystectomy & B/L Int iliac art ligation 6 units Blood Patient died in ICU Case 1 HPE- Placental tissue invading the full thickness myometrium and the overlying serosa.(placenta percreta) ‘Placenta accreta mindedness’ Placenta Percreta Catastrophic event Placenta percreta induced uterine rupture as early as 9 &14 wks 75% cases of percreta are assoc with placenta previa Maternal mortality-20% Perinatal mortality-30% (Obstet Gynecol 1991) What could have been done? Anticipation Multidisciplinary team Preoperative cystoscopy and placement of ureteric stents may aid in identification of the ureters. biopsy contraindicated placement of catheters in both int iliac A Hysterectomy by postr approach Involved portion of bladder is resected with hyst specimen Case 2: G3P2L2 ( Prev 2 LSCS ) at 34 weeks of gestational age was admitted due to bleeding PV for 2 days USG-SLF cephalic ,placenta, anterior low lying covering Os With informed written consent for possibility of hysterectomy (if required)and adequate blood patient was shifted to OT for emergency caesarean section. Case 2 . Per-operative details LUS was thinned out Placenta did not separate from LUS after the delivery of baby Bleeding ++ Decision of hysterectomy taken and done Three units of BT done Post operative Uneventful HPE- Placenta Increta Have we become wiser? Management of a case where pre-operative diagnosis was made Case 3 G2P1L1 with 35 weeks and 5 days was admitted in antenatal ward in view of placenta previa with moderate anemia (no H/O bleeding PV) Obstetric history 1st FT LSCS for CPD 2 years back at govt. hospital USG(8/8/2011)-SLF 29 weeks 4 days ,placenta anterior low lying covering Os Hb-7.1 Case 3 After admission USG-Placenta anterior extending to LUS, with extensive placental lakes within. Overlying myometrium intact with no evidence of placental invasion. MRI-Myometrium grossly thinned out and placental interface with myometrium not properly visualized. Possibility of placenta accreta could not be ruled out Case 3 Elective LSCS -at 37 weeks LUS distended with increase vascularity with purple hue with boggy feeling(?placenta increta) classical CS Placenta did not separate Subtotal hysterectomy done. Bleeding from stump present. B/L Internal Iliac Artery Ligation done. 3 units of PRBC given Case 3 Post operative details Uneventful HPE-Placenta Increta. Others risk factors Major risk factor -Placenta previa with history of Caesarean section previous uterine surgery, Previous Dilatation and Curettage, Previous Myomectomy Asherman Syndrome (Endometrial defects) Submucous leiomyomata Advanced maternal age Multiparity Tobacco use Risk association : C.S. delivery 30,132 P.P 723 P.P.+ACCRETA% No P.P. ,ACCRETA% Hysterectomy First (6201) 398 13(3.3%) 2(0.03%) 40(0.65%) Second (15,808) 211 23(11%) 26(0.2%) 67(0.42%) Third (6324) Fourth (1452) Fifth (258) 72 29(40%) 7(0.1%) 57(0.90%) 33 20(61%) 11(0.8%) 35(2.41%) 6 4(67%) 2(0.8%) 9(3.49%) Diagnosis Clinical suspicion Ultrasound Color Doppler MRI Biochemical Marker Histopathology Ultrasonic features Moth eaten / Swiss Cheese appearance of placenta . Ultrasonic features Obliteration of clearspace between placenta and uterine wall Ultrasonic features Sensitivity -93% Specificity-79% Color Doppler USG Sensitivity 82-100% Specificity 92-97% Distance <1mm between the uterine serosa-bladder interface and the retroplacental vessels High velocity and turbulent (Twickler et al 2000) flow MR Imaging MRI is no more sensitive than USG for diagnosing placenta accreta* MRI is used as an adjunct to USG when there is a strong clinical suspicion of accreta** (Yinka et al 2006)*(Lax et al 2007)** Women who have had a previous CS who also have either placenta praevia or an anterior placenta underlying the old CS scar at 32 weeks of gestation are at increased risk of placenta accreta and should be managed as if they have placenta accreta, with appropriate preparations for surgery made. (RCOG 2011) Management Elective delivery by caesarean section at 34–35 weeks of gestation for suspected placenta accreta (AICOG 2012) Lessons learnt (Pre-operative) Prenatal imaging for placental location in previous CS Rule out MAP in prev. CS* with pl. previa Consent for hysterectomy Arrange sufficient blood and component therapy Consultant obstetrician , alert surgeons Lessons learnt (Intraoperative) NEVER PULL PLACENTA Resort to hysterectomy SOONER RATHER THAN LATER Uterine incision should be made vertically and above the placental insertion site. POSTOP COMPLICATION Transfusion reaction ,sepsis DIC Urinary stasis ,infection Pelvic and renal abscess formation ,Renal compromise ARDS Multi organ failure Fistula formation Ureteral stricture Uterus preserving modalities Expectant management Balloon catheterisation and embolisation of pelvic vessels Methotrexate therapy Uterus preserving surgeries (Charlotte et al, Arch Gynecol Obstet.2011)* Balloon catheterisation /SAE Pre-delivery consultation with the interventional radiology team Pre-operative placement of arterial catheters in internal iliac artery After delivery balloons are inflated to achieve temporary homeostasis Selective arterial embolization(SAE) if necessary Advantages 1. 2. 3. 4. Avoidance of hysterectomy and preservation of fertility Lower estimated blood loss Reduced blood transfusion Low frequency of complications 1. 2. Post procedure fever Pelvic infection SAE Disadvantages Illiac artery thrombosis Uterine necrosis Sepsis MODS (Gupta et al. Cochrane database Syst Rev 2006)* Infertility for succeeding pregnancy Fetal radiation exposure (Gupta et al. Cochrane database Syst Rev 2006)* Methotrexate ? controversial It acts by inducing placental necrosis & expediting a more rapid involution of placenta. MTX should be administered (1 mg/kg) on alternate days for a total of 4 to 6 doses* Methotrexate Complication Hemorrhage Disseminated intrauterine infection (sepsis) Pancytopenia Nephrotoxicity Failure Rate-22% Expectant management Few case reports A series of 7 cases * Placenta was left in situ, uterus involuted spontaneously woman returned to a normal menstrual cycle. Placenta was never expelled but was presumably absorbed. A series of 26 cases** Placenta partially removed in 19/26 4/26 conservative therapy failed (Mark Gabot et al 2010)* (Timmermans et al 2007)** Follow-up management 1.- Ultrasound exams Vascularity 2.- HCG titers 3. Daily Temps, Other S&S of infection 4.- Bleeding 5.- Coagulation profile Thank you