Mike Holden Think Pharmacy HLP presentation August 2013
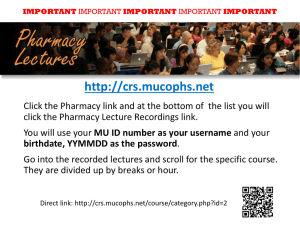
advertisement

Michael Holden FRPharmS NPA Chief Executive Pharmacy and Public Health Forum • • • • Background Healthy Living Pharmacy National Roll-out Evaluation outcomes Community Pharmacy • Over 11,000 community pharmacies in England • 99% of the population can get to a pharmacy within 20min by car • 96% by walking or using public transport • Estimated 1.6 million visits a day • Average 14 visits per year Making Every Contact Count Common Ailments Ongoing adherence support Medicines Optimisation Promotion Prevention Protection Self care & Healthy lifestyle interventions PATIENT and PUBLIC Initial supply and support Early detection Diagnosis & Treatment referral Why use pharmacy? Healthy Living Pharmacy background Pharmacy White Paper states vision for pharmacies to become Healthy Living Centres April 2008 Portsmouth develop HLP concept with support from DH, Director of Public Health and LPC Portsmouth HLPs deliver positive interim results. Minister asks can the results be replicated in differing demography and geography? National pharmacy bodies working with DH March 2011 launch pathfinder programme April 2013 Evaluation of pathfinder programme June 2009 Sept 2010 What distinguishes a Healthy Living Pharmacy? Consistently delivers broad range of high quality commissioned services Quality, innovation and productivity Proactive team ethos Health Champion Identifiable Key question Can the results seen in Portsmouth be replicated elsewhere with different demography and geography? NATIONAL ROLL-OUT National roll-out • Pathfinder Support Group – all pharmacy organisations • Generate evidence and further develop the concept • Pharmacy and Public Health Forum HLP task group • Influencing policy – – – – – NHS Plan 2010-2015 Public Health White Paper Respiratory Strategy NHS Future Forum report Public Health Workforce Development consultation Evaluation aims • Is there better uptake and delivery of services in HLPs compared to baseline (i.e. before being an HLP or against other non-HLP pharmacies)? • Does geography and demography impact on HLP performance? • What is the effect of HLP services on public-reported experiences? • What are the benefits of HLP for public, commissioner, contractor, employees? • Is each individual service delivered through HLP cost-effective? SERVICE EVALUATION Service outcomes: overall Service outcomes: stop smoking 250 Chart 2: Comparison of the number of people achieving quit before and after implementing HLP in each area 200 Number of people No. achieving quit before HLP 150 No. achieving quit after HLP 100 50 0 Birmingham Dudley Bucks Milton Keynes Area South Staffs Lambeth Sheffield Service outcomes: sexual health • Buckinghamshire: – – – – • Pre-HLP, 75% of EHC through pharmacy Post-HLP, 86% through pharmacy Increase in condom distribution by 13% Increase in Chlamydia screening discussion by 6% Stoke on Trent: – Increase in EHC consultations from 1600 to 1848 – 29% increase in chlamydia screening • East Riding and Hull – Average EHC consultations in HLP 123, non-HLP 73 – Increased condom distribution (22.6% vs. 16.1%) • Portsmouth – Average EHC consultations in HLP 160, non-HLP 85 19 Service outcomes: alcohol awareness • Dudley – 55 interventions prior to HLP; 280 after • Milton Keynes – Non-HLP 31 per pharmacy – Working towards HLP 38 per pharmacy – HLPs 59 per pharmacy • Portsmouth – Non-HLP 90 per pharmacy – HLPs 218 per pharmacy 20 Service outcomes: alcohol awareness • Pharmacy London initiative – 24,000 scratch cards – >43% high risk 21 Service outcomes: Substance misuse • Blackburn with Darwen and East Lancs – 328 interactions over 4 months • • • • 35.7% made by pharmacist 26.8% made by Health Champion 20% counter assistants 13% technicians – 60% clients signposted to other services • 34.5% to pharmacist • 10.1% to NHS dentist – 72% of advice was for needle exchange Service outcomes: Medicines Use Review Chart 8: Trend in average no. of MURs per pharmacy: HLP compared to non-HLP pharmacies (BwD & EL) Average no. of MURs per pharmacy 30.0 25.0 HLP Non-HLP 20.0 15.0 10.0 5.0 Baseline 0.0 HLPs introduced (October 2011) Service outcomes: New Medicine Service COST EFFECTIVENESS Cost effectiveness • Contractor survey gives rich insight into how PH services are delivered • Evaluation has affirmed important role of non-pharmacist staff in delivery • Clear evidence that pharmacy staff are engaged and enthused by opportunities to make a difference; potential to spill over to better service outcomes • Stop smoking services delivered by non-pharmacist staff perform at least as well as pharmacists – Service can be delivered more effectively i.e. making best use of each staff member’s skills – And more cost effectively i.e. pharmacist’s time has a higher business cost – Academic evidence shows that stop smoking services are cost effective Making optimal use of each staff member’s time, without necessarily risking ability to generate positive health outcomes, indicates the potential of service delivery in the HLP context PUBLIC REPORTED EXPERIENCES Public satisfaction (n = 1034) Were you comfortable to receive this service in the pharmacy? 99.9% Were you happy with how you were treated by the pharmacy… 99.7% Do you feel you were provided with enough information by the… 99.6% Would you recommend this service to others? 98.3% Before coming in today, had you heard of healthy living… 27.0% 0% 20% 40% 60% 80% 100% Location where service users would have sought help/advice had this service not been available in the pharmacy (n = 1034) Doctor 60.2% A&E 1.6% Walk-in Centre 5.4% Internet 3.7% I wouldn't have done anything Other (please state) 21.2% 1.3% 0% 20% 40% 60% 80% Number of service users referred to an additional service in the pharmacy (n = 1034) Smoking Weight… Alcohol… EHC Chlamydia… Condom… Sexual Health STI info Substance… Heart Healthy… Glucose check MUR Healthy drinking Advice about… NHS health… Minor Ailments Healthy eating Repeat… NMS Blood… 250 219 200 149 150 94 100 50 46 29 26 26 50 20 16 3 1 3 13 15 7 0 3 3 1 0 There were 683 referrals/recommendations into other services offered by pharmacy. Commissioners’ views • “Becoming an HLP will display to commissioners pharmacy’s commitment to delivering cost effective and high quality services” [Birmingham tPCT and Solihull] • “Future commissioning can be targeted and offered to those pharmacies that we know will deliver. So this has become a great organisational tool to target commissioning more cost effectively” [Portsmouth] • “Public health commissioners see the HLP initiative in a very positive manner, public health teams are now keen to involve community pharmacies and in particular the HLPs in their service developments. They have volunteered to give on-going training to HLCs re information and signposting” [Dudley] WHAT MADE THE DIFFERENCE? The Enablers workforce environment Quality Criteria engagement 2000+ qualified Health Champions 1400+ leadership development 500+ Healthy Living Pharmacies What next? Recommendations • • • • • • • • • • Continued local and national support and leadership Potential link with national contract Recognition of HLP status by local commissioners National consistency and quality assurance of HLP status Consideration for establishment of national awarding body National service frameworks Common performance measures including public reported experiences Resources to support pharmacists and their teams Workforce development Consideration for extending role e.g. Dementia, early detection of cancers Summary • Provides a commissioning framework • Is an organisational development tool • Is a Quality mark • Is about the pharmacy team • Has a common vision & goal • Has a brand the public can recognise • Is a means to the end