Chap 15
advertisement

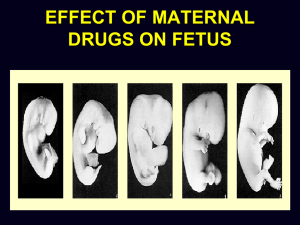
Understanding Nutrition Chapter 15 Life Cycle Nutrition: Pregnancy and Lactation By A. Fellah, Ph.D. Growth and Development During Pregnancy Placental Development: conception: the union of the male sperm and the female ovum; fertilization. Placenta: the organ that develops inside the uterus early in pregnancy, through which the fetus receives nutrients and oxygen and returns carbon dioxide and other waste products to be excreted. Uterus: the muscular organ within which the infant develops before birth. Amniotic sac: the "bag of waters" in the uterus, in which the fetus floats. Umbilical cord: the rope-like structure through which: The fetus's veins and arteries reach the placenta. The route of nourishment and oxygen to the fetus. The route of waste disposal from the fetus. The scar in the middle of the abdomen that marks the former attachment of the umbilical cord is the umbilicus, commonly known as the "belly button." Ovum: the female reproductive cell, capable of developing into a new organism upon fertilization; commonly referred to as an egg. Sperm: the male reproductive cell, capable of fertilizing an ovum. zygote: the product of the union of ovum and sperm; so-called for the first two weeks after fertilization. Implantation: the stage of development in which the zygote embeds itself in the wall of the uterus and begins to develop; occurs during the first two weeks after conception. Embryo: the developing infant from two to eight weeks after conception. Fetus: the developing infant from eight weeks after conception until term. The Placenta The placenta is a sort of pillow of tissue in which maternal blood vessels lie side by side with fetal blood vessels entering it through the umbilical cord. This close association between the two circulatory systems permits the mother’s bloodstream to deliver nutrients and oxygen to the fetus and to carry away fetal waste products. Embryonic and Fetal Development: 1 of 4 A newly fertilized ovum is about the size of the period at the end of this sentence. This zygote at less than one week after fertilization is not much bigger and is ready for implantation. Embryonic and Fetal Development: 2 of 4 After implantation, the placenta develops and begins to provide nourishment to the developing embryo. An embryo five weeks after fertilization is about 1/2 inch long. Embryonic and Fetal Development: 3 of 4 A fetus after 11 weeks of development is just over an inch long. Notice the umbilical cord and blood vessels connecting the fetus with the placenta. Embryonic and Fetal Development: 4 of 4 A newborn infant after nine months of development measures close to 20 inches in length. From eight weeks to term, this infant grew 20 times longer and 50 times heavier. Critical Periods Critical periods: finite periods during development, in which certain events occur that will have irreversible effects on later developmental stages; usually a period of rapid cell division. gestation: the period from conception to birth. For human beings gestation lasts from 38 to 42 weeks Pregnancy is often divided into thirds, called trimesters. neural tube defect: a serious central nervous system birth defect that often results in lifelong disability or death. Anencephaly: an uncommon and always fatal type of neural tube defect, characterized by absence of brain. Spina bifida: one the most common types of neural tube defects, characterized by the incomplete closure of the spinal cord and its bony encasement The Concept of Critical Periods Critical periods occur early in development. An adverse influence felt early can have a much more severe and prolonged impact than one felt later on. The concept of Critical Periods Neural Tube Development: 1 of 2 At four weeks, the neural tube has yet to close (notice the gap at the top). Neural Tube Development: 2 of 2 At six weeks, the neural tube (outlined by the delicate red vertebral arteries) has successfully closed. Successful development of the neural tube depends, in part on the vitamin folate Spina Bifida: 1 of 3 A neural tube defect. Spina Bifida: 2 of 3 Spina Bifida: 3 of 3 Folate Supplementation Rich Folate sources Weight prior to Conception Underweight: has a high risk of having a low birthweight infant. Preterm (infant): an infant born prior to the 38th week of pregnancy; also called a premature infant. Overweight: has a high risk of medical complications such as hypertension, gestational diabetes, and postpartum infections. A term infant is born between the 38th and 42nd week of pregnancy. Post term: an infant born after the 42nd week. Cesarean section: a surgically assisted birth involving removal of the fetus by an incision into the uterus, usually by way of the abdominal wall. Weight Gain during Pregnancy Recommended Weight Gains: Prepregnancy Wt. Status Underweight Normal weight Overweight Obese Recommended Wt. Gain 28-40 lb 25-35 lb 15-25 lb 15 lb minimum Weight-Gain Patterns: 3.5 lb during the 1st trimester and 1 lb per week thereafter. Components of Weight Gain During Pregnancy Energy and Nutrient Needs during Pregnancy Energy: ~300 kcalories above the allowance for nonpregnant women-and only during the 2nd and 3rd trimester. One extra serving from each of the five food groups. Protein: ~ 10 g/day higher than for nonpregnant women. Essential Fatty Acids: a diet that includes seafood has a balance of the omega-3 and omega-6 fatty acids. Folate: ~ 600µg/day. Vitamin B12: 2.6µg/day. Iron: 27 mg/day. The increased need cannot be met by diet or by existing stores. Therefore, iron supplements are recommended during the 2nd and 3rd trimesters. Common Nutrition-Related Concerns of Pregnancy Nausea: morning sickness. Constipation and Hemorrhoids. Heartburn. Food Craving and Aversions. Nonfood Craving. High-Risk Pregnancies High-Risk: a pregnancy characterized by indicators that make it likely the birth will be surrounded by problems such as premature delivery, difficult birth, retarded growth, birth defects, and early infant death. Low-Risk: a pregnancy characterized by indicators that make a normal outcome likely. Fertility: the capacity of a woman to produce a normal ovum periodically and of a man to produce normal sperm; the ability to produce. Low birthweight: a birthweight of 5.5 lb or less; indicates poor health in the newborn and poor nutrition status in the mother. Newborn classification system based on birthweight. Maternal Health Preexisting Diabetes: depends on how well it is controlled before and during pregnancy. Gestational Diabetes: abnormal glucose tolerance that is first detected during pregnancy. Transient Hypertension: high blood pressure that develops in the second half and resolves after childbirth. Preeclampsia: a condition characterized by hypertension, fluid retention, and protein in the urine; formerly known as pregnancy-induced hypertension. Eclampsia: a sever stage characterized by convulsions seizures and coma. Maternal death during pregnancy and childbirth is extremely rare. Demands prompt medical attention. Down Syndrome: a genetic abnormality that causes mental retardation, short stature, and flattened facial features. Practices Incompatible with Pregnancy Alcohol: cause irreversible mental and physical retardation of the fetus. Medicinal Drugs. Herbal Supplements: seeks a physician’s advice. Illicit Drugs: cocaine and marijuana is common among some pregnant women. Smoking and chewing Tobacco: exert harmful effects. Sudden Infant Death Syndrome (SIDS): the unexpected and unexplained death of an apparently well infant; the most common cause of death between the 2nd week and the end of the first year of life. Caffeine crosses the placenta Placenta previa, an effect of smoking during pregnancy Typical Facial Characteristics of Fetal Alcohol Syndrome The severe facial abnormalities shown here are just outward signs of the severe mental impairments within. The internal organs also suffer irreversible damage that, while hidden, may create major problems for a child’s health. A Child with Fetal Alcohol Syndrome This child was born to a woman who drank heavily during pregnancy. In addition to the unusual facial characteristics, children with Fetal Alcohol Syndrome experience growth and mental retardation. Fetal Alcohol Effect (FAE) Alcohol Content and Caloric Value Alcohol content and caloric value of common alcohol-containing beverages. Foods can slow down the absorption of drugs in the digestive tract. Summary Adequate nutrient and energy intake is important for the normal growth and development of the fetus and the health of the mother. Energy needs increase during pregnancy, especially during the second and third trimester. There is also increased need for protein, thiamin, riboflavin, niacin, vitamin B6, folate, vitamin B12, vitamin D, iron and zinc. These needs can be met by consuming a balanced diet with additional servings of nutrient dense foods from the five food groups. Iron supplementation may be required. Summary Many nutrition-related problems can occur during pregnancy. These include nausea, constipation, hemorrhoids, heartburn, food cravings and aversions and nonfood cravings. High risk pregnancies result from various conditions. Maternal weight (either low or high), nutritional deficiencies or toxicities, improper weight gain, poor socioeconomic status, preexisting or gestational diabetes, preexisting or transient hypertension, adolescent pregnancy and alcohol/drug abuse all increase risk to pregnancy. The mother's age may influence the course of a pregnancy. The most common outcome of high risk pregnancy is a low birth weight infant. Summary Practices incompatible with pregnancy include alcohol and drug use, herbal supplements and tobacco use. Lactation is a physiological process. Breastfeeding is a learned behavior that needs a supportive environment. Nutrient needs of the mother during breastfeeding include increased need for energy, vitamins and minerals, and water. Iron supplements may be necessary. Exercise is important. Breastfeeding mothers need to be concerned about the use of alcohol, caffeine, smoking, colds, HIV infections, chronic diseases and environmental contaminants.