Community Based therapeutic care for SAM
advertisement

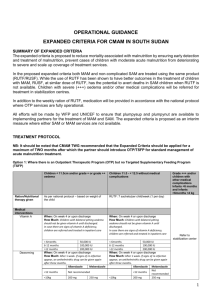
Global Health Fellowship Nutrition module SAM Defined WFH < -3z scores Visible severe wasting Nutritional edema 20 M children worldwide Most in S. Asia + sub-Saharan Africa 5-20 x higher risk death: directly or indirectly ↑ CFR in children w/ diarrhea +/or pneumonia Largely absent from international health agenda Few countries have national SAM policies CTC + Facility based approach CTC - Definition Community based model for delivering care to malnourished people Fast, effective, cost efficient assistance Manner that empowers affected communities Creates platform for longer-term solutions Main principles Basic Public Health & Development & Flexibility Coverage-decentralized Good access to services Engagement w/ & participation Local communities & infrastructure Appropriate levels of intervention Simple protocols & supplies (RUTF local) Commensurate w/ resources Sectoral integration Smooth transitions btw in-pt and out-pt Capacity building Local HCP + outreach/case finding, F/U Timeliness Early intervention to prevent progression CTC classification of acute malnutrition Moderate WFH, HFA: -3< SD score <-2 No edema Treated as out-pt Severe w/out complications WFH, HFA: SD score <-3 Edema Treated as out-pt Malnutrition w/ complications WFH, HRA: SC score -3 < SC <-2 Moderate or severe acute malnutrition Anorexia Life threatening clinical illness Admitted to in-pt care In-patient care ↑ risks nosocomial infections Mother separated from family ↑ malnutrition in siblings ↓ economic activity, food security household Expensive Low coverage Overcrowding in-pt facilities ↑ mortality & morbidity Elements in CTC: Initial Stabilization In-pt phase of treatment of SAM w/ complications Identify/treat life threatening problems Treat infections, electrolyte, specific micronutrient imbalances Begin feeding D/C to out-pt therapeutic program (OTP) ASAP appetite returns Major signs infection ↕ Irrespective of wt gain or WFH Lower Resource allocation priority than out-pt care Once sufficient resources available for good out-pt coverage Good community understanding & participation Fundamental difference: prioritization of resources 10-15% Stabilization Centers: small, little infrastructure, 1-2 skilled staff Elements of CTC: Outpatient Therapeutic Program (OTP) Direct admissions Severe malnutrition w/out complications No period on in-pt stabilization 85% of OTP admissions (coverage) Important difference in CTC Indirect admissions Malnutrition w/ complications Initial in-pt stabilization in SC Transferred into OTP Types of treatment for acutely malnourished children Moderate acute malnutrition Supplementary feeding program w/ take-home rations FBF (micronutrient fortified mix of soya-cereal flour + vegetable oil + salt + sugar Simple medicines (take at home) Severe acute malnutrition w/out complications RUTF Simple medicines (take at home) Weekly check-ups + resupply of RUTF MAM & SAM w/complications In-pt stabilization When appetite + complications controlled → OTP CTC w/ RUTF Malnourished child > 6 mos age, with appetite Standard dose of RUTF adjusted to wt Consumed at home, directly from container Minimal supervision RUTF supplied q 2-4 wk at distribution site – take home ration $3/kg if locally produced 10-14kg or RUTF over 6-8wks RUTF= Ready to Use Therapeutic Food Energy dense mineral/vitamin enriched food Peanuts, milk powder, sugar, oil + mineral/vitamin mix Easily consumed by children > 6mo age 23kJ/g (5.5 kcal/g)/ 500kcal/pk (92g) BID x 4-6 wks Equivalent in formulation to F100 Promotes faster rate recovery from SAM Oil based w/ low water activity Microbiologically safe (pt w/ HIV, chronically ill) Stores for several months Eaten uncooked, soft/crushable Ideal for micronutrient delivery (heat labile) ↓ labor, fuel, water demands RUFT=Therapeutic Food Local production ↓ cost significantly Local formulations: no milk/peanuts, but local grains + pulses, sesame oil Range of protein content Quality control, aflatoxin contamination Vehicles for probiotics + prebiotics + antioxidants Bind CTC w/ food security/agricultural interventions, local income generation + home based care for AIDS CTC SAM id: CHW or volunteers in community MUAC < 115 Nutritional edema Children 6-59 mos Full assessment following IMCI Referral to in-pt or CTC w/ regular visits to health centre Early detection + decentralized treatment prevent progression + complications Coverage Physical access, Understanding, Acceptance & Participation Negative impact of poor coverage Malnourished don’t receive care In-pt services more visible, more demands Essential steps Distribution sites decentralized ○ Balance w/ access, cost, practicalities ○ Dialogue w/ local communities served Negotiation w/ local communities ○ Central to success of CTC ○ Their concerns direct local program design Participation Vital Local communities & local health infrastructures from the start May slow down initial implementation Ultimate benefits ↓ local alienation ↓disempowerment ↓ undermining community spirit ↑program impact ↑ potential for successful handover Protocols & Implementation Core treatments protocols of OTP Objective: physiological & medical requirements Fixed Short & simple: 3 pages Easily taught to local HCP in 1 day Implementation of OTP Context specific Flexibility required Staffing, # & location of distribution sites Frequency of distribution, selection of community nutrition workers Links w/ local practitioners, MOH Rights & Choices CTC programs: uphold rights of pts w/ SAM to access OTP CTC programs: ¾ of caregivers of children w/ SAM w/ complications accepted in-pt stabilization Cost Effectiveness Core expenditures & economies of scale TFC Fixed capacity model: once center filled, others need to be built Small economies scale: central offices, logistical support CTC High initial & fixed cost: recruit/train/equip transport mobile teams, decentralize food logistics, interact/mobilize community Expansion to thousands pts w/ only extra cost of food & medicine Limitations of CTC Decentralization Aim: >90% target pop live w/in 1 day t/f walk to site Mobile teams to sites q wk/bi monthly Access: roads, security Pop confidence in mobile teams/RUFT delivery Low density of malnutrition Low prevalence malnutrition + highly dispersed pop Cost/benefit diminishing returns Fragmented/absent communities (relative) Can reduce participation, mobilization Absence of formal health infrastructure (relative) Networks of HCP, traditional healers Future Developments of CTC Approach in areas of high insecurity, urban areas “in situ” CTC w/ CHW ↑community implementation responsibility Implementation by local MOH/local actors on longer term basis National growth monitoring program integrated into existing health programs ↑ demand for CTC New RUTF recipes, lower costs, locally made for supplemental feeding Evidence 80% of Children w/ SAM who have been identified through active case finding, or through sensitizing & mobilizing communities to access decentralized services themselves, can be treated at home CFR 4.1% Coverage ↑by 72% Community based management of SAM. WHO, WFP, UN System Standing Committee on Nutrition, UN Children’s Fund CTC Preferred approach for emergency relief programs Increasingly adopted for larger non emergency programs WHO: larger-scale implementation