Congenital Infections - DrSQ
advertisement

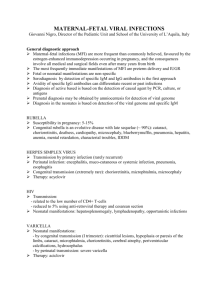
Congenital Infections TORCH Toxoplasmosis Other (syphilis) Rubella Cytomegalovirus (CMV) Herpes simplex virus (HSV) Varicella zoster (the chickenpox virus). Entroviruses Hepatitis B. Parvovirus. HIV (human immune deficiency virus). Chlamydia trachomatis. Mycoplasma. Group B streptococcus. Malaria COMMON CLINICAL FEATURES Low birth weight for gestational age Prematurity Seizures Chorio-retinitis Cataracts Purpura Cerebral calcification Micro-ophthalmia Jaundice Anaemia Hepatosplenomegaly Pneumonitis CONGENITAL CMV Caused by a DNA herpesvirus Cytomegalovirus (CMV) Most common congenital viral infection The majority of congenital infections are asymptomatic severe neurologic morbidity occurs in 80 percent of survivors sequelae appear to be more severe when infection is acquired earlier in pregnancy PATHOGENESIS Neonatal 1. Antenatal (in utero) - 80-96% of cases 2. 3. Primary Maternal Infection Recurrent Maternal Infection Perinatal Postnatal Childhood 1. Horizontal Transmission CMV excreted in saliva, urine, stool, tears 2. Organ Transplantation kidney, marrow, heart, liver, blood (leukocytes) CLINICAL FEATURES: 90% of infants with congenital CMV infection are clinically silent CNS Manifestations 70% - microcephaly 60% - intellectual impairment 35% - sensorineural hearing loss seizures 22% - chorioretinitis CLINICAL FEATURES: Systemic Manifestations Reticuloendothelial (Liver) - 65-75% 70% - hepatomegaly/splenomegaly 68% - jaundice 65% - thrombocytopenia (with petechiae and purpura) hepatitis Others 65% - low birth weight (< 2500 gm) 2-5% - pneumonitis INVESTIGATIONS Diagnostic Virology Serology PCR Serum ELISA - CMV-specific IgM of neonatal blood specimens, cord sampling Others gold standard of urine, saliva, blood, CSF, nasopharynx CBC - anemia, thrombocytopenia conjugated , unconjugated hyperbilirubinemia elevated hepatic transaminases CSF elevated protein content INVESTIGATIONS: Imaging Studies CT (Head) periventricular calcifications can be identified in 25-50% of symptomatic infants Prognosis Infants with signs of congenital CMV infection 80% have long-term sequelae: sensorineural hearing loss neuromuscular problems motor and intellectual retardation seizures chorioretinitis with visual deficits Infants with silent congenital CMV infection have a more favourable outcome ® Ganciclovir CONGENITAL TOXOPLASMOSIS caused by the protozoan Toxoplasma gondii ocular, central nervous system (CNS) incidence: 0.3-1/1000 live births Routes of Transmission Neonatal (in utero) Primary Maternal Infection acquired by the ingestion of raw or undercooked meat ( cattle), or of infectious oocysts in feces (cats, birds) 1st trimester - 17% - spontaneous abortion 2nd trimester - 25% - spontaneous abortion or severe disease 3rd trimester - 65% - subclinical disease CLINICAL FEATURES: 70% of infants with congenital toxoplasmosis infection are asymptomatic Ocular Manifestations (76%) chorioretinitis optic nerve atrophy microphthalmias blindness CLINICAL FEATURES: CNS Manifestations (52%) hydrocephaly motor and intellectual retardation seizures sensorineuronal hearing loss Systemic Manifestations classic triad of congenital toxoplasmosis : chorioretinitis, hydrocephalus, and intracranial calcifications. INVESTIGATIONS: Isolation of T. gondii from placenta or cord blood Serology measures IgG T. gondii antibody IgM fluorescent antibody test Imaging Studies CT (Head) intracranial calcifications (33%) MANAGEMENT combination of : pyrimethamine sulphadiazine folinic acid is added Spiramycin Prevention CONGENITAL RUBELLA caused by an RNA Togavirus Vaccine-preventable disease Routes of Transmission Antenatal (in utero) 1st trimester - 75-90% 2nd trimester - 35-40% 3rd trimester - 25-50% CLINICAL FEATURES: Neonatal Manifestations IUGR low birth weight - prematurity stillbirth - spontaneous abortion Early Manifestations cloudy corneas Cataracts microcephaly hepatomegaly splenomegaly jaundice pulmonary valve stenosis patent ductus arteriosus thrombocytopenia purpura INVESTIGATIONS: Virology from urine, naspharynx, CSF Serology fetal rubella-specific IgM persistence of rubella-specific IgG after 8-12 months of age