Intrauterine Infection

Intrauterine Infection
Intrauterine infection
• Abortion/stillbirth
• Congenital Malformation
• IUGR
• Prematurity
• Acute neonatal disease/delayed neonatal disease
• Asymptomatic
• Persistent infection with late sequelae
• Timing (which trimester)
Signs & symptoms of IU infections
• IUGR
• Microcephalus/hydrocephalus
• Intracranial calcifications
• Chorioretinitis
• Cataracts
• Myocarditis
• Pneumonia
• HSM
• Direct hyperbilirubinemia
• Anemia/thrombocytopenia
• Seizures/SNHL/blindness
• Skin
Blueberry Muffin
• Dermal erythropoiesis
• CMV
• Rubella
• Parvo
• Congenital Leukemia
• Rh hemolytic disease
Pregnant Women Screening (CDC)
• HIV
• Syphilis
• HBsAg
• C trachomatis
• N gonorrhhoeae if at risk
• GBS (35-37 w)
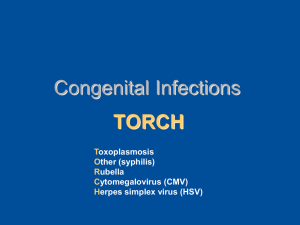
Toxoplasmosis
Toxoplasma gondii human infection:
• Undercooked meat (oocysts)
• Contact with contaminated materials
(sandbox) (oocysts)
• Organ/BM transplantation (tachyzoite/cyst)
• IU (maternal infection during pregnancy)
Primary Acquired Toxoplasmosis
• Mononucleosis like (fever, myalgia, rash, lymphadenopathy, hepatitis, meningitis, encephalitis, pericarditis, unilateral chorioretinitis, myo/pericarditis)
Ocular Toxoplasmosis
Congenital or acquired
30-40% of chorioretinitis in USA and western
Europe
Toxoplasmosis in immunocompromised
• AIDS, malignancy, cytotoxic therapy, organ transplants, stem cell transplant (Tox+→Tox-)
• CNS 50%, also heart, lung, GI
• Toxoplasmic encephalitis 25 to 50% untreated
HIV
Congenital Toxoplasmosis
• 1 st trimester 17% severe infection
• 3 rd trimester 65% mild infection
• Susceptibility (HLA DQ3 etc)
• Wide range of presentation
• 50% of infected are asymptomatic at birth almost all of them will develop ocular involvement
• 10% severe CNS & systemic
• Untreated that presents later in the first 1yr 80% IQ<70
• IUGR, lymphadenopathy, HSM, pneumonitis, nephrotis syndrome, metaphyseal lucency
• SIADH, hypothyroidism, hypopit
Congenital Toxoplasmosis
• Hydrocephalus
• Seizures
• Microcephalus, developmental delay
• CSF abnormal in 30% (sometimes protein
>1gr)
• Calcifications more in caudate nucleus and basal ganglia
• SNHL static or progressive?
Diagnosis of Toxoplasmosis
• Cultures (mice peritoneal fluid or tissue cultures 6-10 days for tachyzoites, if mouse survives and seroconverts at 6 weeks brain cysts)
• Serology:
Sabin-Feldman dye test
Specific, sensitive, difficult
Serology cont.
• IgG indirect fluorescent antibody
1-2wk after infection, peaks at 6-8 wk, persist fo life at low titers, not standardised
• IgM IFA for older children, only 25% of congenital
• IGM ELISA more sensitive and specific (50-75%)
• ISAGA (immunosorbent agglutination assay) combines IGA, IGE and IGA, no FP is the best fot congenital infection
• Differential agglutination (HS/AC) (useful for pregnant women)
“recent antigen” “late antigen”
Diagnosis cont.
• Avidity (12 vs 16 wk)
• Body fluid coefficient
• Enzyme-linked immunofiltration assay ELIFA
85% sensitivity for congenital Toxo
• PCR in amniotic fluid 17-21 gest week 95% sensitive, PCR from WBC of neonate
• Ocular = characteristic lesion with positive serology
Newborn suspected of toxo?
• General, ophtalmologic, neurologic ex
• Head CT
• Toxo PCR from peripheral blood buffy coat
• Toxo specific and total IGG,
IGM, IGE, IGA
• CSF for Toxo PCR (+general CSF )
• Mice inoculation
Treatment
• Pyrimethamine & Sulfadiazine
Contraindicated in first trimester
DHFR inhibitor, bone marrow↓
Rash, hematuria, crystalluria
Hypersensitivity, especially with HIV
• Folinic acid (leukovorin) !!!
• During pregnancy Spiramycin
Duration of treatment
• Acquired (if at all…) 4-6 wk
• Ocular untill sharp borders usually 2-4 wks + steroids
• AIDS for life or until CD4>200 for more than 6 mts and no lesions
• Congenital for 1 year
Pregnant woman
• If infection during the 6 mo prior to conception treat as described for the pregnant
• Spiramycin for prevention if motherdevelops acute toxo until 24 w
• If fetus is infected P&S&FA after 1 st trimester
• Acute toxo after 24 w = P&S&A
• Amniotic fluid PCR 17-21 wk
• Prevention!!!
Specific antiviral therapy
Nonspecific antiviral therapy
Passive immunization
Active immunization
HSV
HSV
• Primary
• Non-primary first infection
• Recurrent symptomatic and asymptomatic
• Only in humans
• Direct mucocutaneous contact
• Any anatomic site
• Predisposition
Incidence of Neonatal HSV Infection and Other Congenital Infections in North America.
Corey L, Wald A. N Engl J Med 2009;361:1376-1385.
Clinical Presentation
• Genital Herpes (15% aseptic meningitis)
• Ocular Herpes
HSV Clinical Manifestations cont.
• CNS infection:
HSV1 encephalitis, Mollaret meningitis (HSV2)
• Immunocompromised: mucositis, esophagitis, tracheobronchitis, pneumonitis, sepsis-like
Pathogenesis of Neonatal Herpes Simplex Virus (HSV) Infection.
Corey L, Wald A. N Engl J Med 2009;361:1376-1385.
Perinatal inf
• Fewer than 30% of mothers have history of herpes
• Primary (>30% risk) vs recurrent (<2%)
• Scalp electrodes
• Intrauterine: skin vesicles, microcephaly, keratononjuctivitis
• During delivery: SEM, encephalitis, disseminated
SEM
• 5-11 days few small vesicles
• If untreated may progress
Encephalitis
• 8-17 days irritability, lethargy, poor feeding, poor tone, seizures
• Usually no fever
• Vesicles 60%
• If untreated 50% will die
Disseminated
• 5-11 days
• Sepsis
• Vesicles 75%
• If untreated 90% will die
Dx
• DNA PCR
• HSV IGM unreliable
• HSV IGG only for retrospect
• Cultures
Tx
• Acyclovir
• Valacyclovir
• Famciclovir (prodrug of penciclovir)
• Foscarnet, cidofovir
• Perinatal infection – high dose (60mg/kg/day)
Common Misperceptions about Neonatal Herpes.
Corey L, Wald A. N Engl J Med 2009;361:1376-1385.
Outcome of Neonatal Herpes.
Corey L, Wald A. N Engl J Med 2009;361:1376-1385.
Cytomegalovirus
• The most common cause of congenital infection
• Important opportunistic pathogen
• β-herpes group
• Large (200-300nm)
Pathogenesis
• Attachment gB, gH proteins (interact with cell surface heparan sulfate)
• Cytoplasmic inclusion typical (accumulation of nucleocapsids and tegument in the Golgi ap.)
Pathogenesis
• Mucosal (UR or genital)
• Viremia
• Leukocytes and endothelial cells infection
• CMV-encoded cell traffic machinery
• Different tissues tropism (PM healthy people
CMV was found in salivary, lung, kidney, liver, pancreas, gut, etc)
• Viral shedding 4-6 weeks after acquisition (saliva, urine, genital)
Pathogenesis cont
• Interfere with immune response
• Maintenance of viral genome in CD34+ cells, also kidney and salivary
• Severity of disease parallels the immunity impairment
• Antibodies modify cannot prevent infection
• Critical role of T-cell mediated (most severe infection after BMT recipients, AIDS (<100cd4) and solid organ after ATG treatment)
Pathogenesis
• Majority of congenital infections are benign
• Congenital symptomatic at birth CMV=
Microcephaly, IC calcifications, CSF protein↑↑, seizures, cochlear, vestibular defects (Mondini dysplasia), retinitis, hepatitis
• 40% of maternal primary are transmittes
• First trimester = 26% symptomatic (32%), third=6%(15%)
Epidemiology
• At areas with high seropositivity >50% positive at 1 yr, >90% of first time mothers
• US overall prevalence is 59%
• Child care centers
• Second peak adolescents (sexual transmission)
• Vertical (10% of seropositive mothers shed
CMV at genital tract, 50% of neonates will be infected)
Epidemiology
• Congenital CMV 0.2-2.2% live births
• Nosocomial: breast milk, blood products
(leukocytes!), organ T, BMT, BW<1250g
• Child care workers at risk, medical workers are considered not at risk
Clinical
• Heterophil-negative mononucleosis (mean duration of fever 14 days)
• Peak ALT usually <300 IU/L
• The expected course is recovery without sequellae in healthy host
Clinical – unusual complications
• DVT, uveitis, persistant trmbocytopenia, hemolytic anemia, myocarditis, GI ulcerations, transverse myelitis, Guillain-Barre, encephalitis
Clinical manifestations – congenital
CMV
• >90% appear healthy at birth
• 7-10% petechiae, microcephaly, thrombocytopenia, conjugated hyperbilirubinemia, optic atrophy, seizures, poor sucking reflex etc etc
• 5% of asymptomatic at birth will have CNS seq
• 7-10% will have progressive SNHL
CMV in premature
• 20y ago transfusion related syndrome in VLBW
• Rare today because of leukocytes filtration
• 59% of premature <1500 gr newborns of CMV positive mothers who were fed mother’s milk were infected, half of them symptomatic (?)
• Compared with term less maternal IGG
• Symptoms = sepsis like
• No consensus, controversial studies
Transplant patients
• Solid organ:
Most common RN DP (majority will develop disease w/o treatment)
Can occur at RP also if profound immunosuppressed (5-
25%)
4-12 weeks after transplantation
Fever, malaise arthralgia, hepatitis, pancytopemia, deterioration of graft function
Pneumonitis is more common in lung or heart lung transplants
Antithmocyte globulin or anti Tlymph ab at risk
Hematopoietic Stem Cell
Transplantation
• Similar as SOT
• Pneumonia and GI disease!!!
• Prior to routine antiviral therapy 40% interstitial pneumonia (half of them CMV with
50% mortality)
• At risk DP RN, GVH, lymphopenia
• Due to ativiral therapy only 5% HSCT will develop CMV during first 120 d but late onset disease has become a problem
CMV in AIDS
• Extremely low CD4 (<50)
• Usually retinitis, esophagitis or colitis
• Controversial in neurological AIDS syndromes
• Adults>children
Lab
• In the healthy IGG, IGM (unreliable during pregnancy), IGG avidity
Lab - congenital
• Detection of CMV in body fluids within first 3 weeks
• Culture, shell vial, PCR
• Quantification in blood – to assess risk of sequella
Lab Dx Immunocompromised
• Quantification of CMV DNA in blood (different techniques: whole blood, leukocytes, plasma)
• pp65 antigenemia (immunofluorescence staining)
• Lack of standartization
Rx
• Acquired healthy – not indicated
• Congenital symptomatic ganciclovir 12 mg/kg/day in two doses daily for 6 weeks
“deserve consideration”
• Congenital asymptomatic “no evidence to support” but…