maternal-fetal viral infections
advertisement

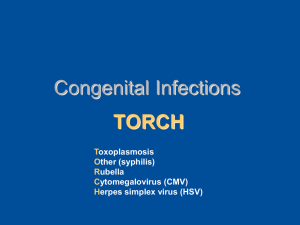
MATERNAL-FETAL VIRAL INFECTIONS Giovanni Nigro, Director of the Pediatric Unit and School of the University of L’Aquila, Italy General diagnostic approach Maternal-fetal infections (MFI) are more frequent than commonly believed, favoured by the estrogen-enhanced immunodepression occurring in pregnancy, and the consequences involve all medical and surgical fields even after many years from birth The most frequently immediate manifestations of MFI are preterm delivery and IUGR Fetal or neonatal manifestations are non-specific Serodiagnosis by detection of specific IgM and IgG antibodies is the first approach Avidity of specific IgG antibodies can differentiate recent or past infections Diagnosis of active based is based on the detection of causal agent by PCR, culture, or antigens Prenatal diagnosis may be obtained by amniocentesis for detection of viral genome Diagnosis in the neonates is based on detection of the viral genome and specific IgM RUBELLA Susceptibility in pregnancy: 5-15% Congenital rubella is an evolutive disease with late sequelae (~ 90%): cataract, chorioretinitis, deafness, cardiopathy, microcephaly, blueberrymuffin, pneumonia, hepatitis, anemia, mental retardation, characterial troubles, IDDM HERPES SIMPLEX VIRUS Transmission by primary infection (rarely recurrent) Perinatal infection: encephalitis, muco-cutaneous or systemic infection, pneumonia, esophagitis Congenital transmission (extremely rare): chorioretinitis, microphtalmia, microcephaly Therapy: acyclovir HIV Transmission: - related to the low number of CD4+ T-cells - reduced to 5% using anti-retroviral therapy and cesarean section Neonatal manifestations: hepatosplenomegaly, lymphadenopathy, opportunistic infections VARICELLA Neonatal manifestations: - by congenital transmission (I trimester): cicatritial lesions, hypoplasia or paresis of the limbs, cataract, microphtalmia, chorioretinitis, cerebral atrophy, periventricular calcifications, hydrocephalus - by perinatal transmission: severe varicella Therapy: aciclovir HEPATITIS VIRUSES HBV: transmission during delivery: chronic liver disease frequently develops HCV: vertical transmission occurs in about 6% of mothers (10-15% if HIV infection is concomitant), depending on the maternal viral load PARVOVIRUS B19 • Pathogenicity: replication in the nuclei of erythroid cells (main target pronormoblasts) • I trimester: fetal death • II trimester: fetal hydrops (aplasia > severe anemia > edema > viral spread > hemolysis) • III trimester: stillbirth CYTOMEGALOVIRUS The most common congenital infection: following both primary and recurrent infection, active CMV infection occurs in 3 to 6% of pregnant women and 0.4 to 2.2% of neonates Symptomatic congenital CMV infection: signs of reticuloendothelial (hepatosplenomegaly, jaundice, thrombocytopenia) and neurological (seizures, hyper- or hypotonia, microcephaly and periventricular calcifications, neuronal migrational disorders, sensorineural hearing loss) involvement; ocular manifestations (chorioretinitis, microphthalmia, cataract), pneumonia and purpuric rash may also occur. Therapy of severe congenital CMV disease: ganciclovir Possible use of CMV-specific immunoglobulins for fetal infection or prevention of maternal-fetal transmission following primary maternal infection Main targets of the study group Antenatal screening: is it necessary, useful or unnecessary ? Screening in pregnancy: should this be done only in seronegative women or also in seropositive women Prevalence and symptoms of active viral infection (as shown by specific IgM antibodies, genome detection, seroconversion, significant increase/decrease of IgG levels) and maternal-fetal transmission in pregnancy in different European countries Diagnostic procedures: role of specific antibodies, including IgG-avidity, DNA and antigen detection, culture; there is a need to obtain standardization of the technique and reproducibility of results Role of the immunity in maternal-fetal transmission; possible correlations between maternal cell-mediated immunity and clinical expression of fetal infection Value of the viral load in the amniotic fluid for prenatal diagnosis Clinical, laboratory and ultrasound monitoring in pregnant women with viral infections Therapeutic approaches towards viral infection in pregnancy: immunoglobulins, antiviral drugs Pediatric follow-up: how this should be done and for how long ? Therapy of congenital viral infections: only symptomatic infections? Which kinds of symptoms and signs are to be considered? Preventive use of antivirals in infants asymptomatic at birth, particularly if HIV-positive or otherwise immunodeficient?