Toxoplasmosisost
advertisement

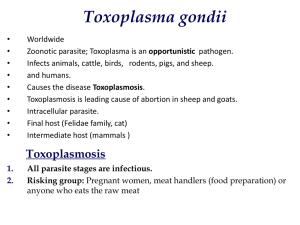
Toxoplasma gondii infects a large proportion of the world's human populations, but it is an uncommon cause of disease. The prevalence of anti-Toxo seropositivity is as high as 75% by the fourth decade of life. Toxoplasmosis • Congenitally infected fetuses , newborns and immunologically impaired individuals with defects in T-cell-mediated immunity are at high risk for severe or life-threatening disease due to this parasite. Toxoplasma gondii • - T.gondii exists in nature in three forms: the oocyst (which releases sporozoites), the tissue cyst (which releases bradyzoites), the tachyzoit (is the hallmark of primary or reactivated infection) Toxoplasmosis-transmission • Tranmission of T. gondii occurs through - the ingestion of raw or undercooked meat (pork, lamb) that contains cysts, - the ingestion of water or food contaminated with oocysts, - congenitally through transplacental transmission from a mother who acquired her infection during gestation - the transplantation of an infected organ or transfusion of contaminated blood cell The life cycle of T gondii The life cycle of T gondii http://images.google.pl/images?svnum=10&hl=pl&lr=&q=Toxoplasmosis+cycle&btnG=Szukaj Toxoplasma gondii http://images.google.pl/images?svnum=10&hl=pl&lr=&q=Toxoplasmosis+cycle&btnG=Szukaj Toxoplasma gondii - strains of the parasite • Type I strains are associated with human congenital toxoplasmosis • Type II strains are associated with reactivation of chronic infections and accounted for 65% of strains isolated from AIDS patients • Type III strains are common in animals but observed less often in cases of human toxoplasmosis Toxolasma gondii-strains Most cases in humans were caused by type II strains Toxoplasma gondii • The life cycle of T. gondii has two phases. - The sexual part of life cycle takes part only in domestic and wild cats. - The asexual part of the life cycle can take place in mammals and birds. Toxoplasma gondi-Oocyst • The definitive host, in which the sexual cycle takes place is the domestic cat. • Cats shed oocysts, that remains viable for as long as 18 months and may be ingested by many annimals and penetrate the epithelial cells of the small intestine. Toxoplama gondii- tissue cyst • Tachyzoite undergo conversion into bradyzoite which form tissue cysts. • The central nervous system, eye, skeletal smooth and heart muscles are the most common site of latent infection. Toxoplasma gondii • Organisms may spread first to the mesenteric lymph nodes and then to distant organs by invasion of lymphatics and blood • Cyst formation takes place in multiple organs and tissues during the first week of infection Toxoplasmosis Toxoplasmosis is conveniently considered in categories: • (1) acquired in the immunocompetent patient, • (2) acquired or reactivated in the immunodeficient patient, • (3) ocular, • (4) congenital Toxoplasmosis in immunocompetent patients • T. gondii infection leads to a chronic or latent infection without clinical significance. This chronic asymptomatic infection corresponds to the persistence of the cyst form in multiple tissues. • In most cases the clinical course of toxoplasmosis in the immunocompetent patient is benign and self-limited. Toxoplasmosis in immunocompetent patients • Only 10 to 20% of cases of T. gondii infection are symptomatic. Most often, toxoplasmosis manifests as asymptomatic cervical lymphadenopathy, fever, malaise, night sweats, myalgias, sore throat, maculopapular rash, hepatosplenomegaly, or small numbers of atypical lymphocytes (less than 10%) • Toxoplasmic chorioretinitis can be a manifestation of the acute acquired infection Toxoplasmosis in immunocompetent patients • Eye infection in immunocompetent patients produces acute chorioretinitis characterized by severe inflammation and necrosis. • Other manifestation of Toxoplasmosis myocarditis, myositis, hemorrhagic gastritis and colitis are rare. Toxoplasmosis in immunocompromised patients • The clinical course of toxoplasmosis in immunocompromised individuals is potentially life threatening. The brain is the most commonly affected organ. The presence of multiple brain abscesses is the most characteristic feature of TE in patients with AIDS. Toxoplasmosis in immunodeficient patients • In the United States, TE has been reported in 1 to 5% of patients with AIDS • The incidence of Toxoplasmosis encephalitis among HIV-infected individuals correlates with the prevalence of T. gondii antibodies among the general HIV-infected population, the degree of immunosuppression (CD4<200), and the institution of effective prophylactic treatment against the development of TE Toxoplasmosis in HIV patients • Clinical manifestations of toxoplasmosis in AIDS patients commonly reflect involvement: - the brain (toxoplasmic encephalitis-TE), - the lung (pneumonitis), - the eye (chorioretinitis). Toxoplasmic encephalitis -CT Toxoplasmic encephalitis-MRI Toxoplasmosis in HIV patients • Clinical manifestations of toxoplasmic encephalitis include: - mental status abnormalities, - focal motor deficits, focal neurologic findings - sensory aberrances, - seizures, cranial nerve disturbances, • cerebellar signs, • meningismus, • movement disorders • neuropsychiatric findings Congenital Toxoplasmosis • Congenital toxoplasmosis-occurs when a mother aquires the infection during pregnancy. • Infants born of mothers who acquire their infection in the first and second trimester more frequently show severe congenital toxoplasmosis. • The majority of children born of women who acquire their infection during the third trimester are born with the subclinical form of the infection. Congenital Toxoplasmosis • The congenital toxoplasmosis during the first trimester of pregnancy can cause spontaneous abortion of the fetus or can cause severe malformation at birth. • However, it is during the third trimester that the highest level of transmission occurs. The transmission rate from a maternal infection is about 45%. Of these 60% are subclinical infections, 9% result in death of the fetus and 30% have sever damage such as hydrocephalus, intracerebral calcification, retinochoroiditis and mental retardation. Congenital Toxoplasmosis • In utero transmission is lowest in the Ist trimester (15%) and highest in the 3 rd (60%). • However, severity is greatest when infection occurs in the Ist trimester. Clinical course of Congenital Toxoplasmosis • 1) neonatal disease • 2)disease (mild or severe) occuring in the first month of life • 3)relapse of previously undiagnosed infection during infancy • 4)subclinical infection Clinical manifestations of severe congenital toxoplasmosis • • • • epilepsy, strabismus, blindness, psychomotor or mental retardation, anemia, jaundice, rash, petechiae encephalitis, pneumonitis, microcephaly, intracranial calcification, hydrocephalus, diarrhea, hypothermia, • chorioretinitis which appears at a mean age of 3.7 years, Clinical manifestations of milder congenital toxoplasmosis Full-term infants frequently develop a milder disease manifested by hepatosplenomegaly and lymphadenopathy that usually appear in the first 2 months of life. In these infants, disease reflecting damage to the CNS may occur later, and eye disease may occur months to years after birth. Congenital toxoplasmosis • Congenital toxoplasmosis must be differentiated from rubella virus, CMV, and herpes simplex virus infections; syphilis, listeriosis, and other bacterial infections; other infectious encephalopathies; erythroblastosis fetalis; sepsis. Congenital Toxoplasmosis • Treatment of the mother with acute Toxoplasmosis infection with spiramycin throughout pregnancy reduces the incidence of congenital infection by about 60%. • Congenital infection after the thirst trimester of gestation is treated additionally with pyrimethamine and sulphadiazine. Ocular Toxoplasmosis in Immunocompetent Patients • chorioretinitis is a late sequela of the infection acquired in utero • is frequently in the second and third decades of life • is bilateral disease with retinal scars, and involvement of the macula Ocular Toxoplasmosis in Immunocompetent Patients • In most cases, toxoplasmic chorioretinitis is diagnosed by ophthalmologic examination, and empirical therapy directed against the organism is often instituted based on clinical findings and serologic test results. • Diagnosis may be made by demonstration of the organism in retinal biopsies, isolation of the parasite from vitreous aspirates, or amplification of the parasite DNA by PCR Toxoplasmic chorioretinitis Toxoplasmosis-DIAGNOSIS • the isolation of T. gondii • serologic tests for demonstration of anty-Toxo antibodies (Sabin-Feldman Dye Test, ELISA, IFA) • detection of T. gondii DNA by PCR or amplification in blood or body fluids; • demonstration of tachyzoites in histologic sections of tissue or in cytologic preparations of body fluids; • Antigen-Specific Lymphocyte Transformation and Lymphocyte Typing • computed tomography or magnetic resonance imaging Toxoplasmosis- treatment • Currently recommended drugs against T. gondii act primarily against the tachyzoite form and thus do not eradicate the encysted form (bradyzoite). • The 'gold' standard' regimen for the treatment of toxoplasmosis is the combination of : - pyrimethamine (200mg loading dose followed by 50–75mg qd) - sulfadiazine (2.0–4.0g loading dose initially followed by 1–1.5g q6h) - folinic (not folic) acid (10–50mg qd). Toxoplasmosis- treatment • Clindamycin (600mg q6h, up to 1200mg q6h) can be used instead of sulfadiazine in patients intolerant of sulfonamides. • Duration of treatment should be 4–6 weeks after resolution of all signs and symptoms (often for several months or longer, untill CD4>200cells/ul). . Toxoplasmosis- treatment • atovaquone+pyrimethamine are considered as an alternative treatment for patients intolerant of sulfonamides • atovaquone+sulfadiazine for patients intolerant of pyrimethamine. Toxoplasmosis- treatment • No therapy is required for lymphadenitis! • Steroids may be required in chorioretinitis !