Think Like A Toxicologist - UNM Internal Medicine Resident Wiki
advertisement

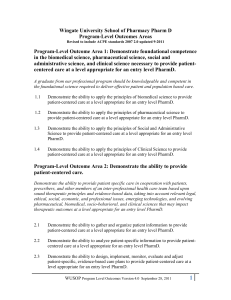
Think Like a Toxicologist Steven A. Seifert, MD, FACMT, FAACT Professor, Department of Emergency Medicine Medical Director, New Mexico Poison Center sseifert@salud.unm.edu The Poisoning Problem Poisoning is the #1 cause of trauma-related deaths (estimated 50,000/yr) > 2.3 m exposures reported to US Poison Centers in 2013 52% in children < 6 Reason: Intentional 16%; Unintentional 84% Deaths 1190 (0.05%) 19% of unintentional deaths therapeutic error Poison Center System American Association of Poison Control Centers (AAPCC) (www.aapcc.org) Center accreditation Specialist in poison information (SPI) certification National Poison Data System Data Use Annual Report (281 pages) publically available: www.aapcc.org Federal advocacy 55 Regional Poison Centers Save lives / Save money / Deliver regional benefits Cost avoidance Indirect (and direct) patient care / consultation Demographics / Toxicosurveillance Continuity of Care Research Prevention/Education Karen, PharmD Rose, PharmD, CSPI Sara, PharmD, CSPI Holly, PharmD, CSPI Stevie, PharmD, CSPI Susan Smolinske, PharmD, DABAT, Managing Director Jennifer, PharmD, CSPI Damon, PharmD, CSPI Steven Seifert, MD Medical Director Lee, PharmD, CSPI Suzi LaDonna PharmD, CSPI Gordon, PharmD, CSPI Drug Info. Heather Admin Asst. Poisoning Morbidity and Mortality Morbidity Moderate and major effects: 138,000 = 5.7 % of exposures (NPDS) Mortality ~1,500 deaths reported to PCs = 0.05% of exposures 0.0022% of pediatric exposures 20 deaths in NM (2013) NM deaths = 0.1% of exposures (double national average) Management Site 74% Managed outside of healthcare facility 22.4% Managed in healthcare facility 3.3% Admitted to ICU Top 5 Substances in Human Exposures 1. 2. 3. 4. 5. Analgesics (primarily APAP) Cosmetics / Personal Care Products Cleaning Substances Sedative/Hypnotics/Antipsychotics Foreign Bodies/Misc Top 5 Substances in Pediatric Exposures 1. 2. 3. 4. 5. Cosmetics and Personal Care Products Analgesics Cleaning substances Foreign Bodies / Misc Topical Preparations Top 10 Categories in Fatalities 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Sedative/Hypnotics/Antipsychotics Cardiovascular Drugs Opioids Acetaminophen Combinations Stimulants and Street Drugs Acetaminophen Alone Alcohols Antidepressants Serotonin Reuptake inhibitors Antihistamines Evidence-based Practice Grade “A” studies on GI decontamination; antidote development & use; enhanced elimination, etc. Consensus documents Triage criteria Managements Example: Trends in GID: 1986-04 % 15 5.2 10 5 5.6 Char coal 1.6 0.66 13.3 0.2 0 1986 2004 Lavage I pecac Ipecac Lavage Charcoal Anchor Bias/Hidden Tox Context of discovery may predispose to too rapid attribution of toxicologic etiology “Facts” are fluid Beware anchor bias Keep tox in differential / Occult presentations CO; APAP Drug accumulation (ASA, Dig, Li, Phenytoin) Drugs of abuse (myriad presentations/hidden hx) Drug-drug/Drug-food interactions Adverse drug effects Withdrawal One More Thing Use a drug-drug interaction tool with EVERY prescription you write Case 17 yo f, unresponsive at home in the morning Empty pill bottles belonging to her parents Oxycodone Atenolol Gabapentin Sertraline Metformin Case SocHx: Stressful home situation / recent departure of father No prior history of overdose or self-harm Patient’s medications: None Allergies: None Think Like A Toxicologist What’s the DDx? What is the “standard” workup of the unresponsive patient w/ tox in the ddx What are the expected toxic effects of the known or suspected substances? Pharmacodynamics: Does the clinical presentation match? What additive, antagonistic, and/or synergistic effects might be anticipated? Pharmacokinetics: What duration of effects anticipated? Think Like A Toxicologist What evaluations would be helpful Clinical exam Labs Other diagnostic tests What are the tox-specific managements Decontamination? Specific antidotes? Enhanced elimination? Symptomatic/supportive care? Case: What’s the DDx? Causes of unresponsiveness? Acute medication/substance overdose Infections Metabolic disorders Trauma / ICB / Endocrine / etc. Standard” workup of the unconscious / unresponsive patient w/ tox in the ddx BMP ECG Acetaminophen (APAP); Salicylate Other tests based on history / exam / context Case: Physical Exam Vitals: HR 52, BP 70/48, RR 8, Sat 84% Temp 37 General: Unresponsive HEENT: Membranes moist Supple neck Pupils 1-2mm; react poorly Oxycodone Atenolol Gabapentin Sertraline Metformin CV: Bradycardia Lungs: Clear Abdomen: Benign; no BS Skin: Warm, dusky, dry Neuro: Non-focal Labs / Other Tests CBC – Normal Chem 7 Na 140 K 4.1 Cl 100 Bicarb 15 Bun 18 Cr 0.9 Glucose 55 Anion Gap ? Lactate 8 Urine pregnancy Negative ASA = undetectable APAP = 230 mg/dL U Tox Oxycodone Atenolol Gabapentin Sertraline Metformin positive for opioids ECG Sinus @ 50; QRS 80; QTc 560 What’s Going On? Oxycodone Atenolol Gabapentin Sertraline Metformin Medication effects Oxycodone: CNS; RR; pupils; Opioid Toxidrome Atenolol: BP; Heart Rate Gabapentin/Sertraline: Additive CNS Sertraline: CNS depression; QTc prolongation Metformin: Hypoglycemia; Lactic acidosis (MALA) What is a Toxidrome? = Toxic Syndrome Collection / Constellation of findings that suggest a substance or substance class Allows you to refine ddx, anticipate effects, choose specific managements, avoid problems Where to focus your attention Vitals Pupils Overall physical examination Think autonomic nervous system! Opioid Toxidrome Miosis (+/-) Hypoventilation (decreased resp. rate!) Coma Bradycardia Hypotension Anticholinergic Toxidrome Tachycardia HTN Urinary retention Decreased bowel sounds Dry skin Seizures Hyperthermia Cholinergic Toxidrome “SLUDGEB…B…B…BAM” Sialorrhea Lacrimation Urination Diarrhea Gastric upset Emesis Bradycardia, Bronchorrhea, Bronchospasm Abdominal pain Miosis Sympathomimetic Toxidrome Diaphoresis Mydriasis Tachycardia Hypertension Hyperthermia Seizures Other Toxidromes Non-specific sedative-hypnotics Metabolic acidosis Serotonin syndrome Neuroleptic malignant syndrome Withdrawal syndromes Others Management: Initial Steps Pre-hospital Dextrose Oxygen Naloxone Thiamine In-hospital / Supportive Care ABCs Monitor IV Oxygen Perfusion Tox-specific Managements GI-decontamination? Applicable < 5% of cases Mostly activated charcoal (AC); rarely lavage or Whole Bowel Irrigation Specific Antidotes? Indications; proper use; contraindications Enhanced elimination techniques? Volume of distribution? Protein binding? Other properties? Urine alkalinization; Multi-dose AC; Hemodialysis; Cardio-pulmonary bypass (ECMO) Common Tox Presentations Agitation Benzos; Ketamine; Propofol; RSI; Avoid neuroleptics Rhythm disturbances Tachycardia: Usually does not require tx Bradycardia: Tx symptomatic Positioning; fluid expansion; pressors Empiric: Dopamine; NE; Neosynephrine; Vasopressin Specific: Glucagon (b-blockers); Insulin (Ca-channel blockers Seizures Atropine; pacer Hypotension Calcium channel blockers; Avoid b-blockers Benzos; Pyridoxine; Levetiracetam; Propofol; Avoid phenytoin Lipophilic cardiotoxics: Lipid emulsion; ECMO Case: Management Naloxone to reverse opioid effects Must be titrated to effect and avoid withdrawal Atropine / Glucagon for b-blocker bradycardia/hypotension Optimization of K, Ca, Mg for QTc, monitoring and preparedness to manage Torsades de Pointes Monitoring of acidosis; bicarbonate if needed; hemodialysis if needed N-acetylcysteine for elevated acetaminophen level Nomogram for Acute Acetaminophen Exposures Use nomograms and resources properly Do not send pre-4h APAP Know application of nomogram Information Resources MicroMedex (PoisIndex) Up-to-Date Library Database (“M”) Library Database (“U”) Other texts/pubmed/ etc. Use with expert guidance 2014.8 National Poison Data System New Mexico Poison Center Website National PC Number: 1-800-222-1222 Recent completion of clinical and database studies Ongoing research BWS AV Database studies Participation in ACMT ToxIC database Methamphetamine course (Aug 21) Your Primary Resource in Poisoning New Mexico Poison Center 1-800-222-1222 nationwide 2-2222 from within UNMH Poison Specialists 24/7/365 Medical Toxicologist always available