Emergency Contraception
Sue Turner: Clinical Nurse Specialist: Sexual Health
1
Menstrual cycle made simple!!!!
• The ovaries contain about 2 million follicles at
birth which develop between 3 and 7 months
gestation
• The follicles are suspended in development
until puberty
• The ovaries also secrete oestrogen and
progesterone.
Pre-Ovulatory (follicular phase)
• Follicle-stimulating hormone (FSH) from
anterior pituitary stimulates follicular
development
• During each cycle 3-30 follicles start to
develop and produce oestrogen
• One follicle becomes the dominant follicle
• Rising oestrogen levels cause a mid-cycle
surge in Luteinising Hormone (LH)
• LH surge causes ovulation – about 9 hours
later
Postovulatory (Luteal Phase)
• Ovulation leaves behind the Corpus Luteum, which
secretes progesterone.
• Unless the ovum is fertilised within 7 days, corpus
luteum degenerates, progesterone production
decreases and the endometrium breaks down and
is shed.
• Decreased levels of oestrogen and progesterone
stimulate FSH production which starts off the
recruitment of follicles and the cycle starts again
• Length of luteal phase (ovulation to
menstruation) relatively consistent at 14 days
The Menstrual Cycle
Calculating Ovulation
• Most likely date of ovulation = 14 days
before next menstrual period.
• Use individuals cycle length to calculation
estimated date of next period
7
Calculating Ovulation
January
W T
2
3
9
10
S
M
6
7
T
1
8
13
14
15
16
20
21
22
23
27
28
29
30
31
February
W T
F
4
11
S
5
12
S
M
T
3
4
5
6
17
18
19
10
11
12
24
25
26
17
18
19
24
25
26
March
W T
S
2
9
S
M
T
7
F
1
8
3
4
5
6
13
14
15
16
10
11
12
20
21
22
23
17
18
19
27
28
24
25
7
M
1
8
T
2
9
April
W T
3
4
10 11
F
5
12
S
6
13
16
14
15
16
17
18
19
20
23
21
22
23
24
25
26
27
29
30
28
29
30
T
4
11
F
5
12
S
6
13
S
M
T
4
5
August
W T
1
6
7
8
F
2
9
S
3
10
S
2
9
S
7
F
1
8
13
14
15
20
21
22
26
27
28
T
2
9
July
W
3
10
31
F
3
10
S
4
11
S
M
T
June
W T
F
7
May
W T
1
2
8
9
2
3
4
5
6
13
14
15
16
17
18
9
10
11
12
19
20
21
22
23
24
25
16
17
18
26
27
28
29
30
31
23
24
25
S
M
T
5
6
12
S
7
S
1
8
7
M
1
8
13
14
15
14
15
16
17
18
19
20
11
12
13
14
15
16
17
19
20
21
22
21
22
23
24
25
26
27
18
19
20
21
22
23
24
26
27
28
29
28
29
30
31
25
26
27
28
29
30
31
30
September
October
S
M
T
W
T
F
S
1
2
3
4
5
6
7
S
8
9
10
11
12
13
14
6
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
M
November
T
W
T
F
S
1
2
3
4
5
S
M
T
W
7
8
9
10
11
12
3
4
5
6
13
14
15
16
17
18
19
10
11
12
20
21
22
23
24
25
26
17
18
27
28
29
30
31
24
25
T
December
F
S
S
M
T
W
T
F
S
1
2
1
2
3
4
5
6
7
7
8
9
8
9
10
11
12
13
14
13
14
15
16
15
16
17
18
19
20
21
19
20
21
22
23
22
23
24
25
26
27
28
26
27
28
29
30
29
30
31
8
WHAT IS EMERGENCY
CONTRACEPTION?
• A means of preventing unintended
pregnancy following unprotected
sex.
• Acts prior to implantation –
pregnancy begins at implantation,
therefore EC is not an abortifacient
• Implantation is assumed to occur
no sooner than 5 days after
ovulation
9
Factors Influencing Risk of Pregnancy
following unprotected sex
• Ovum survives 24-36 hour.
• Sperm can survive up to 7 days (in the uterus)
• Where in cycle sex occurs from 8% risk early in
cycle to 36% on day of ovulation. Drops rapidly
following ovulation
• Fertility of both partners (unknown)
There is no time in the cycle when you can
withhold emergency contraception on
physiological grounds
10
WHO NEEDS EMERGENCY
CONTRACEPTION?
• Any Unprotected intercourse within
120hr
• Rape
• Coitus interrupts
• Contraceptive accidents – what are
these?
11
Contraceptive accidents
•Diaphragm/Cap problems
•Condom failure
•Failure to use additional precautions when starting hormonal methods of
contraception
•2 or more missed combined oral contraceptive pills (see slide 14)
•Late or missed POP (>3hrs late/12hr Desogestrel) and UPSI occurs within 2 days
following this (see slide 15)
•Missed or late Evra patches (48 hrs)
•Missed or late NuvaRings (3 hrs)
•Partial expulsion of IUD/IUS or removal mid-cycle
•Late attendance for Depo Provera( >14 weeks)
•Expired devices – IUD/IUS, implants
•Combined hormonal contraception (pills, patches & rings) & progestogen only
pills & implants - failure to use additional precautions, barrier method failure or
UPSI whilst using or within 28 days of stopping enzyme inducers including St
John’s Wort.
12
Missed pill
guidelines
FSRHC Combined
Pill Guidance 2011
1 missed pill( more than 24hrs late & up to
48hrs)
Continuing contraceptive cover
•The missed pill should be taken as soon as
remembered
•The remaining pills should be continued at the
usual time
Minimising the risk of pregnancy
Emergency contraception is not usually required
but may need to be considered if pills have
been missed earlier in the packet or in the last
week of the previous packet
2 or more missed pills (> 48hrs late
Continuing contraceptive cover
•The most recent pill should be taken as
soon as possible
•The remaining pills should be continued
at the usual time
•Condoms should be used or sex avoided
until 7 active pills have been taken. This
advice may be overcautious in the 2nd &
3rd weeks, but the advice is a backup in
the event that further pills are missed
Minimising the risk of pregnancy
If pills are missed
If pills are missed
If pills are missed
in the 1st week
in the 2nd week
in the 3rd week
(pills 1-7)
(pills 8-14)
(pills 15-21)
…………………………………………………………………………………………………
EC should be
No indication
OMIT THE PILL
considered If
for EC if the pills
FREE INTERVAL
unprotected sex
in the preceding
by finishing the
occurred in the
7 days have been
pills in the current
pill free interval
taken consistently
pack (or discarding
or first week of
& correctly (assuming
any placebo
pill taking
the pills thereafter
tablets) & starting
are taken correctly &
a new pack the
additional contraceptive
next day
precautions are used)
FSRHC Progesterone Only
Pill Guidance 2009
Traditional POPs
(Micronor, Noriday,
Norgeston,
Femulen)
> 3 hours late
(> 27 hours since the
last pill was taken)
Desogestrel – Only
(Cerazette/Cerelle)
> 12 hours late
(36 hours since the last pill
was taken)
late pill
•Take a pill as soon as remembered. If more than one pill missed just
take one pill.
•Take the next pill at the usual time. This may mean making taking 2 pills
in 1 day. This is not harmful
•An additional extra method of contraception, (condoms or abstinence)
is advised for the next 2 days (48 hrs after the POP has been taken).
Does this client need EC?
• Jasmine 24 years. Forgot to return for her depo.
Now 13 weeks and 4 days
• No
• Sophie 17 years using Microgynon 30; missed
the last 2 pills which are in the middle of the
pack. Had sex – no condom last night
• No – should use condoms until 7 days of
consecutive pills taken
16
Does this client need EC?
• Samantha 19 years. Missed her pill yesterday – no
idea what pill but takes every day & all pills same
colour. Had sex – no condom last night
• Yes – but resume pills immediately & use a condom
• Tracey 26. Stopped Cerelle due to moodiness 2
days ago. Had taken for past 2 months. Had sex no condom 3 days ago and requests EC
• No – Needs to sort future contraception
17
Does this client need EC?
• Anne-Marie 14. Had sex last night – boyfriend very
careful and pulled out before ejaculation
• Yes
• Stacey 27. Condom split. Using Gedarel 20 and no
missed pills, but always uses condoms as on a low
oestrogen pill
• No
18
Types of Emergency
Contraception
• Copper IUD – All eligible women should be
offered this as it is the most effective
emergency contraception > 99% effective
• Levonelle – Licensed for up to 72 hours
following UPSI
• ellaOne – Licensed for up to 120 hours
following UPSI
19
Emergency IUD
• Copper IUD most
effective EC > 99% !!!
• Should contain more
than 380mm Cu.
• For women wanting
the most effective
method.
• Those considering
IUD as long term
contraception.
20
Mode of Action
• Copper is toxic to the ovum & sperm & works
primarily by preventing fertilization if inserted early
in cycle.
• Pre & post fertilisation effects contribute to efficacy
• If fertilisation has occurred - anti implantation
effect.
• Therefore must be fitted before implantation
begins
• Mirena IUS must not be used as EC
21
IUD - timing of insertion
• At any time in cycle if < 5 days (120hrs) of first
episode of UPSI OR
• Within 5 days from the earliest estimated date of
ovulation e.g. not after day 19 in a 28 day cycle if
there have been multiple risks
• always check cycle length - base calculation on
shortest cycle
• remember COC bleed is not a normal period –base
calculation on first day of pill free interval
22
Contraindications to IUD
• IUD must not be used if existing pregnancy is
possible
• Allergy to copper
• Wilsons Disease
• Distorted or small uterine cavity
• PID
• Cannot promise an IUD can be fitted therefore
always give emergency contraceptive pill unless
fitting is immediate
23
Information to Client
• Discuss fitting procedure
• Discuss side effects (if wants to keep long term)
• Can be removed AFTER next period if preferred
• Can remain in and become ‘fit and forget method
for 5 to 10 years depending on IUD.
• Chlamydia screen essential, but prophylactic
antibiotics will be given
• Also give EHC unless IUD can be fitted
immediately (i.e. do not even send client back into
waiting room without EHC)
24
Levonelle
25
Mode of Action
• Incompletely understood, efficacy thought to be
primarily due to inhibition of ovulation.
• Appears to prevent follicular rupture or cause luteal
dysfunction.
• If taken prior to the luteinising surge can result in
ovulatory dysfunction in the subsequent 5 days by
which time sperm will have become non viable.
• However NO better at suppressing ovulation than
placebo when given immediately prior to ovulation
• Unknown endometrial effect on implantation
26
Efficacy of Levonelle
• Not effective immediately prior to or on day of
ovulation.
• Efficacy demonstrated up to 72 hours
(licensed use)
• Efficacy remains the same 0-96 hours i.e.
Day 0 – 4 (off-license 72-96)
• 96-120 hours pregnancy risk increases x 6
27
Contraindications to Levonelle
There are no medical contraindications to
Levonelle including breastfeeding
.
However, there are exclusion criteria
concerning your practice as a nurse working
within your PGD and/or local policy.
28
Levonelle - Special Considerations
• Pregnancy – not abortifacient, no known harm to
the woman, or the foetus, but will not be effective
if woman is already pregnant.
• Hypersensitivity to LNG or components
• UKMEC 3 for gestational trophoblastic neoplasia
with abnormal hCG
• Acute Porphyria
• Drug interactions – enzyme inducers,
ciclosporins
N.B New generic brand available i.e. Upstelle®
Levonelle off-license use
• Can be used more than once in a cycle or if
previous episode of UPSI in cycle
• Over 72 hour (if ellaOne unsuitable)
• Women taking enzyme inducing drugs 3mg (2
tablets) can be issued (if IUD declined)
NB
Repeated doses of Levonelle may be effective and
are safe. Repeated episode within 12 hours of
giving Levonelle does not require further dose
30
Information for client
• Return if vomits in 2 hours
• side effect of headache, nausea, altered bleeding, abdo
pain, dysmenorrhoea.
• Doesn’t give protection for rest of cycle
• No adverse effects on foetus should treatment fail
• May have spotting a few days after treatment this is not a
period
• Start OC on day 2 of next period OR
• If ‘quick start’ resuming OC use condoms (COC 7 days,
POP 2 days)
• Return in 3 weeks for pregnancy test if period
absent/abnormal or following ‘quick start’
31
ellaOne (Ulipristal acetate)
32
ellaOne Mode of action
• Selective progesterone receptor modulator
• Primary mode of action - inhibition or delay of
ovulation
• Given immediately prior to ovulation – can suppress
growth of lead follicle
• Can prevent ovulation after the LH surge has started,
delaying follicular rupture for up to 5 days
• Ineffective in delaying follicular rupture if given at
time of LH peak or after
• Unknown endometrial effect on implantation
33
Efficacy of ellaOne
• As effective as Levonelle between 0-72 hours,
but more effective 72-120 hours
• Effective prior to ovulation as able to prevent
ovulation even after LH surge has started
• Unknown efficacy at point of or following
ovulation
34
35
Contraindications/Cautions
• Pregnancy (no known adverse effects but limited
evidence to date
• Hypersensitivity to drug component
• Patients with severe asthma insufficiently
controlled on oral glucocoroids
• Caution in severe renal or hepatic impairment
• Hereditary galactose intolerance, Lapp lactase
deficiency or glucose-galactose malabsorption
• Excretion in breast milk not known so
recommended not to feed for 7 days after taking
• Can only be given once in a cycle
36
Drug Interactions
• Efficacy of ellaOne is reduced in women on
enzyme inducers, anti fungals & drugs which
increase gastric pH e.g. proton pump inhibitors
and antacids
• ellaOne interferes with action of progestogens
therefore reducing contraceptive efficacy. Extra
precautions therefore required for much longer
than with Levonelle
• Cannot be given concomitantly with Levonelle
37
Information to clients - ellaOne
• Return if vomits in 3 hours
• side effect of headache, nausea, altered bleeding, abdo pain,
dysmenorrhoea.
• Doesn’t give protection for rest of cycle
• May have spotting a few days after treatment. Period should be
within 7 days of expected date.
• No known adverse effects on foetus if treatment fails (limited
data)
• Start OC on day 2 of next period (NB ellaOne reduces efficacy of
OC therefore will need condoms for 7 days after EC treatment)
• If ‘quick start’ or resuming OC use condoms (COC 14 days, POP
9 days)
• Return in 3 – 4 weeks for pregnancy test if period
38
absent/abnormal or following ‘quick start’
STI Screening & Investigations
• All clients should be encouraged to have a
Chlamydia screen
• Client choosing IUD - Chlamydia test essential
and prophylactic antibiotics will be given
• All clients should be offered HIV screening
NB Screening gives a baseline following EC
and may need to be repeated
39
Quick Starting Contraception
(FSRH Sept 2010)
• Starting contraception at the time a woman requests
contraception rather than waiting for the NMP
• May reduce the time a woman is at risk of pregnancy
• May also mean starting a method immediately after EC
• Must be reasonably certain that the woman is not
currently pregnant
• Use of pregnancy testing no earlier than 3 weeks
following last sex
• ‘off-licence’
IUD – Don’t Forget
• IUD most effective form of emergency
contraception (Over 99%)
• Can stay in as ongoing contraception and lasts
up to 5 to 10 years & effective immediately
(avoids off-licence quick start!!)
• Can be used when progestogens cannot be
taken e.g. drug interaction
• Young people can have emergency IUD
Still give EHC if referring a client for an IUD
41
What method should be offered?
Factors for consideration
•
•
•
•
•
•
Medical eligibility
Efficacy of method
Last menstrual period & cycle length
Number and timing of unprotected sex
Previous use of EC this cycle
Need for additional precautions/ongoing
contraception
• Drug interactions
• Individual choice &/or service proforma/PGD
42
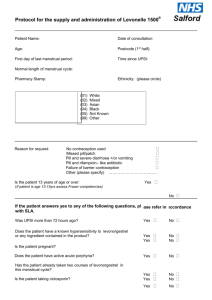
Table 2: Eligibility for different methods of emergency contraception
(FSRH Update EC Provision June 2014 )
Clinical Scenario
Cu-IUD
LNG
UPA
Single episode of UPSI within 72 hours
√
√
√
Single episode of UPSI between 72 and 120
hours
√
√ (outside product licence)
FSRH supports use up to 96 hours and up
to 120 hours if no other method
appropriate
√
Multiple episodes of UPSI within 120 hours
√
√
√
Multiple episodes of UPSI
Sex occurred <5 days ago plus > 5 days
√/X
(Yes if presents within 5 days of
ovulation. If presents more than 5 days
following earliest estimated time of
ovulation an IUD is not suitable)
√
X
Using enzyme inducing drugs
√
√
(3mg recommended- outside product
licence)
X
Breastfeeding
√
√
√
(Can be given if the woman is willing
to express for 7 days after taking)
Already used oral EC in same cycle
X
(unless all episodes within 5 days of
earliest expected ovulation)
√
X
Women under 25 years of age
√
√
√
Nulliparous women
√
√
√
43
44
45
Who to refer to sexual health services
• Clients interested in ‘IUD or quick start’
• Clients not using any contraception or have persistent
failures with their current method
• Clients who have used of EHC before/repeatedly
• Those with previous unplanned pregnancies
• Those with multiple partners
• Those attending for repeated pregnancy tests
• Those that you /they have concerns re STIs & the need
for a full screen
• Those with gynaecological problems
Contact details
- Conifer 01482 336336
- Text ‘conifer’ to 61825 (normal network rates apply)
www.conifersexhealth.co.uk
Clinical Nurse specialists in young peoples sexual health
East Riding:
Kay – 07590 304 269
Sue – 07816 645 468
HU8 & HU9:
Emma – 07590 304 278
HU6 & HU7:
Amanda – 07909 906 198
HU1 to HU5:
Tracy - 07702 366 596
47
Scenario 1: Emily – 16 years
• You see Emily at 1pm on Thurs the 1st August
• First ever sex on Monday 29th July at 9pm
• LMP 28th July– normal
• Regular 28 day cycle
• How many hours since UPSI
• What is expected date of next cycle?
• What is expected date of ovulation ?
• What emergency contraception would you offer & why?
48
Scenario 1 Emily
•
•
•
•
•
•
•
•
First ever sex so no pregnancy risk
64 hrs
LMP 28th July – normal
Estimated date ovulation = 11th August
3 days before and 2 days after = 12th – 17th
So not within dates of EDO
Offer IUD
Offer Levonelle
49
Scenario 2 – Leanne 26
• You see Leanne at 1 pm on Thursday 1st August
• Split condom on Tuesday around 11pm
• Periods irregular,
• Thinks LMP was about 4 weeks ago but not sure
• No other UPSI since LMP
• How many hours since UPSI
• What EC would you offer? Leanne also wants a
pill what advice would you need to give?
50
Scenario 2 - Leanne
• 37hrs
• LMP not clear
• Offer IUD
• Irregular cycle & unknown date of LMP so needs
ellaOne
• Use condoms for 7 days from treatment if starting
OC on 2nd day of cycle
• if ‘quick start’ condom use/abstain POP = 9 days,
COC = 14 days. Pregnancy test In 3 - 4 weeks
51
Scenario 3 – Joanne 19 years
• You see Joanne at 1 pm on Thursday 1st August
• Joanne stopped taking combined pill in the
middle of her packet 2 weeks ago (took around
10 pills) when she fell out with boyfriend. She
made up with him and had sex last night 11pm –
no condom used. Last ‘period’ 2 weeks ago on
stopping pills. No sex since stopping pill. She
wants to start pills again but doesn’t know when
to restart
• How would you manage Joanne?
52
Scenario 3 - Joanne
• 14hrs since UPSI
• Hasn’t had pills for 2 weeks so is unprotected
• Was protected until she forgot her pills so only at
risk since
• Offer IUD < 120 hours since UPSI
• ?? Period on stopping pills was not true period
• Because we don’t know where she is in her cycle
she should have ellaOne
• Re start pills immediately, condoms 14 days and
pregnancy test in 3 weeks
53
Scenario 4- Kerry
• You see Kerry at 1pm on Thursday 1st
August
• Kerry had sex at a party on Saturday night
10pm, unsure if condom used. LMP 11th July.
No other UPSI since LMP.
• How many hours since UPSI?
• What EC would you give and why?
54
Scenario 4- Kerry
• 87 hrs plus
• Offer IUD
• ellaOne
• (What if she suffers from uncontrolled asthma and is
on oral medication?)
55
Scenario 5 - Chloe
• You see Chloe at 1 pm on Thursday 1st
August. She went away with her boyfriend to a
festival, but they ran out of condoms. Several
episodes of unprotected sex since Saturday at
10 am. Her LMP 16th July and she has a
regular 28 day cycle.
• What EC should be offered? Chloe wishes to
start the pill what information do you give?
56
Scenario 5 - Chloe
• 123 hrs
• NMP due 13th August
• EDO 30th July
• Within 5 days of ovulation (13th final day)
• Offer/ refer for emergancy IUD
57
Scenario 6 - Hannah
• You see Hannah at 1pm on Thursday 1st August
• Had sex and condom split Tuesday 30th 9pm
• LMP 8th July
• Had Levonelle on 15th July
• Periods every 30 – 35 days.
• What emergency contraceptive options could
Hannah have?
58
Scenario 6 - Hannah
• 16 Hours since UPSI
• NMP 7th – 12th August
• EDO 24th – 29th July
• Cannot use ellaOne due to previous EC in cycle
• Levonelle unlikely to be effective – but could be
given.
• IUD can not be fitted as multiple episodes > 120
hours and not within 5 days of earliest ovulation
time (28th July)
59
References
Faculty of Sexual & Reproductive Healthcare [Available from www.fsrh.org]
Emergency Contraception (2011) (updated January 2012)
Quick Starting contraception (2010)
labelling of emergency contraception in Europe: Body weight and body mass
index (BMI) and efficacy (2014)
Use of Ulipristal Acetate (ellaOne®) in Breastfeeding Women: Update from the
Clinical Effectiveness Unit (201 3)
Specific Product Characteristics [Available from www.medicines.org.uk ]
ellaOne (last updated 14/5/14)
Levonelle (last update 27/11/12)
Kubba A. Connolly A. Walling M. Proctor T. French K. Mansour D. (2012)
Emergency contraception: towards a multidisciplinary consensus Primary Care:
Women’s Health Journal Vol(4) Sup1 Available from www.pcwhj.com
60