SSRIs & Antidepressants (MS Powerpoint)

SSRIs &
Antidepressants
Shanthi Antill
ST3
What we will cover…
General overview
Indications for prescribing
Choice of SSRI & side effects
Current guidance
Stopping & switching
What to do if SSRIs don’t work
Prescribing in special groups
SSRIs
Selective serotonin reuptake inhibitors
Increase extracellular level of serotonin by limiting reabsorption into presynaptic cell
Varying degrees of selectivity for other monoamine transporters
Main indications include depression, anxiety +
OCD
Advantages over TCAs include:
less sedative fewer anticholinergic SEs fewer cardiovascular SEs therefore safer in OD
Lesser effect on psychomotor performance
Side Effects
Most common = GI, commonly nausea which is dose related + often settles with use
Others include:
Psychiatric – anxiety, panic attacks
Neurological – tremor, seizures, serotonin syndrome
CV - postural hypotension
Metabolic - SIADH, hyponatraemia
Hepatobiliary – abnormal LFTs
MSK - myalgia, arthralgia
Urological - urinary retention
Reproductive - sexual dysfunction
Skin - pruritus, rash,sweating, angioedema
GI - nausea,vomiting, diarrhoea,dry mouth,GI bleeding
Other – dizziness,insomnia, drowsiness, fatigue
Type
SSRI – Selective serotonin reuptake inhibitor
Examples
Citalopram
Escitalopram
Paroxetine
Fluoxetine
Sertraline
Fluvoxamine
SNRI – Selective noradrenaline reuptake inhibitors
Duloxetine
Venlafaxine
Desvenlafaxine
NaSSA - Noradrenergic and specific serotonergic antidepressants
SARI – Serotonin antagonist and reuptake inhibitor
TCA – tricyclic antidepressants
Mirtazepine
Trazodone
Amitriptyline
Dosulepin
Doxepin
Imipramine
Points to be aware of…
Paroxetine – more weight gain, higher rates of sexual dysfunction, more dangerous in withdrawal
Sertraline – higher rate of diarrhoea
Citalopram/escitalopram – prolong QT interval so consider other medications
Fluoxetine – longer half-life compared to rest of SSRI
Mirtazepine – helps sleep, increases appetite for carbs so often causes weight gain (can be helpful with certain patients)
Choice of treatment (1)
Choice depends on:
Adverse effect profiles
Patient preference
Previous experience of treatment
Likelihood to cause discontinuation symptoms
Safety in overdose
Choice of treatment (2)
Cipriani et al, 2009
Compared 12 new generation antidepressants
Systematic review of 117 RCTs, 25928 participants from 1991-2007
Favoured escitalopram and sertraline with regards to efficacy + favorability
Sertraline as best choice when starting treatment for moderate – severe depression in adults
NICE guidance…
Depression – all SSRIs are licensed.
Paroxetine only for major depression
Panic disorder – citalopram, escitalopram, paroxetine
Social anxiety – escitalopram, paroxetine
OCD – fluoxetine, fluvoxamine, paroxetine, sertraline
PTSD – paroxetine, sertraline (only in females)
GAD - paroxetine
Starting SSRIs
Before starting ensure patients are aware that they may take a few weeks to work
Review 1-2 weeks after starting treatment.
A trial of at least 4-8 weeks (6 weeks in older patients) should be given before deciding to discontinue/change an agent
If partial response, allow another 2 weeks to decide if effective or not
Little evidence to support use of dose escalation in patients who do not respond to standard doses
After remission of symptoms, continue for at least
4-6 months (12 months in the older patient)
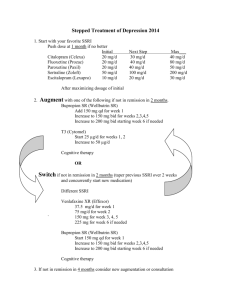
Switching treatment
No clear guidance on switching antidepressants
Maudsley Prescribing guidelines offers table of advice.
Note long half-life (1 week) of fluoxetine affects regime
MIMS/GP notebook have good online reference tables when looking to switch
Stopping treatment
Patients should be advised not to stop treatment suddenly or omit doses.
Drug and Therapeutics Bulletin advises:
after a 'standard' 6-8 months treatment it is recommended that treatment should be tapered off over a 6-8 week period
if the patient has been on long-term maintenance therapy then an even more gradual tapering e.g. by 1/4 of the treatment dose every 4-6 weeks.
if a course has lasted < 8 weeks then discontinuation over 1-2 weeks is safe
Discontinuation symptoms
Review patients who are stopping/weaning
SSRIs regularly
If suffering with any symptoms, consider increasing dose & tapering even more cautiously
Generally begin within 24-72 hours of stopping and last approximately 1-2 weeks
Most commonly nausea, dizziness, headache and lethargy
Other symptoms include paraesthesia, 'shocklike' sensations, anxiety, tremor, balance problems, nightmares, insomnia and sweating
What if treatment doesn’t work?
Consider trying different SSRI
Can try combining 2 antidepressants
Venlafaxine & duloxetine thought to be good in treatment resistant cases
Can also try older agents depending on experience
Amitriptyline/nortriptyline
Dosulepin
If still ineffective or unsure, refer secondary care
Lithium augmention
Antipsychotics
Prescribing in certain groups
Children/young people
NICE state only after specialist review
Fluoxetine 10mg first line, increased to 20mg if needed after 1 week
2 nd line – citalopram or sertraline
Post stroke depression – sertraline or mirtazepine
Chronic disease – consider sertraline as lower propensity for interactions with other medications
Elderly – consider risk of falls with SSRIs/drug interactions. Sertraline or citalopram good choices if required
Diabetes – diabetes double odds of co-morbid depression. Most data suggests fluoxetine most effective