Board Review: Ticks and TB
advertisement

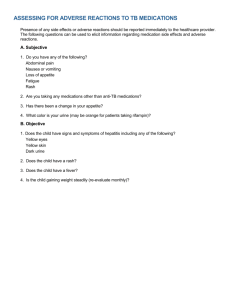
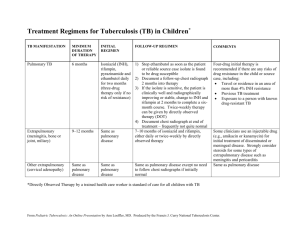
Board Review: Ticks and TB Jordan Neviackas September 10, 2013 Tick-borne diseases Lyme disease • Deer tick, Ixodes scapularis transmitting Borrelia burgdorferi • Three distinct stages: – Early localized – EM, Tx with empiric doxycycline – Early disseminated – multiple EM lesions, cranial nerves, meningitis, myocarditis (treat with IV) – Late stage – 60% untreated patient: Arthritis, encephalomyelitis • Serologic testing not recommended in early localized and restricted to those with signs or symptoms in endemic areas • Antibodies in people with nonspecific sxms of fatigue/myalgia are likely false-positives Babesiosis • Babesia microti, same tick vector as Lyme • Replicate inside erythrocytes, typically asymptomatic, but can range from febrile illness to fulminant multiorgan failure • Mild: fever, hemolysis, hepatomegaly, jaundice • Severe: hemolytic anemia, AKI, DIC, heart failure • Dx: PCR more sensitive than direct microscopy; serologic testing not recommended • Rx: – Mild: atovaquone and azithromycin – Severe: Quinine with clindamycin + exchange transfusion Southern tick-associated rash illness • Indistinguishable from early localized Lyme – EM skin lesion a/w fever, HA, myalgias • Southeast, mid-Atlantic, and south central US • No causative agent known, but vector is the Lone Star tick. • Treat with doxycycline. Ehrlichiosis & Anaplasmosis • Monocytic ehrlichiosis and granulocytic anaplasmosis, clinically similar rickettsial diseases nonfocal febrile illness with HA, myalgias and fatigue +/- rash • Antibodies appear 2-4 weeks after illness. • Treat empirically with doxycycline Rocky Mountain Spotted Fever • • • Rickettsial disease with 2-14 day incubation period Fever, headache, myalgia, confusion, GI sxms Petechial rash (90%), but only 15% at onset – • • Nonblanching macules on the wrist and ankles progressing to petechial on trunk, extremitites palsm and soles Thrombocytopenia, elevated LFTs, normal WBC Rx with doxycycline empirically and should not be discontinued based on test results. Tuberculosis Background • Rate of TB in foreign-born persons living in the US is 11 times higher than that of persons born in the US • Progression to active TB can occur after initial infection or by reactivation of LTBI • Without Rx, 10% will develop active TB during their lifetime. Clinical manifestations • LTBI is asymptomatic • Active disease is insidious: fever, night sweats, cough (bloody and/or purulent), chest pain, weight loss, anorexia • Physical is nonspecific; immunocompromised patients do not have typical signs or sxms and are more likely to develop disseminated disease • Any site may be involved; mimics other diseases • If suspected active disease, obtain TST/IGRA; CXR; microbiologic tests including AFBs and cultures Diagnosis: TST • Delayed-type hypersensitivity • Based on patient’s risk factors for infection • False negative: recent infection, age < 6 months, overwhelming infection, recent live virus vaccine or infection and anergy • Remote exposure may result in an initially negative result that can become positive several weeks later >5mm -HIV-infected persons -A recent contact of a person with active TB -Persons with fibrotic changes on chest radiograph consistent with prior TB -Patients with organ transplants -Persons who are immunosuppressed for other reasons (e.g., taking the equivalent of >15 mg/day of prednisone for 1 month or longer, taking TNF-a antagonists) >10mm -Recent immigrants (< 5 years) from high-prevalence countries -Injection drug users -Residents and employees of highrisk congregate settings -Mycobacteriology laboratory personnel -Persons with clinical conditions that place them at high risk -Children < 4 years of age - Infants, children, and adolescents exposed to adults in high-risk categories >15mm any person, including persons with no known risk factors for TB. However, targeted skin testing programs should only be conducted among high-risk groups. Diagnosis: Interferon-y Release Assay • Measure interferon-y by T cells as a response to MTB associated antigens • As sensitive but more specific than TST • Preferred when person has received BCG either as Rx or as vaccine (or poor follow up) Cultures and micro tests • If active disease suspected, cultures always need to be performed for confirmation (solid slow, liquid faster). • AFB depends on the concentration of mycobacteria • Nucleic acid amplification • Consider bronch/BAL/biopsy; ADA fluid analysis • CSF: lymphocytic pleocytosis, decreased glucose, elevated protein; AFB/cultures usually negative; PCR high specificity, but average sensitivity Radiography • Primary: localized infiltrates or paratracheal/hilar LAD • Reactivation: fibrocavitary disease in the superior segments of the lower lobes or apical-posterior segments of the upper lobes. Treatment: LTBI • 9 months of isoniazid with pyridoxine (or rifampin for 4 months • CDC included once-weekly rifapentine and isonizid Treatment: Active disease • Multiple drugs for at least 6 months – Treatment phase for 2 months (isoniazid, rifampin, ethambutol, pyrazinamide) folllowed by continuation phase (isoniazid and rifampin). – If interrupted for >2 weeks, must restart • TB meningitis for 12 months • Steroids for pericarditis and meningitis Medications • Isoniazid – rash, LFTs, peipheral neuropathy, lupus like syndrome • Pyrazinamide – hepatitis, rash, hyperuricemia • Rifampin – rash, GI upset; caution with protease inhibitors, orange body fluids • Ethambutol – optic neuritis, rash; get baseline visual acuity and color vision MDR and XDR TB • 88 cases in the US in 2010 • Resistant to at least isoniazid and rifampin • XDR also fluoroquinolones and to at least kanamycin, capreomycin or amikacin • Rx includes more medications and longer duration Questions A 22-year-old man is evaluated for a skin eruption on his leg. The patient lives in Virginia and is active outdoors. One week ago, he found a black tick on his lower leg, which his roommate removed with a tweezers. Yesterday he developed diffuse myalgia, neck stiffness, and fatigue. These symptoms have persisted, and today he notes erythema at the site of the previously attached tick. On physical exam, temp is 38.1 C (100.6 F); other vitals are normal. There is no nuchal rigidity. Which of the following is the most appropriate initial management? A. B. burgdorferi PCR on skin biopsy specimen B. Empiric IV ceftriaxone C. Empiric oral doxycycline D. Serologic testing for Lyme disease C. Empiric oral doxycycline Empiric oral doxycycline is the recommended treatment for erythema migrans regardless of the cause. A 72 year old man is evaluated for fatigue and weakness of 8 months’ duration. The patient is a retired businessman who is an avid gardener and recalls many tick attachments over the past several years. He lives in Texas but has traveled extensively throughout the US. He was seen in a walk-in clinic 1 week ago and had lab testing for Lyme disease. An ELISA for Borrelia burgdorferi was positive. A Western blot was negative for IgG and positive for IgM antibodies. Physical exam today revealed normal vital signs. An EKG is normal. What is the most appropriate management? A. Initiate additional evaluation for fatigue and weakness. B. Repeat serologic testing for B. burgdorferi in 1 month C. Treat with ceftriaxone D. Treat with doxycycline A. Initiate additional evaluation for fatigue and weakness. Nonspecific symptoms with low pretest probability for Lyme disease. ELISA is sensitive but nonspecific. When symptoms have been present for more than 1 month, a positive IgM in the absence of IgG most likely represents a false-positive. A 42 year old man is evaluated in the ED for a 3 day history of dyspnea and dizziness. He is training for a marathon and initially attributed his symptoms to overexertion and dehydration. Despite refraining from training and increasing his fluid intake, his symptoms have persisted. He has no chest pain, fever, or cough. The patient is a college professor in Rhode Island. He has not noted any tick attachments or rash. On physical, he has a normal temp, BP is 100/60 and pulse is 35. Lab results show a normal CBC, metabolic panel and cardiac enzymes. EKG shows complete heart block. Both ELISA and confirmatory Western blot are positive. What is the most appropriate initial treatment? A. IV ceftriaxone B. Oral cefuroxime C. Oral doxycycline D. Placement of a permanent pacemaker E. Observation A. IV ceftriaxone IV ceftriaxone is the recommended therapy for patients with Lyme myocarditis associated with second or third degree heart block. A 56 year old woman is seen in the ED in May for a 2 day history of fever, myalgia and headache. She works as a horse trainer in Oklahoma and recalls removing at least 3 ticks from her skin in the past 2 weeks. On physical, she appears ill with a temp of 102.7 F. Other vitals are normal. There is no nuchal rigidity, lymphadenopathy or rash. Labs: Leukocyte count 14,600 with 87% neutrophils Platelet count 136,000 ALT 177 AST 211 Serologic testing for Rickettsia rickettsii, Anaplasma and Ehrlichia is performed What is the most appropriate next step in management? A. Begin empiric amoxicillin B. Begin empiric doxycycline C. Withhold antibiotics unless a petechial skin rash develops D. Withhold antibiotics while awaiting serologic results B. Begin empiric doxycycline Delay in therapy is associated with a significant increase in morbidity (clinically difficult to distinguish anaplasmosis, ehrlichiosis and RMSF especially if there is no rash) A 27 year old man is evaluated in the ED for a 2 day history of fever, weakness and dark-colored urine. He returned yesterday from a 2 week camping trip to Cape Cod. While there, he developed a target-shaped lesion on his thigh. He was evaluated at a walk-in clinic, where early-stage Lyme disease was diagnosed. He is currently on day 10 of a 14 day course of doxycycline. On physical, temp is 101.3, BP 122/66 and pulse is 118. He is jaundiced and the liver is palpable 5cm below the costophrenic margin. Hemoglobin 8.4 Reticulocyte count 10% Leukocyte count 12,600 Platelet count 110,000 LDH 675 Total bilirubin 8.3 Which of the following pathogens is most likely causing this patient’s findings? A. Anaplasma phagocytophilum B. Babesia microti C. Borrelia burgdorferi D. Rickettsia rickettsii E. West Nile virus B. Babesia microti Because the same vector tick carries different pathogens, coinfection may occur; only babesiosis causes hemolysis. A 33 year old man is evaluated after learning that a person living in his home was recently found to have active TB. He has no acute symptoms. He was recently diagnosed with HIV and his CD4 is 250. He is a US citizen and has no history of incarceration, homelessness, or travel to areas with an increased prevalence of TB. He takes no medications but had been planning to begin antiretroviral therapy. Physical exam is normal and a tuberculin skin test induces 0 mm of induration. CXR is normal. What is the most appropriate next step in management? A. Begin isoniazid and pyridoxine B. Begin isoniazid, rifampin, pyrazinamide, pyridoxine, and ethambutol C. Begin rifampin and pyrazinamide D. No additional evaluation or therapy is needed A. Begin isoniazid and pyridoxine Patients with HIV infection who have had a known recent exposure to a close contact with active TB should receive Rx for LTBI after active disease has been excluded. A 63 year old man undergoes annual screening for TB. He is a physician, and this creening is required for maintaining his hospital appointment. His medical history is significant for bladder cancer diagnosed 1 year ago that was treated with bacillus Calmette-Guerin. There is no current evidence of active bladder cancer on follow up cystoscopy, and he has no respiratory or systemic symptoms. Physical exam is otherwise normal. What is the appropriate next step in management? A. Chest radiograph B. Interferon-y release assay C. tuberculin skin test D. two-step tuberculin skin testing B. Interferon-y release assay IGRA preferred for those who have received BCG as a vaccine or as cancer therapy and those who are unlikely to return for interpretation of the TST. A 30 year old man is admitted to the hospital with a 1 month history of fever, night sweats, cough, weight loss and chest pain. A diagnosis of pericardial tamponade is established. Pericardiocentesis is performed, following which there is no recurrence of a significnat pericardial effusion. Microbiologic examination of pericardial fluid identifies Mycobacterium tuberculosis. In addition to four-drug antituberculous therapy, which of the following is the most appropriate next treatment? A. Indomethacin and colchicine B. Pericardial window C. Prednisone D. Surgical pericardiectomy C. Prednisone Patients with TB pericarditis should receive prednisone for the first 11 weeks of therapy. Associated with improved survival and decreased need for pericardiectomy. A 25 year old woman started treatment for active pulmonary TB 6 weeks ago. The mycobacteria were susceptible to all first-line antituberculous agents, and a 2-month course of isoniazid, rifampin, ethambutol, and pyrazinamide was prescribed as initial therapy. However, the patient was lost to follow up for 3 weeks, during which time she discontinued all medications. Physical exam reveals a temp of 99.9 F, BP 110/70, pulse 90. Otherwise normal exam. What is the most appropriate management option? A. Continue the same Rx to complete the planned total number of doses, provided all doses are complete within 3 months B. Repeat sputum smear for AFB; if negative, Rx can be considered complete C. Restart different treatment with at least 2 new drugs to which the mycobactera were originally suscptible D. Restart the same treatment from the beginning D. Restart the same treatment from the beginning When a patient with active TB being treated with initial-phase antituberculous agents discontinues treatment for 2 weeks or longer, the same antituberculous regimen should be restarted from the beginning. A 53 year old man is evaluated for a 2 day history of swelling and pain of the right knee. Active TB was recently diagnosed, and he has been treated with isoniazid, rifampin, and pyrazinamide for the past 7 weeks. Ethambutol, which was also started 7 weeks ago, had to be discontinued 1 week ago after the patient experienced decreased visual acuity ascribed to optic neuritis. Mycobacteria are fully usceptible to all first-line anti-TB agents. His medicla history also includes hypertension for which he takes amlodipine. Vitals are normal. The right knee is warm, erythematous, and swollen, and he has difficulty bearing weight on this leg because of intense pain. Range of motion of the knee is restricted and elicits pain. Serum uric acid level is 10.5. A CBC reveals WBC of 14,700 with 87% PMNs and 13% lymphocytes. An arthrocentesis of the right knee reveals synovial fluid leukocyte count of 30,000 (90% PMNs, 10% lymphs). Gram stain is negative, but polarized light microscopy reveals intra and extracellular monosodium urate crystals. What is most likley responsible for this patient’s clinical findings? A. amlodipine B. isoniazid C. pyrazinamide D. Rifampin C. Pyrazinamide Pyrazinamide can cause hyperuricemia by inhibiting renal tubular excretion of uric acid. Can also cause hepatitis, rash and GI upset. Rifampin enhances kidney excretion of uric acid and can cause rash, hepatitis, GI upset, orange-colored body fluids. A 23 year old man undergoes preliminary evaluation after being admitted to a detox center because of injection drug use. Temp is 98.2, BP 125/75, pulse 90. Findings on exam demonstrate evidence of injection drug use on the bilateral upper extremities but are otherwise normal. TST testing induces 6mm of induration. The patient has no had previous TSTs. Results of a serologic test for HIV infection are negative. What is the most appropriate next step in management? A. Chest radiograph B. Isoniazid C. Isoniazide, rifampin, pyrazinamide, and ethambutol D. No additional therapy or evaluation D. No additional therapy or evaluation >5mm -HIV-infected persons -A recent contact of a person with active TB -Persons with fibrotic changes on chest radiograph consistent with prior TB -Patients with organ transplants -Persons who are immunosuppressed for other reasons (e.g., taking the equivalent of >15 mg/day of prednisone for 1 month or longer, taking TNF-a antagonists) >10mm -Recent immigrants (< 5 years) from high-prevalence countries -Injection drug users -Residents and employees of high-risk congregate settings -Mycobacteriology laboratory personnel -Persons with clinical conditions that place them at high risk -Children < 4 years of age - Infants, children, and adolescents exposed to adults in high-risk categories >15mm any person, including persons with no known risk factors for TB. However, targeted skin testing programs should only be conducted among high-risk groups. A 30 year old man is evaluated for 3 months of fever, night sweats and headache. He has a history of IVDU and is currently incarcerated. On exam, temp is 101F, BP 110/65 and pulse 95. He is oriented but lethargic. Leukocyte count is 15,000 with 70% neutrophils, 20% lymphs and 10% monocytes and the serum albumin is 2.3. The remaining metabolic panel and results of the UA are normal. LP reveals an opening pressure of 250 mm H2O. CSF shows a cell count of 400 with 95% lymphs, protein level of 200 mg/dL and glucose of 20 mg/dL. CSF PCR is positive for Mycobacterium TB and CSF culture grows M. tuberculosis. Blood culture specimens show no growth. CT scan of the head reveals basilar meningeal enhancement. Treatment with isoniazid, rifampin, pyrazinamide, and ethambutol and steroids is begun. Mycobacteria are fully susceptible to all four antituberculous agents. What is the most appropriate duration of treatment? A. 4 to 6 months B. 9 to 12 months C. 15 to 18 months D. 24 months B. 9 to 12 months Increased opening pressure, lyphocytic pleocytosis and elevated protein and decreased glucose in the CSF. CT with basilar meningeal envolvement (may also see hydrocephalus). Serial LPs should be considered to assess the response of the CSF cell count, protein and glucose levels to therapy.