Christine Roke - The Goodfellow Symposium 2012
advertisement

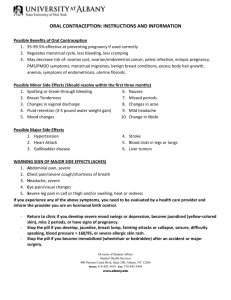
Contraceptive update Dr Christine Roke National Medical Advisor, Family Planning March 2012 Long Acting Reversible Contraception - LARC • New emphasis because: • Easier to use - action less often than monthly • Increased efficacy - all less than 1% failure rate Long Acting Reversible Contraception - LARC • Depo Provera injection • Intrauterine contraception • Implants Longacting contraception Why? • Methods that require something with every act of sexual intercourse or need to be taken every day have higher user failure rates • Combined pill has about 3% failure rate per year in every day use and 8% in first year of use • Women have first baby in NZ at about 30 • So average woman has more than 10 years contraceptive use before first baby • About 1 in 3 may therefore have an unintended conception in that time • Average woman has less than 2 children • So many years of contraception required when family complete with possible contraceptive failure WHO medical eligibility criteria for contraceptive use • WHO 1: Unrestricted use • WHO 2: Advantages generally outweigh theoretical or proven risks • WHO 3: Theoretical or proven risks usually outweigh advantages • WHO 4: Do not use Depo Provera • Problem with women returning on time for subsequent injections • Now internationally recommended that “late” injection is more than 14 weeks since last injection • Still schedule next appointment for 12 weeks Possible side effects • Most don’t put on weight • Most don’t have mood changes Depo Provera and bone density • Depo Provera may reduce bone density by 5 – 7% over the first 2 years of use – it then plateaus • Caused by suppression of oestrogen • When Depo Provera discontinued, regain this loss of bone density over next few years Bone density • Maximum increase in bone mass age 1114, some sites reach peak bone mass by 18, others later • Reduced in anorexia nervosa, exerciseinduced amenorrhoea etc • Increased in Maori and Pacific nation people Depo Provera use re bone density • Can be used by adolescents if other methods unsuitable, especially if 18 or older • All ages - review at 2 years – risks and benefits – UK Faculty of Family Planning and Reproductive Health care, WHO Intrauterine contraception Action • Primarily prevention of fertilisation – copper or progestogen immobilise passage of sperm • Can prevent implantation so copper IUD can be used for emergency contraception Intrauterine contraception • Now clear that STIs cause infection not IUDs, beyond the initial insertion phase • Ideal to exclude STIs before insertion • If asymptomatic chlamydia found, can treat and insert IUD if reinfection not likely • If STI or PID diagnosed while IUD in situ, treat and only remove if not settling Intrauterine contraception • IUDs can be used by women who have not had children • No increased risk of PID or infertility unless exposed to STIs • Insertion may be more uncomfortable • Slightly higher expulsion rate Intrauterine contraception • Fertility declines in 40s • Copper IUDs – if inserted when 40 or older, can stay until postmenopausal if no problems • Mirena - if inserted when 45 or older for contraception, can stay until postmenopausal if no problems Mirena • Efficacy not statistically different from copper IUD • Special authority if menorrhagia causing anaemia and standard treatment for HMB unsatisfactory Jadelle • Progestogen-releasing rods • 2 rods of levonogestrel - lasts 5 years • inserted subdermally into upper arm under local anaesthetic by trained clinician • Subsidised • Available on individual prescription (obtain trochar from Bayer NZ) Action Slow release of progestogen which works by • Interfering with ovulation • Thickening cervical mucus • Oestrogen levels remain above threshold for loss of bone density Jadelle efficacy Women 60kg or more Year 1 Annual pregnancy rate 0.1 Year 2 0.1 0.2 Year 3 0.1 0.3 Year 4 0.0 0.0 Year 5 0.8 1.1 0.2 Side effects • Main side effect is change in bleeding pattern • Can have other hormonal side effects but lower hormonal levels than POP – headache, weight gain, mood changes, libido – randomised control trials do not confirm difference in these side effect rates • Scar for insertion and removal occasionally local wound problem Jadelle bleeding pattern • Irregular bleeding and amenorrhoea common • Settles to long term pattern over first 3 - 6 months • Bleeding less likely to settle with time than Depo Provera or Mirena • Bleeding problems are commonest reason for discontinuation in international studies • Spotting and irregular bleeding common – 14% (1 in 7) discontinue for this reason: – 5% for prolonged episodes of vaginal bleeding and spotting – 4% for irregular bleeding – 3% for heavy bleeding Bleeding • Discussion of possible bleeding problems essential before insertion • Consider other causes of irregular bleeding • Management of irregular bleeding – COC as long as oestrogen not contraindicated – NSAIDs 5 -10 days Advantages • • • • • Efficacy Long timeframe Rapid return of fertility when removed Lower PID rates Less dysmenorrhoea Insertion • By day 7 or reliable contraception • Contraceptively effective immediately if inserted by day 5, otherwise 7 days • Contraindicated if breast cancer within last 5 years • Should not be used by those on enzyme inducing medication • Otherwise suitable for all ages provided able to manage possible bleeding problems • Superficial placement essential Removal • Do not attempt removal if implants impalpable • Refer to interventional radiologist Combined Oral Contraceptive Major WHO 4 categories Past or present circulatory disease - arterial or venous Disease of the liver – cirrhosis, jaundice Breast cancer – current within last 5 years COC and arterial disease (MI, CVA) Not an independent risk factor Amplifies other risk factors - smoking - obesity - hypertension - diabetes - hyperlipidaemia : ↑ cholesterol : family history of MI and/or CVA ARTERIAL RISK FACTORS WHO 4 CV disease in parent or sibling under 45 Cigarette smoking Smoker over 35 years of age Diabetes WHO 3 WHO 2 Lipids abnormal Lipids normal Over 35, given up < 1 year ago, no other risk factors Over 35, given up >1 year ago no other risk factors. Under 35 Has arterial disease No arterial disease BP over 160/100 BP 140 – 159 90 – 99 Hypertension in pregnancy BMI > 40 BMI 35 – 39 BMI 30 – 34 + no other risk factor Migraines With aura or takes ergotamine Without aura over 35 Without aura under 35 Age 35 or over & one other risk factor Hypertension Overweight 35 or over and no other risk factor Migraine Simple migraines present with: • Throbbing or pulsating unilateral or bilateral pain • Nausea, vomiting, anorexia • Sensitivity to light or sound • Severe and not easily relieved by aspirin or paracetamol Visual symptoms in migraine with aura • • • • • In 99% migraines with aura – usually before headache Usually symmetrical, affecting one hemifield of both eyes, although subjectively, they may appear to affect only one eye Typically begins with small bright blind spot which gradually increases in size to assume a C shape Often develop scintillating edges round blind spot which appear as zigzags May include flashing lights Neurological symptoms and signs of focal migraine • • • • • Less common Unilateral sensory disturbance typically pins and needles, spreading up one arm or affecting one side of the face or tongue – the leg is rarely affected Disturbance of speech – usually nominal dysphasia Loss of motor function is very unusual These symptoms usually follow one another – visual, then sensory, then dysphasia Headaches Migraines (without aura) - COC OK if no other risk COC contraindicated - migraine with aura - migraine without aura plus additional risk factor for stroke including age over 35 Past history of migraine with aura and no other risk factors – WHO 3 Risk of venous thrombosis (DVT/PE) RISK: for non pregnant woman between 15-44 yr olds - 5-10 per 100,000 for pregnant woman - up to 10 times risk on low dose second generation pills - 3-4 times risk on other combined pills - 6 times risk or more Fatality rate 3% Risk factors for venous disease WHO Category 4 WHO Category 3 VTE in parent or sibling under 45 Abnormal clotting factor or tests not available Overweight BMI over 39 BMI 35 – 39 Immobility Confined to bed Wheelchair Past Thrombosis Extensive varicose veins Varicose Veins WHO Category 2 Normal clotting factors BMI 30-34 Superficial thrombophlebitis First line COCs – second generation pills Oestrogen 35mcg Norethisterone Levonorgestrel *Brevinor 1 *Norimin *Brevinor Norinyl-1 30mcg 20mcg * Government subsidised pills *Levlen Microgynon 30 *Monofeme Nordette Loette Microgynon 20 Other combined pills Higher VTE risk Oestrogen Progestogen Brand name Use 30mcg 20mcg Desogestrel Marvelon Mercilon Third generation 35 mcg Cyproterone acetate *Ginet 84 Moderate/severe acne, PCOS 30 mcg 20 mcg Drosperinone Yasmin Yaz Acne, PMS, bloating 50mcg Levonorgestrel *Microgynon 50 Enzyme inducers, BTB Side effects • Irregular bleeding and chloasma are linked to COC use • Randomised control trials do not show that COC causes weight gain, headaches, breast tenderness, nausea or change in libido • Nocebo effect – experience symptoms because aware they are possible Starting instructions for COC If starting with a hormone pill: Day 1 - 5 of cycle safe = straight away Any other time not safe until 7 hormone pills have been taken (one each day) Missing COC pills • WHO: additional precautions required only if: • Miss 3 x 30mcg pills in a row • Miss 2 x 20mcg pills in a row • UK FFPRHC: 2 missed pills in a row • Data sheets still recommend additional precautions if 12 hours late • NZ Family Planning teach missing any 2 pills within a week Missed pills One missed pill, take it as soon as remembered, taking the next pill at the usual time – this may mean taking 2 hormone pills together Any 2 pills missed within a week of each other, follow the 7 day rule. 7 day rule Not contraceptively safe until 7 hormone pills have been taken in a row Use another method of contraception such as condoms or do not have sexual intercourse while taking the 7 hormone pills If during this time a condom breaks or slips off, the emergency contraceptive pill (ECP) is indicated. If there are less than 7 hormone pills left in the pack, finish the hormone pills and start the new pack immediately (miss the 7 inactive pills or the 7 day break) Vomiting, diarrhoea and other medications Vomiting or severe diarrhoea for more than 24 hours, follow the 7 day rule and miss the 7 inactive pills (or 7 day break) if necessary Enzyme inducing medications reduce efficacy – need to use higher dose COCs and shorten break between hormone pills of each packet Antibiotics no longer thought to cause significant interaction Missed pills FIRST WEEK: Danger of ovulation following pill free week 7 day rule essential Emergency contraception required if additional precautions not taken If any UPSI during the 7 days before missed pills, client needs ECP (may be > 72 hours) SECOND WEEK: No additional precautions required THIRD WEEK: Miss pill free week, no additional precautions required If pill free week taken, emergency contraception may be required. New ways of taking COC • Tricycling = taking 3 packets of pills in a row without a break • Continuous = no breaks • Less risk of contraceptive failure • Less breakthrough bleeding with time but some women will find this spotting a problem – take 7 day break • No known medical concerns Continuous pill taking • Family Planning is offering as a choice • Should be better efficacy • With 21 hormone pill regimen, missing more than 1 pill prejudices efficacy • With continuous pill regimen, need to miss more than 8 pills before efficacy prejudiced Mortality associated with COC 39 year follow up of cohort of 46000 women from Royal College of General Practitioners Oral Contraception Study Pill users had a lower mortality rate than non users Increase in cervical cancer and cerebrovascular deaths balanced by decrease in ovarian cancer deaths BMJ 2010 Causes of breakthrough bleeding Late or missed pill Diarrhoea or vomiting Medications - enzyme inducers, antibiotics Infection - chlamydia Abnormal cervix – ectropion, cancer Pregnancy First few months of new pill Hormone dose too low Running packets together Progestogen only pills Use when oestrogen contraindicated or side effects with COC No increased risk of arterial or venous disease or cancer Progestogen only pills Noriday and Microlut work mainly by altering cervical mucus Variable suppression of ovulation Cerazette reliably suppresses ovulation Distance penetrated (cm) Sperm penetration test 3 Repeat Dose 2 1 0 0 2 4 6 8 10 12 14 16 18 20 22 24 26 Time (hours) Progestogen only pills Noriday and Microlut – missed pill = 3 hours late, 2 days before protection reestablished Cerazette – missed pill = 12 hours late, 2 days for cervical mucus protection, 7 days if waiting for ovulation suppression Timing of ECP • UK FFPRHC recommend taking LNG ECP up to 72 hours – registered use • No statistical difference between first 4 days • Can be given on 4th day • No evidence that ECP effective on 5th day