Methods of Contraception
advertisement

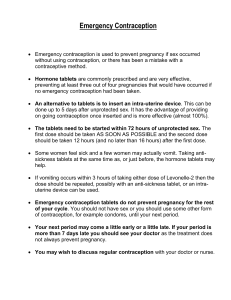
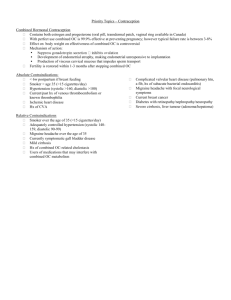
Dr Fahmi I. EL-URI METHODS OF CONTRACEPTION Methods of Contraception Contraception is the prevention of conception by methods other than abstinence , its used to limit the size of family ( birth control ) or ( Family planning) Ideal Contraception An ideal contraception should fulfill the following: Highly efficient Free from unwanted side effect Absolute safety Simplicity of use Reversible Well tolerated Methods of Contraception The following is an overview of the currently available methods of contraception: Barrier Methods The condom Diaphragms and cervical caps Spermicides Hormonal Methods Oral contraceptives Injectable contraceptives Implants Other Methods Intra uterine devices Periodic abstinence/ NFP natural family Planning ( I. e safe period ) Sterilization IUCDs Barrier Methods The condom Simple Effective methods of contraception- 98% success rate Without side effects Available Reduce the risk of STDs including the acqui immune deficiency syndrome ( AIDS) 40 MILLION COUPLES RELY ON CONDO GLOBALLY Diaphragms and Cervical Caps and The Sponge The diaphragms and cervical caps should be used with spermicide Failure rate 5-10 % The sponge is known in the U.K and the USA Advantage of the sponge in that it can be left for 24 hours in the vagina ,besides that one size fits all women Success rate 85- 95 % Diaphragm Spermicides In the form of creams, gel aerosols, melting suppositories and foaming tablets Used alone Failure rate 10- 15 % Hormonal Methods Oral contraception three types: Combined monophasic pill: most commonly used ( combination of estrogen and progestogen) Triphasic combined pill : estrogen and progestogen but the ratio varies during the month to mimic the natural hormonal pattern in the menstrual cycle Progestogen only pill : mini pill Combined Oral Contraceptives Advantages These are simple to use and highly effective No special preparation is necessary before intercourse The pill may relieve irregular menstrual periods, cramps and premenstrual tension Combined Oral Contraceptives Advantages (continue….) Less likely to get cancer of the uterus Less suffering from ovarian cysts Much less likely to suffer from ectopic pregnancy Fewer attacks of rheumatoid arthritis Disadvantages: Some women have difficulty remembering to take their daily pill Some women experience side effects such as nausea, breast tenderness or , weight gain or loss, headache , depression and spotting or bleeding between menstrual periods Disadvantages The estrogen -containing contraceptives present increased risk of serious disorders due to blood clotting in some women ( low dose is recommended) A woman should not take the combined pill while breast -feeding an infant Disadvantages Oral contraceptives sometimes interact with other drugs. This can result in diminished contraceptive effectiveness or interference with another drug’s activity Average annual failure rate including patient error and omissions: 2.6 unwanted pregnancies per 100 couples P.s. Healthy women not smoking under 35 years the risk of taking combined pill are very small by comparison with risks associated with pregnancy and child birth Progestogen Only Pill ( mini pill) Has higher failure rate than combined pill Suitable for lactating mother Action By the interference with the passage of sperm through the cervical mucous, also affect the endometrium making it less suitable for implantation of the embryo Side Effects Headache Nausea Intermittent bleeding Thrombosis Hypertension further research under taken to develop a once month pill Hormonal Contraception The designation of first , second or third generation progestins derives from the timing of introduction of each product containing these various progestins into the market place All progestins used In oral contraceptives are derivatives of 19 nor-testerone Norgestimate, gestodene and desogestrel are cumulatively referred as third generation OCs Injectable Contraceptives Has proven to be highly effective method of fertility regulation The most widely available injectable contraceptive in the U.K , Germany , New Zealand , Sweden and many countries all over the world Injectable Contraceptives Contents: synthetic progesterone, administered once every three months Side effects: headache, dizziness, weight gain , menstrual disturbances, no life threatening complications such as CV effects seen with Ocs. Implants The recent development in the field of hormonal contraception Six capsules which are implanted under the skin of the arm and provide contraception for five years It should be put in the place by a trained health worker and at the end of the five years the capsules can be removed Implants Proper aseptic techniques should be used during insertion and removal to avoid infection at the site of implant Implants Side Effects Irregular bleeding in the first few months followed by amenorrhea Norplants are non-biodegradable ( biodegradable = absorbed by the body) A two rod, 18 month implant is being developed as well IUDs These are plastic or metal devices which are placed in the uterus to prevent pregnancy More than 60 million women around the world use IUDs Common available IUDs :lippes loop copper T copper 7 Multi load Nova T Side Effects of IUDs Expulsion Perforation Heavy and prolonged bleeding P.S Superiority of copper released IUDs over plastic devices in the terms of perforation, expulsion, and continuation rate Periodic Abstinence Advantage: not requiring mechanical or medical measures – accepted by certain religious groups This method of family planning is based on attempts to identify the fertile period of the menstrual cycle, which occurs around the time of ovulation and abstaining from intercourse during this time = calendar method ( I. E. day 9 to day 19 in 28 days regular cycle) Periodic Abstinence 1. 2. This method is less effective than techniques that record BBT and monitor consistency of the cervical mucus both of these undergo changes at the time of ovulation NFP methods can be used both: To prevent pregnancy To plan pregnancy Periodic Abstinence Side effects: not present due to inexperienced couples and not well motivated, the pregnancy rate can be as high as 25% Sterilization Male sterilization ( vasectomy) safe operation, out patient procedure under local anesthesia Female sterilization mini lapratomy under local or general anesthesia * laparoscope's------- Coagulation ------- Rings ------- Clips All to obstruct tubal patency, prevent pregnancy Conclusion The world population is around 6 billion , four hundred million couples are practicing a family planning, many couples around the world who are motivated to practice family planning lack the sources or the methods suitable for their needs. At least one method may be suitable for each couple at any given time in order to plan their families avoid unwanted pregnancy. Emergency Contraception or Post-Coital Contraception : Since 1984 , the Yuzpe method has been used to reduce ‘ risk of pregnancy by administering two doses of ‘ following medication 12 hrs apart & within 72hrs of unprotected intercourse : 100 microgram Ethynil oestradiol plus. 500 microgram Levonorgestrel . Continue : The endometrium is made unfavourable for implantation & there is interference with normal corpus luteum function . If taken before ‘ preovulation estrogen surge, ovulation can be inhibited . The medication is often administered with an antiemetic to reduce nausea & vomiting, which occur in up to 50% of patients . Continue : The failure rate is 2-5 %, depending on ‘ time in ‘ cycle at which it is taken . Counselling is essential so that ‘ patient understands ‘ implications of ‘ failure rate & so that she makes sure she is followed up, especially if she has not a period but also to decide on future longterm contraception . Continue : More recently , this method has been superceeded by : Levonelle-2 ( x2 tabs of 750mg Levonorgestrel ) which is available over ‘ counter . Another method of emergency contraception is to insert an IUCD within 5 days of unprotected intercourse , this can be removed after ‘ patient’s next period or left in situ as a contraception .