PALLIATIVE CARE A Brief Intervention
advertisement

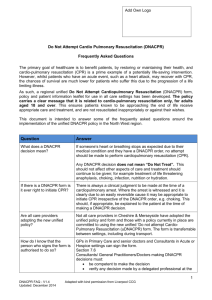
GP ST 1&2 PALLIATIVE CARE & ETHICS Niall Cameron Rosalie Dunn Carolyn Mackay Euan Paterson Palliative Care and Ethics 09:00 Palliative care – Planning in an uncertain world 11:30 Coffee / Tea 12:00 Symptom Relief in Palliative Care 12:45 Dining with death! 13:30 End of Life Ethics 14:45 Coffee / Tea 15:00 The ‘Good Death’ 16:30 Feedback / Close Some all too common problems… • • • • • • • • • The ‘sudden’ deterioration What does the patient know / think / want? What do the family know / think / want? Lack of medication Blue light ‘999’ at end of life Who knows what? The weekend catastrophe The ‘bad’ death… …and then 4 hours to confirm it happened! Who are we talking about? • What cohort of patients do YOU think we are talking about? Who is WHO talking about? ‘Palliative care is an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.’ World Health Organisation Who is Chuck talking about? ’Marla doesn’t have testicular cancer. Marla doesn’t have Tb. She isn’t dying. Okay in that brainy brain-food philosophy way, we’re all dying, but Marla isn’t dying the way Chloe is dying’ Chuck Palahniuk - Fight Club Who are we talking about? • Probability / possibility • Uncertainty • What about… - Renal failure / dialysis Advanced lung cancer COPD 93 year old / multi-morbidity / dementia Who are we talking about? • Probability / possibility • Uncertainty • What about… - Renal failure / dialysis / decision taken to stop dialysis Advanced lung cancer / semi-conscious / no fluids COPD / chest infection 93 year old / multi-morbidity / dementia / UTI How do we decide? • Consider ‘dying’ as a possibility! • What primary disease do they suffer from? Numbers and Trajectories Function High Function High Cancer Death Low Death Low Months or years Weeks to years Organ failure GP has 20 deaths per list of 2000 patients per year 5 2 Acute 6 Function High 7 Death Low Many years Dementia, frailty and decline Diagnosing dying • Personal trajectory – How are they at this moment? – How were they? – How rapidly are they changing? • Would you be surprised…? Who are we talking about? • Patients with supportive / palliative care needs • Whoever YOU feel should be included! • And consider: – – – – – – Palliative care register GSF register SPICT / GSFS prognostication guidance? Chronic disease registers? Care Home patients?? Housebound patients??? The 9 Cs C1 C2 C3 C4 C5 C6 C7 C8 C9 Consider dying as a possibility Competence Compassion Capacity Communication Care planning Ceilings Current needs Care in the last stages of life C 1 – Consider dying as a possibility • The last dozen slides… C 2 – Competence • Your own! • Do you have enough knowledge & skills? - Diagnostic accuracy Knowledge of condition, natural history, interventions Communication skills • Do you have enough experience? • Do you need help? • Who can you get help from? C 3 – Compassion • Show that you care! - Be polite and courteous Make it personal Show interest Add ‘little touches’ / Unbidden Acts of Human Kindness(!) Give your time (even when you have very little!) Empathy & Compassion C 4 – Capacity • Does the patient have capacity? • If not do they have a legally appointed representative e.g. PoA or Guardian? • Other medico-legal aspects - Consent (KIS / ePCS) Advance decision to refuse treatment C 5 – Communication • Who needs to know? • What do they need to know? • How? C 5 – Communication • Who needs to know? - Patient / family / loved ones - Colleagues e.g. Partners, Nurses, OOH, SAS, Acute, Specialists • What do they need to know? - Possibility / probability of death Prognostic uncertainty What the plans are That you care! • How? - In person, telephone, KIS C 6 – (Anticipatory) Care Planning • Plan A - Active treatment aimed at recovery • Plan B - Active treatment aimed at a good and dignified death C 7 – Ceilings of treatment / intervention • What are the ceilings? E.g. - Transplant Admission / transfer Dialysis / ventilation / cardiac devices(!) CPR Surgery / drug therapy Antibiotics (and route) Nutritional support Hydration (including S/C fluids) C 8 – Current needs • Physical - Symptom relief - Bowel / bladder care - Oral care • Psychological • Personal - Social - Spiritual (the inner self) C 6 – (Anticipatory) Care Planning • Plan B - Probable / Possible Prescribing • Rationalise medications - • What is essential What is not needed What to do with those in between Just in Case - What might be needed / Route of administration - Processes • • • DN VoED DNACPR End of Life Care Plan DNACPR DNACPR – Fundamentals • • • • The decision to offer CPR is a medical one Nothing to do with ‘quality of life’ If CPR is likely to be futile do not offer it Patient / family view is only relevant if CPR is a treatment option • If success anticipated – discussion needed • If success not anticipated – inform patient • Relatives should not be asked to ‘decide’ unless patient lacks capacity & legally empowered to do so DNA CPR – Framework • Is the patient at risk of a cardiopulmonary arrest? • Decision making - CPR is unlikely to be successful due to: - The likely outcome of successful CPR would not be of overall benefit to the patient • decided with patient • decided with legally appointed... • ...basis of overall benefit... – CPR is not in accord with a valid advance healthcare directive/decision (living will) which is applicable to the current circumstances DNA CPR – Decision making • Is CPR realistically likely to succeed? – – – – What do we mean by ‘success’? Population that we are considering Facilities available People available Introducing the subject of DNACPR • Communication • Breaking bad news – Narrowing the information / knowledge gap – We know something we think they need to know! • E.g. CPR futile or CPR not futile and do they want it – – – – How much do they actually know? How much more, if any, do they want to know When do they want to know Who do they want to tell them Discussing DNACPR • • • • • • • • • • Know the patient and their context Be clear about benefit/burden balance of CPR (Rx) Consider benefit/burden balance of discussion Consider who should discuss Consider when to discuss Discussion on CPR should be part of wider discussion Often less difficult earlier in disease Small chunks and check… (BBN) Aim is to Allow a Natural Death Compassion! Getting CPR raised • By patient and carer – Spontaneously – Prompted • Another professional e.g. the hospital said… • ‘My Thinking Ahead & Making Plans’ Getting CPR raised • By us (in the course of a discussion) – – – – – – How do you feel you are doing? Where would you like to be cared for? And if things got worse…? How do you see the future? Are there any things you’d like to avoid? Etc etc etc… Getting CPR raised • By us (more pushy…) – If you’re really keen to be kept at home then • What to do if there was a sudden change in your condition • What to do if your heart was to stop CPR – the subject matter • General – What it means • Allow a natural death – Likelihood of success – Whether ‘people’ would wish it • Individual – In your case… • ‘Fine line’ – Awareness raising, BUT – Clinical decision has already been made What DNACPR is not about • • • • Anything other than CPR Any other treatments e.g. antibiotics Feeding Fluids • Highlight everything else that we can still do Patient centred supportive care • • • • • • What’s the most important thing in your life right now? What helps you keep going? How do you see the future? What is your greatest worry or concern? Are there ever times when you feel down? If things get worse, where would you like to be cared for? Professor Scott Murray, University of Edinburgh DNA CPR – Practicalities • • • • Completing the DNACPR form Where should form be kept When to update form Patient transfer DNA CPR – Practicalities • Communication – Patients home • • • • • Patient Family / loved ones OOH Services Scottish Ambulance Service Others? C 9 – Care in the Last Stages of Life • Care checklist - Review ceilings of treatment / intervention Review medication Review hydration Review current needs Plan for death • Communication - Does everyone know that now just Plan B? • Compassion (yet again!) C 6 – (Anticipatory) Care Planning Advance Care Planning Legal Welfare Power of Attorney Advance Statement Continuing Power of Attorney 1 Statement of values 2 Preferences & priorities 3 Advance decision to refuse treatment 4 Who else to consult Guardianship Medical Personal Thinking ahead & making plans SPAR Potential Problems DNA CPR Lanarkshire Home Care SPAR Pack GSFS Just in Case KIS / ePCS DN Verification of Expected Death End of Life Care Plan (LCP) Anticipatory Care Planning Patient / Personal • Preferred priorities of care – – – – Place of care Place of death Admission? Aggressiveness of treatment • What is wanted • What is not wanted – Who is to be involved The views and wishes of patient / carer • ‘My thinking ahead and making plans’ - What’s important to me just now Planning ahead Looking after me well My concerns Other important things Things I want to know more about e.g. CPR Keeping track Developed from work by Professor Scott Murray & Dr Kirsty Boyd, University of Edinburgh Advance statement • Statement of values - E.g. what makes life worth living • What patient wishes - E.g. place of care, aggressiveness of treatment • What patient does not want - E.g. PEG feeding, SC fluids, CPR • Who they would wish consulted ACP Process • • • • When should this be done? Who should do it? How should it be done? How can it be shared? ACP Process • When should this be done? – At any time in life that seems appropriate – Continuously • Who should do it? – By anyone with an appropriate relationship! • How should it be done? – My Thinking Ahead & Making Plans – Carefully – Write it down • How can it be shared? – KIS / (ePCS) – Other communication Which patients is KIS for? • Not just palliative care! • Patients with supportive / palliative care needs – – – – – – – Whoever YOU feel should be included! Palliative care register GSF register SPICT / GSFS prognostication guidance? Chronic disease registers? Care Home patients?? Housebound patients??? What is KIS for? • Information transfer – In Hours GP to OOH GP – Primary Care to A&E / Acute Receiving Units – Primary Care to Scottish Ambulance Service • • • • • Prompts for proactive care Anticipatory Care Planning All data stored in one place Structure for lists / meetings / etc Palliative care DES What does KIS contain? 0 : Consent 1 : Demographics 2 : Current situation 3 : Care & Support 4 : Resuscitation & Preferred Place of Care ePCS What does KIS contain? 0 : Consent • KIS Upload decision • Patient consented? These two are essential for data upload • Apply Special Note • KIS Review date What does KIS contain? 1 : Demographics • • • • • • • • Patient Details Practice Details Usual GP Patients Emergency Contact Number Carers Next of Kin Access Information Agency Contacts What does KIS contain? 2 : Current Situation • • • • • • • Medical History Self Management Plan Anticipatory Care Plan Single Shared Assessment Oxygen Additional Drugs Available at Home Catheter and Continence Equipment at Home What does KIS contain? 3 : Care & Support • • • • Moving and Handling Equipment at Home Adults with incapacity Form Guardianship with Welfare Decision Making Powers Power of Attorney What does KIS contain? 4 : Resuscitation & Preferred Place of Care • Preferred Place of Care • DNACPR • Form in place What does KIS contain? ePCS • • • • • Consent for Electronic Transfer to ePCS Services Care at Home (basically presence of syringe pump) OOH arrangements GP OOH Contact Number(s) Patient’s Understanding The ACP Checklist • Capacity – Power of Attorney / Possible future problems? • Have we considered – – – – What is likely & what might happen to this patient? Where the patient would like to be cared for? CPR / DNACPR? OOH information transfer (KIS/ePCS) • Have we considered the possible need for – Anticipatory prescribing (Just in Case) – RN Verification of Expected Death – The Liverpool Care Pathway for the Dying • The patient / carer view – My Thinking Ahead & Making Plans… Knowledge K Skills K S Attitudes K S A