PowerPoint presentation template
advertisement

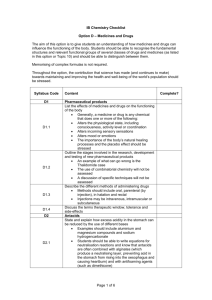
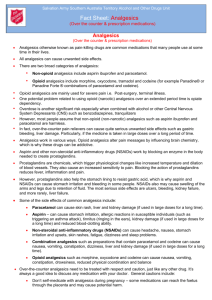
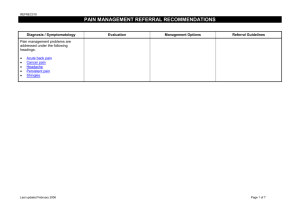
Pain management Learning objectives At the end of the workshop you will be able to: • Consider the important principles of pain and pain management • Use validated tools to assist in assessing patients pain • Outline strategies to manage pain with your patients • Discuss pain medicines with your patients What is pain? • A message to the brain, pain is a ’whole body’ experience and involves both the mind and the body • Usually a protective mechanism to warn us to be more careful of our bodies • It hurts and may cause suffering or distress • Different for different people: it is whatever the person says hurts Types of pain • Acute pain can be important for the body to tell the brain that there is something wrong and help to avoid harm. • Chronic pain is pain that goes on for a long time. It needs regular assessment and a different approach to treatment. Chronic pain impacts on the whole person and their community Ask your patients about any changes that have happened in their lives since their ongoing pain started. For example: • How are you sleeping? • Are you feeling worried or sad? • Are you still visiting friends or relatives? • Are you eating well? Things to talk about: • How pain is affecting their life • Where the pain is, how bad the pain is • How long they have had the pain • What medicines they are taking for the pain (and any other conditions) • How the pain has affected them and their family • If they have any other problems or worries • Make sure people understand that it may not be possible to be pain-free at all times • Anticipation of pain How do we assess pain Ask the patient: • To describe their pain • Rate their pain (use the faces scale based on how they perform everyday activities) • What made the pain worse or better REMINDER: Observe the person’s body language (how freely do they move). Talk with the person about how they feel, and how it affects their everyday life Talk with their family when appropriate Make sure people understand that it may not be possible to be pain-free at all times Use the same pain assessment tool to keep a detailed record of the patients’ pain changes in the clinic notes. Managing chronic pain Treatment goals: • To improve the level of activity • To modify thoughts about pain and suffering • To promote self-management • To relieve pain to a tolerable level Managing chronic pain Tips on helping people to exercise • Educate patients that there is a difference between ‘hurt’ and ‘harm’ when you have chronic pain. Avoiding physical activity can make their pain seem worse over time. • Encourage patients to talk to their family and friends and not isolate themselves. Also get a family member or friend involved as their ‘exercise buddy’. • You may wish to suggest some exercises to try e.g. walking, swimming, gentle stretching exercises. Remember to start slow with exercise as they may feel some discomfort initially, especially if they have been inactive for a long time. Medicines Key points: • Use a step-wise approach to introduce pain medicines (analgesics) • Prescribe regular doses of analgesics • Plan a trial period with clear and specific instructions • Review the effects on regular basis eg may need more frequent review for new medicines or when dose changes Analgesics – Non-opioid analgesics AMH 2010, CARPA 5th edition Nonsteroidal anti-inflammatory drugs (NSAID) Generic names and how given Other NSAIDS Diclofenac Indomethacin Ketoprofen Ketorolac Mefenamic acid Naproxen Piroxicam Tiaprofenic acid Cox-2 Inhibitors: Celecoxib Meloxicam Parecoxib What it is used for Mild to moderate pain and fever Reduces swelling and inflammation in arthritis , period pain, sprains and injuries or attacks of gout Renal colic Suppositories are used when the patient is vomiting .They can still cause stomach pain when used for long period s Gels can be used as a rubbing medicine Can be used with other medicines How it works Prostaglandins in the body cause redness, swelling and pain at the site of injury. NSAIDs stop the body making prostaglandins Adverse effects AMH 2010, CARPA 5th edition Short-acting and long-acting opioids Short-acting opioids Long-acting opioids codeine Modifies release tramadol Methadone Tramadol hydromorphone Immediate-release morphine Immediate-release oxycodone Immediate-release tramadol Modified-release hydromorphone Modified-release morphine Modified-release oxycodone Transdermal buprenorphine Transdermal fentanyl Opioid analgesics – Combination analgesics Generic PARACETAMOL + names and Codeine 30 mg how given (Panadeine Forte ®, Codalgin Forte ®) What it is used for Moderate to strong pain relief Can be used in combination with other pain relief medicines How it works Two different medicines work together (but in different ways) in the brain and nerve ending to reduce pain Adverse effects •Drink lots of water to prevent constipation Laxatives may be needed • Return to the clinic if need to Use for more than a short time •If you take more than 8 tab lets a day containing paracetamol you can damage your liver (make sure there is no paracetamol in your other medicines) Opioid analgesics - Morphine AMH 2010, CARPA 5th edition Opioid analgesics - Tramadol Generic names and how given TRAMADOL What it is used for Moderate to severe pain Slow release formulations are used for chronic pain How it works Adverse effects AMH 2010, CARPA 5th edition Drug interactions (do not take with) Warfarin SSRI Venlafaxine Carbamazepine St John’s Wort Take home messages When you see a person who has pain: • Perform a thorough history and physical examination to determine if referral is necessary • Discuss options for managing pain with the person • Recommend medicine only as part of an agreed pain management plan Resources • Australian Pain Management Association’s Pain Link Helpline (1300 340 357) • Australia’s National Phone Information and Support line (1800 218 921) Provide support for patients, their carers and health professionals. • Chronic pain Australia – www.chronicpainaustralia.org Your name Contact details