NASH CRN - Ennect Mail
advertisement

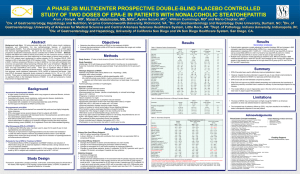
Nonalcoholic Fatty Liver Disease Stephanie H. Abrams, MD, MS Assistant Professor of Pediatrics Baylor College of Medicine Medical Director-Kamp K’aana shabrams@bcm.edu NASH: a typical case 57 year old white female with elevated LFTs in 2008 No symptoms; history of obesity, type 2 diabetes, hypertension, hyperlipidemia, depression/anxiety Meds: metformin, olmesartan/HCTZ, thyroxine, alprazolam, metoprolol, sertraline, clonidine, vitamins SH: Occasional alcohol; nonsmoker PE: BMI 41 kg/m2 Lab: ALT 77, AST 81, AP 179, T bili 0.3, gluc 199, plts 168, INR 1.1 NASH: a typical case Liver biopsy: NASH, NAS 4, stage 2 with extensive periportal fibrosis Plan: weight loss, exercise Follow up at 6 months: "No symptoms"; "working on wt loss" PE: weight down 3 lbs/6 months NASH: a typical case Admitted after no follow up x 2 years Increased abdominal girth, dyspnea, leg edema Wt up 60 lbs in 6 weeks Minor MVA with confusion Interim diagnosis: obstructive sleep apnea PE: Ascites, 3+ leg edema, alert/oriented Lab: ALT 55, AST 102, Alb 2.6, INR 1.7, MELD 15, plts 149 CT: nodular liver, splenomegaly, perisplenic varices, moderate ascites NASH: a typical case Abdominal CT: NASH: a typical case Summary: Progression of NASH to cirrhosis in setting of obesity, DM2, HTN Near normal liver enzymes Prevalence of NAFLD in Adults NAFLD was present in 46% of all subjects by ultrasound (n=400) 74% of diabetics Prevalence higher in men (58.9%) Most common in Hispanics (58.3%), Caucasians (44.4%), African Americans (35.1%) NAFLD patients: Were more likely to have HTN, higher BMI, & DM Ate more fast food & exercised less NASH present in 12.2% of all adults Present in 22.2% of diabetics Advanced fibrosis in 22.5% 30% of all of those with NAFLD NASH: 12% Williams CD, et al. Gastroenterology 2011; 140: 124-131 Prevalence of NAFLD in Children Fatty liver was present in 13% of all subjects Prevalence higher in boys (11.1%) compared with girls (7.9%) Prevalence increases with age 17.3% for ages 15-19 years NASH present in 3% of all children Schwimmer, et al. Pediatrics 2006 Prevalence of Fatty Liver by Race/Ethnicity Percentage 15 10 5 0 Black White Asian Hispanic •Using a logistic regression model, the odds ratio for the presence of fatty liver in Hispanics was 5.0 Schwimmer, et al. Pediatrics 2006 NASH as an indication for transplant * *PN = Probable NASH based on risk factors Brandman et al, AASLD 2011 Primary Diagnoses for Patients in 2006 NASH Accounted for 10.3% of all Transplanted Liver Transplantation at the Cleveland Clinic in 2006 33.1% 12.8% 10.3% A lc o H e ho pa lic titi C sC C ir r ry ho pt si og s en N ic A Ci SH rr ho si B s ili ar PS y C C O th ir r ho er M si et C s irr ab ho ol R et ic si ra s D ns is ea pl an se tG ra ft BA Fa M i al lur e ig na nc y O th er Percent 35 30 25 20 15 10 5 0 www.clevelandclinic.org Pathogenesis: new ideas “Two hit” vs lipotoxicity Liver fat metabolism: Insulin resistance Diet, uncontrolled diabetes Excess peripheral lipolysis Excess carbohydrates Increased circulating fatty acids De novo lipogenesis Hepatocellular free fatty acids Triglyceride B Tetri VLDL (secreted) “Two-hit” hypothesis: Insulin resistance Excess peripheral lipolysis Increased circulating fatty acids Diet, uncontrolled diabetes Excess carbohydrates De novo lipogenesis Hepatocellular free fatty acids SER (P450) ω-oxidation Peroxisomal β-oxidation 2 ROS Mitochondrial β-oxidation Triglyceride 1 NASH B Tetri Lipid droplets (steatosis) VLDL (secreted) ROS = reactive oxygen species Lipotoxicity hypothesis: Insulin resistance Excess peripheral lipolysis Excess carbohydrates Increased circulating fatty acids De novo lipogenesis Hepatocellular free fatty acids Lipotoxic metabolites • • • • B Tetri SER (P450) ω-oxidation Peroxisomal β-oxidation Mitochondrial β-oxidation ER stress Inflammation Apoptosis Necrosis NASH Diet, uncontrolled diabetes Triglyceride Lipid droplets (steatosis) VLDL (secreted) Neuschwander-Tetri BA. Hepatology, 52:774-788, 2010 Lipotoxicity hypothesis: • Ceramides • Diacylglycerols • Lysophosphatidyl choline • Others Insulin resistance Excess peripheral lipolysis Excess carbohydrates Increased circulating fatty acids De novo lipogenesis Hepatocellular free fatty acids Lipotoxic metabolites • • • • B Tetri SER (P450) ω-oxidation Peroxisomal β-oxidation Mitochondrial β-oxidation ER stress Inflammation Apoptosis Necrosis NASH Diet, uncontrolled diabetes Triglyceride Lipid droplets (steatosis) VLDL (secreted) Neuschwander-Tetri BA. Hepatology, 52:774-788, 2010 Treatment of NASH • Weight loss • Exercise • TZDs? Insulin resistance Excess peripheral lipolysis Divert to muscle • Exercise Increased circulating fatty acids • • • Diminish toxicity • Vitamin E? ER stress • Fish oil? Inflammation • Ursodiol? Apoptosis Necrosis NASH B Tetri Excess carbohydrates De novo lipogenesis Hepatocellular free fatty acids Lipotoxic metabolites • Diet, uncontrolled diabetes Lipid droplets (steatosis) • Cut the carbs! Divert to muscle • Exercise SER (P450) ω-oxidation Peroxisomal β-oxidation Mitochondrial β-oxidation Triglyceride Facilitate storage/secretion • Betaine? VLDL (secreted) Neuschwander-Tetri BA. Hepatology, 52:774-788, 2010 NASH and the Metabolic Syndrome Bad diet + Obesity + Sedentary + Genetic predisposition IR Excess circulating NEFA Increased liver triglyceride Steatosis β-oxidation Lipotoxic intermediates in the liver NEFA: nonesterified fatty acids, ie, free fatty acids IR: insulin resistance PCOS: polycystic ovary syndrome NASH NASH and the Metabolic Syndrome Cancer PCOS Hyperinsulinemia β-cell loss Bad diet + Obesity + Sedentary + Genetic predisposition IR Excess circulating NEFA Reninangiotensin activation Vascular disease HTN CAD/PVD Hypertriglyceridemia Hypercholesterolemia Diabetes Increased liver triglyceride Steatosis β-oxidation Lipotoxic intermediates in the liver NASH Sleep apnea NEFA: nonesterified fatty acids, ie, free fatty acids IR: insulin resistance PCOS: polycystic ovary syndrome Treatment of NASH Lifestyle modification remains the primary treatment recommendation Bariatric surgery Neuschwander-Tetri, B. A. Lifestyle modification as the primary treatment of NASH. Clinics in Liver Disease (2009) 13: 649-665 Harrison, S. A. and Day, C. P. Benefits of lifestyle modification in NAFLD. Gut (2007) 56: 1760-1769. Sullivan, S. Implications of diet on nonalcoholic fatty liver disease. Curr Opin Gastroenterol (2010) 26: 160-164. Pillai, A. A. and Rinella, M. E. Non-alcoholic fatty liver disease: is bariatric surgery the answer? Clinics in Liver Disease (2009) 13: 689710. Drugs Ratziu, V. and Zelber-Sagi, S. Pharmacologic therapy of non-alcoholic steatohepatitis. Clinics in Liver Disease (2009) 13: 667-688. Trial results NASH CRN PIVENS trial Pioglitazone vs Vitamin E vs Placebo in adults Excluded diabetics, cirrhotics PIVENS Study Design Randomization Eligibility assessed by local pathologist (1:1:1) Wk 0 Month -6 Liver biopsy End of treatment Liver Biopsy Wk 96 Vitamin E (rrr α-tocopherol) 800 IU/day Week 120 end of study placebo Pioglitazone (30 mg/day) N Engl J Med (2010) 362: 1675-1685 PIVENS Primary endpoint: Decrease in NAS by 2 or more points, with at least a 1 point drop in ballooning, and no worsening of fibrosis 2 Primary comparisons: Vitamin E vs placebo Pioglitazone vs placebo Significance set at p< 0.025 Secondary endpoints: changes in individual histologic features resolution of steatohepatitis changes in anthropometrics, insulin resistance, quality of life adverse events N Engl J Med (2010) 362: 1675-1685 Proportion of subjects (%) Vitamin E alone met the pre-specified primary endpoint 50 40 P< 0.001 P< 0.04 36/84 NNT=4.4 26/80 NNT= 6.6 30 20 16/83 10 0 Vit E placebo treatment groups Pio proportion of subjects (%) Both vitamin E and pioglitazone increased the proportion of subjects with resolution of NASH 100 80 P< 0.0008 P< 0.01 60 40 44/84 40/80 23/83 20 0 Vitamin E placebo study groups pioglitazone Liver enzymes -10 -20 -30 -40 Change (U/L) 0 ALT 0 24 48 72 96 Weeks Placebo Vitamin E Pioglitazone Change in body weight 0 2.5 -2.5 Change (kg) 5 WEIGHT 0 24 48 72 96 Weeks Placebo Vitamin E Pioglitazone Who should we treat with vitamin E? Should we look for low vitamin E levels? Does reduction in the ALT mean the patient is responding? Who should we treat with vitamin E? • Responders didn’t have low initial vitamin E levels Vit E treated • The increase in vitamin E did not correlate with response • Non-compliance did not explain nonresponse Loomba et al, AASLD 2010 Who should we treat with vitamin E? • Responders didn’t have low initial vitamin E levels • The increase in vitamin E did not correlate with response Vit E treated Placebo • Non-compliance did not explain nonresponse Loomba et al, AASLD 2010 Who should we treat with vitamin E? Non-responders P = 0.005 Responders • ALT dropped a bit more in responders than placebo • ALT dropped in both responders and nonresponders Loomba et al, AASLD 2010 PIVENS trial summary Vitamin E helped in about half the patients Non-cirrhotic, non-diabetic Natural vitamin E, 800 IU/day We don’t know why it works We can’t predict who will respond or who is responding Pioglitazone helped a bit less that half the patients NASH CRN TONIC trial Treatment of NAFLD in Children = TONIC NASH Clinical Research Network study Hypothesis: metformin and vitamin E are superior to placebo for the treatment of NAFLD Lavine et al, JAMA (2011) 305: 1659 TONIC trial Multicenter, double masked, double placebo, randomized Metformin 500 mg bid + vitamin E placebo or Vitamin E (natural form) 400 IU bid + metformin placebo or Both placebos bid Treatment duration: 2 years A priori endpoint: change in ALT Secondary endpoint: histology Lavine et al, JAMA (2011) 305: 1659 ALT TONIC: changes in primary endpoint (ALT) Metformin Placebo Vitamin E Lavine et al, JAMA (2011) 305: 1659 ALT TONIC: changes in primary endpoint (ALT) Metformin No significant differences Placebo Vitamin E Lavine et al, JAMA (2011) 305: 1659 % with resolution TONIC results: Liver biopsy changes Vitamin E increased resolution of NASH (from initial definite or borderline NASH) P = 0.006 N.S. Lavine et al, JAMA (2011) 305: 1659 TONIC trial summary Vitamin E helped about half the children Primary endpoint of ALT change not met (placebo improved) Biopsies did improve 800 IU of natural vitamin E daily Metformin did not help Lavine et al, JAMA (2011) 305: 1659 Treatment of NASH 2011 Focus on preventing adipose IR and associated systemic lipotoxicity Doing this treats NASH and comorbidities Lifestyle modification Exercise: Goal of 30-45 minutes aerobic daily Weight loss gradual and sustained bariatric surgery an option Healthy eating portion control avoid sugar sweetened beverages no trans-fats Treatment of NASH 2011 Drugs Vitamin E? Thiazolidinediones? (pioglitazone, rosiglitazone) Statins? Metformin-no benefit of improving hepatic insulin sensitivity Not effective: ursodiol, betaine Benefit of controlling co-morbidities on NASH? Recognize and treat obstructive sleep apnea Treating hyperlipidemia, improving glycemic control: no effect on liver Future directions Incretin mimetics? Naturally occurring: GIP, GLP-1 Made by enteroendocrine L-cells Responsible for 70% of post-prandial insulin secretion Delays gastric emptying, increases satiety Peripheral effects? Analogue: exenetide Inhibit breakdown by inhibiting FXR agonist for NASH FXR = “Farnesoid X receptor” = ligand activated nuclear receptor Bile acids are the major natural ligands Increased bile acids decreased synthesis, increased export FXR agonist for NASH Cholesterol Gut BA BA BA BA = Bile acids FXR agonist for NASH Cholesterol Gut Exporters (MDRs, BSEP) TGR5 Bile acid receptor BA + FXR BA BA Hepatic and peripheral effects FGF19 synthesis by enterocytes FXR BA BA = Bile acids FGF=Fibroblast growth factor FXR = Farnesoid X Regulation of gene expression by FXR Neuschwander-Tetri, B. A. Curr Gastroenterol Rep (2012) 14: 55-62 FXR agonist for NASH High affinity FXR ligand Research options at SLU NASH Clinical Research Network studies NASH CRN treatment trials FLINT (FXR Ligand in the Treatment of NASH) Enrolling now! “Database” observational study, seeking: Ideally patients suspected of having NAFLD but not yet biopsied Can enroll with a biopsy < 3 months old Annual visits with free lab tests until 2014 tetriba@slu.edu Pathogenesis of NASH: A Two “Hit” Hypothesis OBESITY Dyslipidemia Type 2 Diabetes FFAs Hyperinsulinemia Insulin sensitivity Leptin sensitivity Adiponectin effect FAT STORAGE FIBROSIS HSCs activation Festi, et al. Ob Rev. 2004; 5: 27- 42 TNFa IKKb Endotoxin Leptin LPO end products TNFa ATP NF-kb IL-6 1st Hit FFAs Lipid Peroxidation ROS Scavengers Inflammation Necrosis Apoptosis 2nd Hit Normal Environment Steatosis Steatosis genes Steatohepatitis Oxidative Stress, cytokine, & endotoxin related genes Genes Fibrosis & cirrhosis Fibrosis genes Day CP. Liver International 2006 Environmental Factors Alcohol intake Low is protective Dietary factors Low antioxidant vitamins saturated fat Obesity * Food intake Lack of exercise Type II DM* Small bowel bacterial overgrowth Sleep apnea syndrome *Have a genetic component Wilfred de Alwis, NM & CP Day Seminars Liv ds. 2007 Hypothesis Both pioglitazone and vitamin E are superior to placebo for the treatment of NASH. NASH CRN Specific Aim To perform a prospective multicenter, double-masked, double-placebo, randomized clinical trial of pioglitazone (30 mg/day) or vitamin E (rrr α tocopherol 800 IU/day) versus placebo pioglitazone provided by Takeda under a CRADA vitamin E provided by Pharmavite under a clinical trials agreement NASH CRN Inclusion and exclusion criteria Inclusion criteria: Alcohol consumption < 20 gm/day for women and 30 gm/day for men Biopsy proven steatohepatitis within last 6 months NAFLD activity score: ≥ 5 with definite or probable steatohepatitis =4 + definite steatohepatitis agreed by 2/3 pathologists Exclusion criteria: Diabetes mellitus Cirrhosis Prior bariatric surgery Any drug therapy for NASH between biopsy and randomization Presence of other liver diseases NASH CRN Study Design Randomization Eligibility assessed by local pathologist (1:1:1) Wk 0 Month -6 Liver biopsy End of treatment Liver Biopsy Wk 96 Vitamin E (rrr α-tocopherol) 800 IU/day Week 120 end of study placebo Pioglitazone (30 mg/day) NASH CRN Plan of Analysis (all histologic analyses on blinded central review of deeper cuts of baseline liver biopsy & end of treatment biopsy) Primary endpoint: Decrease in NAS by 2 or more points, with at least a 1 point drop in ballooning, and no worsening of fibrosis 2 Primary comparisons of proportion of subjects who met endpoint: Vitamin E vs placebo Pioglitazone vs placebo Significance set at p< 0.025 Secondary endpoints: changes in individual histologic features resolution of steatohepatitis changes in anthropometrics, insulin resistance, quality of life adverse events NASH CRN Baseline Characteristics Means or %s Age (yrs) Female (%) Caucasian (%) BMI (Kg/m2) Waist circumference (cm) AST (IU/L) ALT (IU/L) AP (IU/L) Bilirubin (mg/dl) Triglycerides (mg/dl) IR (HOMA-IR) Vitamin E N= 83 Placebo N= 84 Pioglitazone N= 80 46.6 61 66 34 107 59 86 77 0.7 166 5.2 45.4 58 81 35 109 55 81 82 0.7 165 5.5 47 59 74 34 108 54 82 86 0.7 162 5.0 NASH CRN Baseline histology blinded central review of deeper cuts of baseline liver biopsy Vitamin E Mean or % Placebo Mean or % Pioglitazone Mean or % Steatosis grade Inflammation grade Ballooning grade Fibrosis stage NAFLD activity score (NAS) 1.9 1.8 1.3 1.5 5.1 1.9 1.6 1.3 1.6 4.8 2 1.8 1.1 1.4 5 % without ballooning on central review of deeper cuts of baseline biopsy 18 17 27 NASH CRN Proportion of subjects (%) Primary Outcome –Vitamin E alone met the pre-specified primary endpoint 50 40 P< 0.001 P< 0.04 36/84 NNT=4.4 26/80 NNT= 6.6 30 20 16/83 10 0 Vit E placebo Pio treatment groups NASH CRN Both Vitamin E and Pioglitazone improve steatosis proportion of subjects (%) worsened improved Improvement in severity of steatosis grade Vit E vs placebo: p< 0.0001 Pio vs placebo: p< 0.0001 80 P< 0.001 P<0.0001 60 40 Δ grade 0.8 Δ grade 0.7 Δ grade 0.1 20 0 -20 Vit E placebo pioglitazone -40 NASH CRN proportion of subjects (%) worsened improved Both Vitamin E and Pioglitazone improve lobular inflammation 80 p< 0.01 p< 0.001 60 40 Δ grade 0.6 20 Δ grade 0.7 Δ grade 0.2 0 -20 Vit E pioglitazone placebo -40 -60 Improvement in severity of inflammation: Vitamin E vs placebo: p< 0.008 Pioglitazone vs placebo: p< 0.0009 NASH CRN proportion of subjects (%) worsened improved Both Vitamin E and Pioglitazone improve the severity of ballooning and the proportion of subjects whose ballooning improves 80 60 40 P<0.02 Δ grade 0.5 20 -40 -60 Δ grade 0.4 Δ grade 0.2 0 -20 P<0.02 Vit E pioglitazone placebo Improvement in severity (grade) of ballooning: Vit E vs placebo: p< 0.01 Pioglitazone vs placebo: 0.03 NASH CRN proportion of subjects (%) Both vitamin E and pioglitazone increased the proportion of subjects with resolution of NASH 100 80 P< 0.0008 P< 0.01 60 40 44/84 20 40/80 23/83 0 Vitamin E placebo pioglitazone study groups NASH CRN Mutually exclusive categorization of reasons for not meeting primary outcome Vit E N=48/84 Placebo N=67/83 Pio N=53/80 No follow up biopsy 4 11 10 Worsening of fibrosis score 15 16 12 Failure to improve NAS ≥ 2 22 35 20 Failure to meet primary outcome due to ballooning score=0 at baseline 7 5 11 Categories NASH CRN proportion of subjects (%) worsened improved Neither Vitamin E nor Pioglitazone improved fibrosis scores or proportion of subjects with improved fibrosis 60 40 20 n.s. Δ grade 0.3 n.s. Δ grade 0.1 Δ grade 0.4 0 -20 Vitamin E placebo pioglitazone -40 -60 Improvement in severity of fibrosis scores: Vit E vs placebo: p= 0.19 (n.s.) Pioglitazone vs placebo: p=0.1 (n.s.) NASH CRN Liver enzymes -10 -20 -30 -40 Change (U/L) 0 ALT 0 24 48 72 96 Weeks Placebo Vitamin E Pioglitazone NASH CRN Insulin resistance -1 0 1 HOMA-IR 0 48 96 Weeks Placebo Vitamin E Pioglitazone NASH CRN Change in body weight -2.5 0 2.5 5 WEIGHT 0 24 48 72 96 Weeks Placebo Vitamin E Pioglitazone NASH CRN Adverse events Adverse event Vitamin E Placebo Pioglitazone Total SAE Drug-related SAE Deaths 7 0 1 10 0 0 2 0 0 ALT > 500 IU/l Bili > 3 mg/dl 0 1 0 0 0 2 CVD events New onset T2DM Bone fractures Bone ΔT > -1 12 4 3 0 12 0 5 0 10 0 3 1 NASH CRN Summary -1 Vitamin E (800 IU/day), but not pioglitazone (30 mg/day), was superior to placebo for histological improvement as defined in the primary outcome measure Both vitamin E and pioglitazone significantly improved: Steatohepatitis Steatosis grade Inflammation grade NAFLD activity score Neither drug improved fibrosis scores significantly NASH CRN Summary -2 Pioglitazone improved insulin sensitivity, but was associated with weight gain There were no study drug related SAEs NASH CRN Conclusions Vitamin E is superior to placebo for the treatment of active NASH in nondiabetic adult patients. Pioglitazone did not meet the primary outcome for histological improvement, but significantly improved other key histological features of NASH. Neither drug improved fibrosis Both agents were relatively safe over the 96 week study, although pioglitazone was associated with weight gain NASH CRN Treatment Of Nonalcoholic steatohepatitis In Children (TONIC) The NIDDK Clinical Research Network (NASH CRN) Hypothesis Both metformin and vitamin E are superior to placebo for the treatment of NAFLD NASH CRN Specific Aim To perform a multicenter, double-masked, double-placebo, randomized clinical trial of metformin (500mg BID) or vitamin E (RRR-atocopherol 400 IU BID) versus placebo for the treatment of NAFLD Over-encapsulated generic metformin/placebo Vitamin E/placebo provided by Pharmavite under a Clinical Trials Agreement (CRADA) NASH CRN Inclusion and exclusion criteria Inclusion criteria: Boys & girls 8-17yo Biopsy proven NAFLD within 6 mos ALT>60 U/L at randomization and 112mos prior Able to swallow pills Informed consent/assent Complete screening in 112 days Exclusion criteria: Diabetes mellitus Cirrhosis Prior bariatric surgery Significant alcohol ALT>400 Presence of other liver diseases Pregnancy/nursing Any drug tx for NASH in the 3mos prior to randomization NASH CRN Hypothesis Both metformin and vitamin E are superior to placebo for the treatment of NAFLD NASH CRN NASH CRN Specific Aim To perform a multicenter, double-masked, double-placebo, randomized clinical trial of metformin (500mg BID) or vitamin E (RRR-atocopherol 400 IU BID) versus placebo for the treatment of NAFLD Over-encapsulated generic metformin/placebo Vitamin E/placebo provided by Pharmavite under a Clinical Trials Agreement (CRADA) NASH CRN Primary Outcome-neither treatment met criterion for sustained ALT reduction NASH CRN Specific Aim To perform a multicenter, double-masked, double-placebo, randomized clinical trial of metformin (500mg BID) or vitamin E (RRR-atocopherol 400 IU BID) versus placebo for the treatment of NAFLD Over-encapsulated generic metformin/placebo Vitamin E/placebo provided by Pharmavite under a Clinical Trials Agreement (CRADA) NASH CRN Vitamin E increased resolution of NASH (from initial definite or borderline NASH) NASH CRN Neither Vitamin E nor Metformin Improved Fibrosis Score To perform a multicenter, double-masked, double-placebo, randomized clinical trial of metformin (500mg BID) or vitamin E (RRR-atocopherol 400 IU BID) versus placebo for the treatment of NAFLD Over-encapsulated generic metformin/placebo Vitamin E/placebo provided by Pharmavite under a Clinical Trials Agreement (CRADA) NASH CRN Specific Aim To perform a multicenter, double-masked, double-placebo, randomized clinical trial of metformin (500mg BID) or vitamin E (RRR-atocopherol 400 IU BID) versus placebo for the treatment of NAFLD Over-encapsulated generic metformin/placebo Vitamin E/placebo provided by Pharmavite under a Clinical Trials Agreement (CRADA) NASH CRN Final Conclusions NAFLD is the most common chronic liver disease in the world & threatens our organ allocation system Vitamin E, Pioglitazone, & Metformin do not improve fibrosis in NAFLD Vitamin E improves ballooning and NAS scores in adults & children Behavior modification & treatment of underlying obesity is imperative www.kampkaana.org Demographics & physical characteristics (n=39) Parameters Mean Gender 25 females 14 males Ethnicity 15 Whites 12 Hispanics 11 Blacks 1 Asian Age (y) 11.9 ± 1.39* Weight (kg) 88.8 ± 18.6 Height (cm) 159.8 ± 7.3 BMI (kg/m2) 34.6 ± 6.1 FFM (kg) 49.8 ± 9.3 FM (kg) 39.1 ± 13.0 FM (%) 43.2 ± 7.4 Wt z-score 2.65 ± 0.60 BMI z-score 2.38 ± 0.31 Wt percentile 98.8 ± 1.9 BMI percentile 98.9 ± 0.9 Changes in anthropometric & body composition post camp 3 FFM (kg) Post Camp - Pre Camp 2 1 0 Wt (kg) BMI 2 (kg/m ) Fat (kg) BMI z-score P<0.01 Fat (%) P<0.01 -1 -2 P<0.01 -3 -4 -5 -6 P<0.01 P<0.01 P<0.01 Changes in IWQOL scores post camp Post Camp - Pre Camp 20 P<0.01 15 10 P<0.02 P<0.01 P<0.03 5 P=0.60 0 Physical Comfort -5 Body Esteem Social Life Family Relations Total Score Post Camp - Pre Camp 0.5 0.0 -0.5 -3.0 1.0 P=0.51 In Pr ter ob pe le rso m n s al In ef fe ct iv en es s An he do ni a N Se ega lf tiv Es e te em To ta lS co re N M ega oo ti d ve Changes in CDI scores post camp P=0.77 P=0.07 -1.0 P<0.05 P=0.10 -1.5 -2.0 -2.5 P=0.94 www.kampkaana.org