Late-Breaking Poster - LB-13. A Phase 2B Double
advertisement

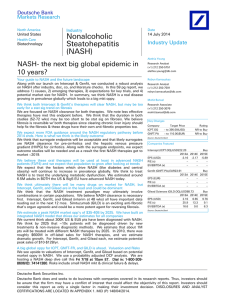
Genotype and clinical characteristics (regardless of fructose consumption) A PHASE 2B MULTICENTER PROSPECTIVE DOUBLE-BLIND PLACEBO CONTROLLED STUDY OF TWO DOSES OF EPA-E IN PATIENTS WITH NONALCOHOLIC STEATOHEPATITIS 2 MD1, 3 4 5 Arun J Sanyal, Manal F. Abdelmalek, MD, MPH , Ayako Suzuki, MD , William Cummings, MD and Mario Chojkier, MD . 1 2 3 Div. of Gastroenterology, Hepatology and Nutrition, Virginia Commonwealth University, Richmond, VA; Div. of Gastroenterology and Hepatology, Duke University, Durham, NC; Div. of Gastroenterology, University of Arkansas for Medical Sciences and Central Arkansas Veterans Healthcare System, Little Rock, AR; 4Dept. of Pathology, Indiana University, Indianapolis, IN; 5 Div. of Gastroenterology and Hepatology, University of California San Diego and VA San Diego Healthcare System, San Diego, CA. Figure 1: A CONSORT diagram of subjects included in the trial Abstract Background and Aims: N3 polyunsaturated fatty acids (PUFA) reduce insulin resistance, lipogenesis and inflammation, the key pathophysiologic features of nonalcoholic steatohepatitis (NASH). Pure ethyl-eicosapentanoic acid (EPA-E) is used as a PUFA agent that improves hypertriglyceridemia. We report the final results of a phase 2b multicenter prospective double-blind randomized placebo controlled trial of EPA-E for NASH. Methods: Subjects with NASH and a NAFLD activity score (NAS) ≥ 4 with a minimum score of 1 each for steatosis and inflammation plus either ballooning or at least stage 1a fibrosis were included. A total of 243 subjects were randomized to receive placebo (n=75), low-dose EPA-E (1800 mg/day) (n=82) or high-dose EPA-E (2700 mg/day) (n=86). The primary efficacy endpoint was a NAS ≤ 3 without worsening of fibrosis or a drop in NASH by 2 or more with contribution from more than one parameter without worsening of fibrosis after 1 year of treatment. Results: The proportion of subjects meeting the primary endpoint (32.7 vs 32.7 vs 31.3% for placebo, low dose- and high dose-EPA-E) were similar. There was no significant effect of EPA-E on steatosis, inflammation, ballooning or fibrosis scores. There were also no significant effects on liver enzymes, insulin resistance, adiponectin, CK18, hsCRP or hyaluronic acid levels. High dose EPA-E decreased triglyceride levels compared to placebo (-4.9 ± 116 vs 11.5 ± 50.9, p=0.03). There were no treatment-related serious adverse events. Conclusions: EPA-E had no significant effect on the histological features of NASH. It is safe and produced a modest improvement in triglyceride levels. Background Nonalcoholic Steatohepatitis (NASH): A major cause of chronic liver disease which may progress to advanced fibrosis, cirrhosis and hepatocellular carcinoma. Associated with obesity, insulin resistance, cardiovascular disease, dyslipidemia, hypertriglyceridemia and a pro-inflammatory state. Is associated with a depletion of n3 polyunsaturated fatty acids (PUFAs) No FDA approved therapies for NASH currently exist. Eicosapentanoic acid (EPA): PUFAs (both n3 and n6) are derived from essential fatty acids and are highly biologically active molecules EPA is decreased across several classes of lipid in subjects with NASH. Decreased EPA is associated with decreased levels of docosahexanoic acid (DHA) (22:6 n3) a downstream product of EPA. Both EPA and DHA are known to improve hypertriglyceridemia, insulin sensitivity and reduce inflammation via effects on a multitude of targets including the sterol response element binding protein (SREBP), IL-6, angiotensin 2 and nitric oxide-mediated signaling. Objectives Determine the efficacy and safety of EPA-E for the treatment of NASH Evaluate the pharmacokinetic profile of EPA and its metabolites after single and multiple doses of EPA-E or placebo Methods Study Centers: 37 sites in North America (Clinical Trials.Gov NCT # 01154985) Study Population: Adults (age 18-70) with biopsy proven NASH within 6 months prior to randomization Less than 3 alcoholic drinks daily (approximately 10 gm alcohol/drink) for the previous 5 years. Histologic Diagnosis of NASH: Defined using NASH CRN criteria (Kleiner et al. Hepatology. 2005). Histologic entry criteria included (1) the presence of possible or definite steatohepatitis, AND (2) a NAFLD activity score (NAS) ≥ 4 with a minimum score of 1 each for steatosis and inflammation plus either ballooning or at least stage 1a sinusoidal fibrosis. Central pathology committee of 4 pathologists Exclusion Criteria: Refusal to provide informed consent Presence of cirrhosis on liver biopsy Decompensated liver disease (ascites, encephalopathy or variceal hemorrhage Serum ALT > 300 IU/L Pregnancy or lactation at the time of screening Serum creatinine > 2 mg/dl Symptomatic cardiovascular or peripheral vascular disease Symptomatic heart failure of New York Heart Association class 2 or higher EKG with a QTc > 450 msec for males and > 470 msec Advanced respiratory disease requiring oxygen therapy History of cerebral or retinal hemorrhage or known bleeding diatheses. Prior bariatric surgery, esophageal banding, and gastric banding Greater than 10% change in weight in the two months prior to entry Alternative causes of steatohepatitis (drugs, alcohol etc) Use of any agent used to treat NASH (vitamin E > 60 IU/day, thiazolidinediones and n3 PUFA > 200 mg/day) within 3 months prior to liver biopsy The presence of other concomitant chronic liver diseases Poorly controlled type 2 diabetes (hemoglobin A1C > 9%) Participation in any intervention trial within 3 months prior to entry Ethyl Eicosapenta (EPA-E or EPADEL®): Is highly purified EPA ethyl ester, has been used in Japan for the past 20 year to treat hyperlipidemia and arteriosclerosis Produces an improvement in hypertriglyceridemia and also lowers total cholesterol Is safe and without reports of serious drug-related adverse events in over 485,000 subjects which receive this drug annually in Japan for the indication of hypertriglyceridemia and atherosclerosis obliterans. Primary One-Year Efficacy Endpoint: NAS ≤ 3 without worsening of fibrosis OR A drop in NAS by ≥ 2 points with contribution from more than one parameter AND no worsening of fibrosis. Rationale for Use of EPA for Treatment of NASH: The beneficial effects of EPA on lipogenesis via SREBP inhibition and reduction of inflammation along with its observed depletion in NASH provide a strong rationale for its use as a treatment of NASH. In a pilot study of subjects with suspected NAFLD, 2700 mg/day of EPA-E decreased ALT levels by 26% in subjects with metabolic syndrome and an ALT > 45 IU/L . Secondary Efficacy Endpoint: Changes from baseline in alanine aminotransferase at 3 and 6 months Changes in the individual histological parameters related to NAFLD Changes in hemoglobin A1C and insulin sensitivity as measured HOMA-IR) Changes in acute phase reactants, levels of cytokeratin 18 (CK18), hyaluronic acid, type IV collagen (7S domain), procollagen III peptide and key cytokines Study Design Prospective, double-blind, placebo-controlled, multi-center, randomized phase 2b clinical trial of two doses (1800 mg/day or 2700 mg/day in three divided doses) of EPA-E vs placebo for treatment of NASH for 12 months. Analysis Statistical Analysis: Cochrane-Armitage test Wilcoxon 2-sample tests Sample size was estimated based on the assumption that the placebo response rate would be 20% while that for EPA-E (1800 mg/day) would be 30% and for EPA-E (2700 mg/day) would be 40%. It also accounted for a 10% drop out rate. A sample size of 210 subjects (70 in each arm) would provide a power of 80% with a one-sided α set at 5%. Differences were considered statistically significant when the p-value(s) were less than 0.05. P-values have not been adjusted for multiple comparisons. Results Results Secondary analyses Table 1: Baseline Patient Characteristics Parameter Age (yrs) Males (n) Caucasian n (%) African American Others BMI (kg/m2) Hemoglobin (gm/dl) WBC (cells/mm3) Platelets (cells x 1000/mm3) Fasting glucose (mg/dl) HOMA-IR Type 2 diabetes (n) Total Cholesterol (mg/dl) LDL-cholesterol (mg/dl) HDL-cholesterol (mg/dl) Triglycerides (mg/dl) AST (IU/l) ALT (IU/l) Alk Phos (IU/l) Bilirubin (mg/dl) Albumin (gm/dl) hsCRP (mg/L) CK18 (U/L) Hyaluronic acid (ng/mL) Type IV collagen (ng/mL) Procollagen III polypeptide (ng/mL) Adiponectin (μg/ml) Placebo N= 75 Mean ± S.D. 50.5 ± 12.4 32 68 (90.7) 3 (4) 4 (5.3) 33.6 ± 5.9 14.2 ± 1.5 6.8 ± 1.9 233 ± 58 115 ± 29.1 9.5 ± 21 15 192 ± 44 117 ± 39 45 ± 11 150 ± 51 67 ± 49 94 ± 65 92 ± 41 0.6 ± 0.3 4.5 ± 0.4 5.8 ± 6.1 886 ± 890 73.8 ± 84 164.9 ± 106 8.3 ± 4.4 5.13 ± 2.9 EPA-E (1800 mg/day) N= 82 47.8 ± 12.5 34 77 (94) 3 (3.7) 2 (2.4) 35.8 ± 6.6 13.9 ± 1.5 6.7 ± 2.3 229 ± 63 110 ± 24 7.9 ± 8.4 24 190 ± 49 108 ± 40 44.5 ± 11.8 183 ± 127 63 ± 37 87 ± 51 80 ± 22 0.5 ± 0.25 4.5 ± 0.26 6.3 ± 6.5 781 ± 655 56.7 ± 81 148.9 ± 66 8.05 ± 5.04 4.7 ± 2.5 EPA-E (2700mg/day) N= 86 47.8 ± 11.1 29 75 (87) 2 (2.3) 9 (10.5) 34.9 ± 6.3 14.1 ± 1.3 6.6 ± 1.7 231 ± 64 117 ± 34 7.4 ± 10.3 15 202 ± 45 121 ± 41 45.6 ± 14.9 178 ± 106 68 ± 43 88 ± 48 89 ± 26 0.54 ± 0.23 4.5 ± 0.28 6.5 ± 6.5 776 ± 634 51.7 ± 57 144 ± 53 7.5 ± 3.7 4.9 ± 2.6 P value n.s. n.s. n.s. n.s. n.s. n.s. n.s. n.s. n.s. n.s. n.s. n.s. n.s. n.s. n.s. n.s. n.s. n.s. n.s. n.s. n.s. n.s. n.s. n.s. n.s. n.s. n.s. Ordinal logistic regression models adjusting for baseline histology, BMI and changes in BMI indicated a significant beneficial effect of EPA-E (i.e., more improvement and less deterioration) in steatosis (OR: 7.9 (95% CI: 1.1-55.4) p=0.03 for low dose EPA-E only) as well as overall NAS (OR10.5 (1.4-81.7) p=0.02 for low dose EPA-E and 6.8 (1.1-40.8) p=0.03 for high dose EPA-E) in women under 50 years of age receiving EPA-E. Multiple linear regression models adjusting for baseline value, BMI and changes in BMI confirmed that the drop in both AST and ALT from baseline to end of study was significantly greater in the placebo arm compared to the high dose EPA-E group (p<0.01 and 0.02 for ALT and AST respectively). Summary EPA-E has also been used to effectively improve dyslipidemia in Japan. However, despite the strong rationale to support its use, it was critical to demonstrate its utility for the treatment of NASH in a rigorously performed clinical trials. EPA-E was safe and well tolerated compared to placebo. EPA-E did not improve any NASH-related parameters and underscores the importance of performing carefully controlled trials to assess the efficacy of pharmacological agents for any disease. The modest effects on serum triglycerides seen in this trial which are less than what has been seen in Japan support this possibility. Limitations Table 2: Histological Outcomes in Efficacy Evaluable Dataset Parameter Placebo N=55 EPA-E (1800 mg/day) N= 55 Proportion of responders* NAS Steatosis Lobular inflammation Cytologic ballooning Fibrosis 32.7 4.7 vs 3.8 1.9 vs 1.5 1.5 vs 1.5 1.2 vs 0.7 1.4 vs 1.5 32.7 4.8 vs 3.7 2.0 vs 1.6 1.5 vs 1.4 1.1 vs 0.7 1.4 vs 1.4 EPA-E (2700 mg/day) N= 64 P value 31.3 4.9 vs 4 2.0 vs 1.6 1.7 vs 1.5 1.2 vs 0.9 1.4 vs 1.4 n.s. n.s. n.s. n.s. n.s. n.s. Table 3: Secondary Endpoints Variable AST (IU/L) ALT (IU/L) Alk Phos (IU/L) Bilirubin (mg/dL) Albumin (gm/dL) HBA1C (%) Glucose (mg/dL) HOMA $ Adiponectin (μg/mL) $ CK18 (U/L) $ Hyaluronic acid (ng/mL) $ Procollagen III peptide (ng/mL) Collagen IV (ng/mL) $ Total cholesterol (mg/dL) LDL cholesterol (mg/dL) HDL cholesterol (mg/dL) Triglycerides (mg/dL) Body Weight (kg) BMI (kg/m2) hsCRP (mg/L) $ Ferritin (ng/mL) $ $ The dose of EPA-E may not have been not high enough for NASH in an American population as dose was selected based on Japanese data . The increased loss of patients to follow-up (25%) may have resulted in the inability to detect a therapeutic response if one was present. Acknowledgements Clinical Centers: Principal Investigators Placebo (N=55) Mean ± S.D. -14.9 ± 45.7 -24.1 ± 48.3 -1.2 ± 17.2 -0.01 ± 0.22 0.06 ± 0.30 0.04 ± 0.43 -0.9 ± 22.0 -0.01 ± 3.52 0.32 ± 1.68 -154 ± 1036 -0.11 ± 54.78 -0.97 ± 3.90 -18.2 ± 51.8 4.5 ± 35.2 0.7 ± 27.5 1.38 ± 9.27 11.5 ± 50.9 -1.17 ± 4.32 -0.37 ± 1.38 -0.33 ± 4.87 -40.7 ± 141.6 Change from Baseline to Month 12 EPA-E 1800 mg/day (N=55) Mean ± S.D. -9.5 ± 33.2 -10.6 ± 44.4 -1.5 ± 14.9 0.02 ± 0.17 0.07 ± 0.26 0.21 ± 0.75 6.7 ± 31.0 0.60 ± 7.22 0.09 ± 0.80 -187 ± 641 -4.38 ± 70.25 -0.99 ± 2.96 -10.3 ± 40.9 4.4 ± 35.7 8.8 ± 27.1 1.42 ± 8.62 -9.5 ± 79.8 0.15 ± 5.55 0.06 ± 2.02 -0.91 ± 3.51 -45.8 ± 168.1 EPA-E 2700 mg/day (N=64) Mean ± S.D. -3.0 ± 41.6 -3.2 ± 51.5* -2.4 ± 15.4 0.01 ± 0.19 0.05 ± 0.23 0.18 ± 0.86 1.0 ± 30.9 -0.86 ± 9.08 0.10 ± 0.99 -61.3 ± 711 -2.10 ± 48.99 -1.07 ± 3.16 1.5 ± 38.5 3.0 ± 29.2 4.4 ± 25.3 -0.02 ± 7.09 -4.9 ± 116.0* -0.35 ± 5.34 -0.12 ± 1.89 -1.12 ± 3.83 -17.7 ± 113.8 These were analyzed using the efficacy evaluable dataset and Wilcoxon two-sample test. *: Everything except for ALT (EPA-E 2700 mg/day vs. Placebo) and Triglycerides (EPA-E 2700 mg/day vs. Placebo) were P value > 0.05. ALT (EPA-E 2700 mg/day vs. Placebo) = 0.0304. Triglycerides (EPA-E 2700 mg/day vs. Placebo) P value = 0.0386 $: Analyzed using fewer # of subjects than the efficacy evaluable dataset due to missing values. The accurate number of subjects is as stated below. [Placebo : EPA-E 1800 mg/day : EPA-E 2700 mg/day], HOMA [N=53 : N=52 : N=59], Adiponectin [N=48 : N=50 : N=56], CK18 [N=49 : N=51 : N=59], Hyaluronic acid [N=47 : N=50 : N=58], Procollagen III peptide [N=47 : N=51 : N=58], Collagen IV [N=50 : N=51 : N=58], hsCRP [N=51 : N=52 : N=59], Ferritin [N=51 : N=52 : N=58] • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • Central Pathology--Indiana University Gastrenterterology Research Consultants: Fredrick Weber • Oscar Cummings Consultants for Clinical Research: Mark Jonas • Muhammad T. Idrees Adobe Gastroenterology Research, LLC: Sam Moussa • Narasimhan P. Agaram NYU Hepatology Associates: Melissa Palmer • Romil Saxena Rhode Island Hospital: Kittichai Promrat University of Texas Health Science Center of Houston; Michael Fallon Scripps Clinic: Paul Pockros Duke University: Manal Abdelmalek Tulane University: Luis Balart Medical Associates Research Group: Michael Bennett University of California San Diego: Mario Chojkier Metropolitan Gastroenterology Group, P.C.: Robert Hardi Nashville Gastrointestinal Specialist: Robert Herring Henry Ford Health Center: Many Ann Huang Funding Support: Virginia Mason Medical Center: Kris Kowdley Mochida Pharmaceuticals, Japan Gastrointestinal Associates, P.A. : Billy Wayne Long The Cleveland Clinic Foundation: Arthur McCullough Digestive Health Specialists: John Phillips Advanced Clinical Research Institute, Inc – Anaheim: Michael Dimicco Digestive Health Specialist of the Southeast: Samuel Tarwater Virginia Commonwealth University Medical College of Virginia: Arun Sanyal Rush University Medical Center: Nikunj Shah Liver Institute of Virginia: Mitchell Shiffman Minnesota Gastroenterology: Colman Smith Advanced Liver Therapies at St. Lukes Eposcopal Hospital: John Vierling Memphis Gastroenterology Group: Lawrence Wruble Gastro One: Zaid Younes Rocky Mountain Clinical Research, LLC – Littleton: Bahri Bilir University of Kentucky: Paul Angulo Southern California Liver Centers: Tarek Hassanein Fundacion de Investigacion de Diego: Maribel Rodriguez-Torres Digestive Medicine Associates: Jeff Gonzalez Brooke Army Medical Center: Stephen Harrison Asheville Gastroenterology Associates: Kimberly Beavers Cedars-Sinai Medical Center: Fred Poordad University of Michigan Cardiovascular Center: Hari Conjeevaram Kelsey-Seybold Clinic: Greg Galler