Acute Management of Myocardial Infarction
advertisement

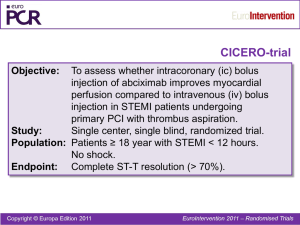
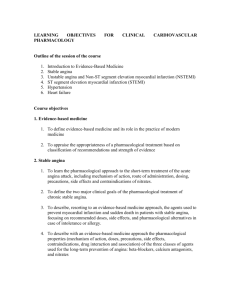
Acute Management of Myocardial Infarction Henry Yao Intern, Royal Melbourne Hospital Introduction • Stable angina • Acute coronary syndrome – STEMI – NSTEACS • NSTEMI • Unstable angina Introduction • Stable angina arise when lumen stenosis >70% → impaired blood supply to heart only during on exertion or increased metabolic demand • Acute coronary syndrome arise when vessel becomes occluded by thrombus – Unstable angina – when atherosclerotic plaque shoot of embolus downstream to cause microinfarct – NSTEMI – when necrosis confined to endocardial layers (most susceptible to ischaemia) – STEMI – when full thickness necrosis of the ventricular wall occurs Introduction • • • • Stable angina – normal ECG, normal troponin Unstable angina – normal troponin NSTEMI – elevated troponin STEMI – elevated ST segment • Criteria for thrombolysis or PCI (i.e. STEMI) – >1mm elevation in 2 contiguous limb leads – >2mm elevation in 2 contiguous precordial leads – New onset LBBB History • All causes central crushing chest pain or tightness radiating • • • • • to arm, neck and jaw Stable angina usually last less than 20 minutes, precipitated by exertion and relieved by rest or nitrates ACS usually lasts more than 20 minutes, sudden onset usually at rest and not relieved by rest All associated with sx of ↓cardiac output – SOB, presyncope or syncope, palpitations All associated with sx of sympathetic activation – nausea, vomiting, sweating, pale, clammy All associated with risk factors – HTN, high cholesterol, DM, smoking, family history Examination • Usually no signs • Signs of precipitants (e.g. anaemia, infection, thyrotoxicosis, arrhythmias), risk factors, other atherosclerotic diseases (PVD, stroke), complications (e.g. MR, CHF) Investigations • Resting ECG (on arrival) – Stable angina – normal – Unstable angina or NSTEMI – ST depression or T wave inversion – STEMI – ST elevation → Q wave (permanent) → T wave inversion (in this order) • Cardiac enzymes – Troponin, CKMB/CK ratio, AST, LDH – Stable angina and unstable angina – normal – NSTEMI, STEMI – raised Investigations • FBE – anaemia, infection • UECR, coagulation study – ability to take contrast and • • undergo PCI FBG, lipid profile (within 24h) – DM, hypercholesterolaemia CXR – r/o aortic dissection, pneumonia, pneumothorax, interstitial lung disease Investigations • Note: Troponin vs CKMB • CKMB – rise in 4hr, elevated for 72hr • Trop – rise in 8hr, elevated for 5 days (trop I) and 10 days • (trop T) If trop –ve → repeat in 8hr → last serial trop done 8hr after sx resolves • CKMB can be used to detect second infarcts Acute Management • • • • Oxygen therapy GTN (½ sublingual tab) Aspirin 300mg IV morphine 2.5~5mg + IV metoclopramide 10mg Hospital Management • Aspirin, GTN, morphine, oxygen if not already given • Monitor oximetry, BP, continuous ECG • 12 lead ECG, IV access, cardiac enzyme STEMI • Reperfuse ASAP (within 12hrs of onset of sx – i.e. before MI is complete): – Antiplatelet therapy (aspirin and clopidogrel ± GPIIb/IIIa inhibitor) – Anticoagulation agent (unfractionated heparin or LMWH) – Immediate PCI or fibrinolytic therapy – PCI has higher reperfusion rate and is better if pt present > 1hr but thrombolysis is gold standard if pt arrive within an hour STEMI • Subsequent management (start during this hospital admission) – Statins, aspirin and clopidogrel, ACEI (or ARB), β-blocker (if CI then CCB) – Anticoagulation therapy to prevent thromboembolism (warfarin for 6mos if large anterior MI, esp if echo show large akinetic/dyskinetic area, aneurysm or mural thrombus) – Nitrates PRN – Cardiac rehabilitation • Antiplatelet post stent – Aspirin for life – Clopidogrel for at least 6wks for metal stent – Clopidogrel for at least 12mos for drug eluting stent – Drug eluting stent have lower early re-stenosis rate c.f. bare metal stent however have a problem of late thrombosis Trop of 0.1 UA and NSTEMI • Stabilize acute coronary lesion • • • – Anti-platelet (aspirin and clopidogrel ± GPIIb/IIIa inhibitor) – Anti-thrombin (UFH or LMWH) – Anti-ischaemia (β-blocker if CI then CCB, consider nitrates, morphine) High risk – urgent angiography ± PCI Low risk – arrange stress tests Subsequent management (start during this hospital admission) – Statins, aspirin and clopidogrel, ACEI (or ARB), βblocker (if CI then CCB) – Nitrates PRN – Cardiac rehabilitation Risk Stratification • TIMI Score (Para Sea) • Historical • – PHx – known CAD (stenosis ≥ 50%) – Age>65 – ≥3 RFs for CAD – Aspirin use in past 7d Presentation – ST segment deviation ≥0.5mm – ↑cardiac enzymes • Recent (≤24hr) severe angina Risk Stratification • Risk stratification of NSTEACS – “HEART DOC” – – – – – – – – – Haemodynaic compromise ECG changes Arrhythmia Renal failure Troponin rise Diabetes mellitus Ongoing chest pain Cardiac bypass anytime or PCI in last 6months Having 1 of these → high risk group Stable Angina • Statins, aspirin (or clopidogrel), ACEI, β-blocker • Nitrates – sx relief or prophylaxis (patch or tablets but must have 8h nitrate free period/day) Wholistic care (all IHD): • Lifestyle change – quit smoking, eat healthy, exercise • more, avoid excessive exertion or stress Risk factor control – HTN, high cholesterol (keep <4mmol/L), DM • Assess depression, level of support Summary • • • • MOAN ECG, troponin, R/O DDx Code AMI Reduce time to PCI QUESTIONS!? Quiz 1 - Complications • Early (0~48h) • • • – Any arrhythmias – worry about AF, VT, VF, CHB – LVF → cardiogenic shock Medium (2~7d) – Any arrhythmias – worry about AF, VT, VF, CHB – LVF → cardiogenic shock – Rupture of papillary muscle (→MR), IV septum, LV wall → acute cardiac failure → APO → death Late (>7d) – Any arrhythmias – worry about AF, VT, VF, CHB – Cardiac failure – LV aneurysm → mural thrombus → thromboembolism – Dressler’s syndrome (3~8wk) – recurrent pericarditis following AMI (Hence why β blockers given initially → prevents arrhythmia as well as rupture of cardiac muscle) Quiz 2 • Contraindication for thrombolysis – – – – Past allergic reaction, past streptokinase use Past stroke – haemorrhagic (ever), ischaemic (6mos) Brain tumour/trauma Recent bleeding or risk of bleeding – e.g. GI bleeding, liver disease – Recent surgery – Hypertension – Pregnancy Quiz 3 • PCI vs CABG – Advantage of PCI – less invasive, less peri-operative stay, morbidity and mortality – Advantage of CABG – higher chance of revascularization – PCI over CABG – single or double vessel disease, inability to tolerate surgery – CABG over PCI – triple vessel disease or left main disease, diabetes mellitus, failed PCI © Copyright The University of Melbourne 2009