Help with Hepatology (Oct 2013)
advertisement

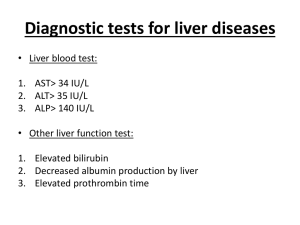
Help with Hepatology Dr Allister J Grant Consultant Hepatologist Leicester Liver Unit University Hospitals Leicester NHS Trust Spire 2013 Abnormal LFT’s in well patients 1) Isolated raise in bilirubin 2) γGT raised 1) ALT rise predominant 2) ALP rise predominant 1) Isolated raise in bilirubin Differential Gilberts vs Haemolysis Gilbertsunconjugated hyperbilirubinaemia HaemolysisUnconjugated hyperbilirubinaemia splenomegaly, anaemia , DCT, haptoglobin, reticulocyte count, film 2) -Glutamyl transpeptidase The high sensitivity and very low specificity seriously hampers the usefulness of this test If ALP is elevated and GGT is elevated then the raise in ALP is likely to be hepatic in origin Elevated in a whole host of liver diseases Drugs/Alcohol Obesity/ dyslipidaemia/ DM CCF Kidney, Pancreas, Prostate 2) ALT rise predominant The majority of abnormal LFTs in asymptomatic people occur in those with: Diabetes or metabolic syndrome (increased risk of NAFLD) Excessive alcohol intake Chronic hepatitis B Chronic hepatitis C Drugs Case - Mr Z 59y Architect Type 2 DM 15 yrs on diet alone BMI 35 Hypertension Amlodipine , Ramipril Minimal Alcohol Mr RP Generally unwell for 2 years Cytopaenia Low Hb/platelets Normal haematological Ix (peripheral consumption) May 07 LGH admission with ataxia/drowsiness Extensive Ix Mr RP CT abdo cirrhotic liver, portal hypertension, splenomegaly OPD referral Alb 28, Pl 65 LFT’s normal, INR 1.5 Imaging compatible with cirrhosis Reversal of sleep pattern, lack of concentration Daytime somnelence, intermittant confusion OGD- varices How common is NAFLD? The most common cause of abnormal liver function tests in the United States. Estimated 30.1 million with NAFLD and 8.6 million with NASH Affects 10-24% of the population 58-74% of the obese population Affects 2.6% of children 23-53% of obese children Non Alcoholic Fatty Liver Disease (NAFLD) Spectrum of Hepatic Pathology Steatohepatitis Steatosis Cirrhosis Hepatocellular carcinoma Diseases Associated with Steatohepatitis 1.Alcoholism 2.Insulin resistance a.Metabolic Syndrome i.Obesity ii.Diabetes iii.Hypertriglyceridemia iv.Hypertension b.Lipoatrophy c.Mauriac Syndrome d.PCOS 3.Disorders of lipid metabolism a.Abetalipoproteinemia b.Hypobetalipoproteinemia c.Andersen’s disease d.Weber-Christian syndrome 4.Total parenteral nutrition 5. HCV (certain genotypes) 6. Untreated coeliac disease 7.Severe weight loss a.Jejuno-ileal bypass b.Gastric bypass c.Severe starvation 8.Iatrogenic a.Amiodarone b.Diltiazem c.Tamoxifen d.Steroids e.HAART f. tetracycline g.glucosamine 9.Refeeding syndrome 10.Exposure to toxic agents a.Environment b.Workplace – Sb,Th,Ba NASH Affects 3.5-5% of the population The rates of progression to cirrhosis have been estimated at between 5% and 20% over 10 years. There aren't any non-invasive means of predicting which patients are at risk of progression, and there are no agreed guidelines on how to monitor progression. Natural history Simple steatosis: relatively benign “liver” prognosis with a risk of developing clinical evidence of cirrhosis over 15–20 years in the order of 1%–2%. NASH and fibrosis: risk of progress to cirrhosis between 0% at 5 years to 12% over 8 years. Cirrhotic: high risk of developing hepatic decompensation and of dying from a liver-related cause including HCC. Initial Investigation Look BMI, DM, HBP, Lipids,FHx, Drugs, Alcohol Liver for risk factors screen (to exclude other diseases) Including Glc/GTT/HbA1c/Lipids/AST Pl, Alb, INR USS Spleen size, fatty liver, collaterals Fibroscan® Electronic platform Integrated computer Ultrasonic signals acquisition Numerical signal processing Stiffness measurement Examinations database Dedicated probes with unique technology Vibrator (50 Hz) US Transducer (3,5 MHz) Fibroscan® (Echosens, Paris, France) Position of probe & explored volume Cylinder of 1 cm wide & 4 cm long From 25 mm to 65 mm below skin surface This volume is at least 100 times bigger than a biopsy sample Results Stiffness (kPa) Median value of 10 shots 3.9 Kilo Pascals IQR * (kPa) Interval around median Contains 50% of valid shots ≤ 25% of median value At least 10 shots Success Rate: ≥ 60% NASH Management 1) All patients should be encouraged to exercise, as there is good evidence that even in the absence of weight loss exercise improves NASH. Obese Patients Weight reducing diet (aim for 10%, 1-2lb per week) In patients with BMI>28 with risk factors, or >30 without risk factors, consider treatment with Orlistat etc. 2) Diabetic Patients Good diabetic control (HbA1c <6.5%) Metformin Thiazolidinediones Dietician for re-education. Diabetologist if glucose control is difficult. NASH Management 3) Patients with Hyperlipidaemia and abnormal LFT’s Dyslipidaemia should be aggressively addressed Dietician Review Hypercholesterolaemia -Statins Hypertriglycerideaemia -Fibrate. Lipid Clinic Avoid Drugs amiodarone, glucocorticoids, methotrexate, nifedipine, synthetic estrogens, tamoxifen Antioxidants? Alcohol Related Deaths E&W 1979-2010 http://www.statistics.gov.uk/cci/nugget.asp?id=1091 Monthly admission rate UHL Alcohol Admissions 2004-8 Spectrum of Alcoholic Liver Disease The most common manifestations of alcoholic liver disease are: Alcoholic steato-hepatitis Acute alcoholic hepatitis Cirrhosis due to alcohol Alcoholic Hepatitis Most florid manifestation of ALD Cholestatic liver disease associated with the long term heavy use of alcohol Often a precursor to the development of cirrhosis More severe forms are associated with a high mortality 1yr mortality after initial hospitalisation is 40% Best treatment Stop drinking Resolution occurs within weeks-months +/- cirrhosis Symptoms Fever Hepatomegaly Jaundice Coagulopathy Features of hepatic decompensation However, milder forms of alcoholic hepatitis often do not cause any symptoms Investigation Biochemistry AST/ALT ratio >1.5 ALT usually <100 IU/ml Raised GT (variable) Raised ALP (variable) Low Albumin (advanced disease) Bilirubin (≥80 mmol/l) Haematology Prolonged INR (advanced disease) Macrocytosis / anaemia Leukocytosis Thrombocytopenia (advanced disease) Glasgow Alcoholic Hepatitis Score Score 1 Age <50 WCC(109/l) <15 Urea (mmol/l)<5 PT ratio <1.5 Bili (mol/l) <125 2 3 ≥ 50 ≥15 ≥5 1.5-2.0 125-250 >2.0 >250 Patients score from 5-12 points. Score >8 was used to define the high risk population and maximised sensitivity and specificity. Survival from Alcoholic Hepatitis Derivation and validation datasets combined – 436 patients Day 1 GAHS <9 GAHS ≥9 28 day survival (%) 84 day survival(%) 87 46 79 40 93 47 86 37 Day 7 GAHS<9 GAHS ≥9 Corticosteroids If the patient has severe alcoholic hepatitis mDF>32, MELD >11, GAHS>8 Therapeutic trial of prednisolone 40mg PO 7 days If no improvement in bilirubin then discontinue Mathurin P Hepatol 2003;38;1363-9 Louvet A Hepatol 2008;45:1348-54 Pentoxifylline PTX is a phosphodiesterase inhibitor which modulates the transcription of the TNFα-gene, lowers blood viscosity and reduces portal hypertension. RCT 101 patients with severe alcoholic hepatitis (mDF>32). Given 400mg tds for 28 days vs placebo Mortality 24% vs 46% at 28 days Significant reduction in hepatorenal syndrome Acriviadis E, Gastro 2000 119;1637-48 3) ALP Elevated Cholestatic Illness (With or without jaundice) Differentiate from Bony ALP GGT, ALP iso-enzymes Investigation of Cholestasis Raised ALP Check GT if isolated rise Dilated bile ducts 1) Stop alcohol Consider MRCP ERCP Other imaging 2) Stop hepatotoxic drugs 3) Advise weight loss if BMI>25 Non-dilated bile ducts 4) Recheck LFT’s after an interval Persistently raised ALP Full liver screen Diagnosis madeTreat disease Non diagnostic Ixconsider Liver biopsy Liver ALP Elevated Cholestatic Illness Acute CBD stones/Gallstones Tumours 1º or 2º Pancreatic pathology Drugs Infiltration SOD Chronic PBC Sclerosing Cholangitis • 1º or 2º NASH α-1 antitrypsin Sarcoid Amyloid HIV Drug Induced Cholestasis Intrahepatic Hepatocellular Cholestasis Intrahepatic Ductular cholestasis Ductopenic Granulomatous Allopurinol Antithyroid agents Augmentin Azathioprine Barbiturates Captopril Carbamezepine Chlorpromazine Chlorpropamide Clindamycin Clofibrate Diltiazem Erythromycin estolate Flucloxacillin Isoniazid Lisinopril Methyltestosterone Oral contraceptives (containing estrogens) Oral hypoglycemics Phenytoin Trimethoprim-sulfamethoxazole The END Allister.J.Grant@uhl-tr.nhs.uk 0116 258 6630 http://hepatologist.sharepoint.com