Cardiopulmonary Physiology
advertisement

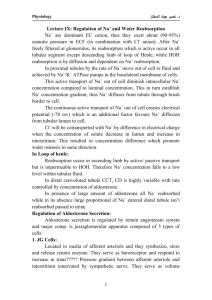
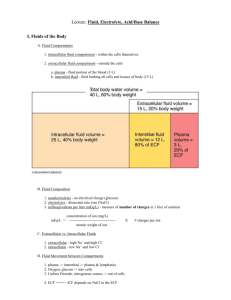
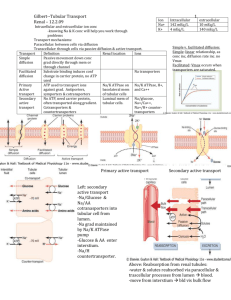
Cardiopulmonary Physiology Millersville University Dr. Larry Reinking Chapter 7 - Renal Considerations As stated at the end of Chapter 1, the kidneys are essential adjuncts to the cardiovascular system. These organs control erythrocyte production (p. 2, chapter 2), direct the release of vasoactive hormones and regulate both the blood composition and volume. The concepts of renal function will be reviewed in this chapter in order to serve as a basis for better understanding the materials in Chapter 8, Regulation of Arterial Blood Pressure. Perhaps the best way to appreciate the role of the kidneys is to consider their blood supply. The kidneys are placed in a strategic position in the circulation and, at rest, receive 2025% of the cardiac output. This is a huge amount of blood for a pair of organs that represent only about 1% of the body mass. It is important to consider that fluid processing, by the kidney, alters blood volume and an altered blood volume, in turn, alters cardiac filling. General Structures The following simplistic diagram illustrates a nephron, the functional working unit of the kidney. Detailed representations of renal structures are shown in the lecture pack, Figures -. efferent arteriole Bowman's caps ule proximal convoluted tubule glomerulus afferent arteriole thin segment (loop of Henle) REABSORPTION FILTRATION dis tal convoluted tubule Figure 7.1 collecting duct Nephron SECRETION CONCENTRATION Combined, both human kidneys have about two million nephrons. There are two basic parts to the nephron, a glomerulus and a renal tubule. The glomerulus, a knot of capillaries, receives blood from the afferent arteriole. Blood leaves the glomerulus via the efferent arteriole which then forms vessels that cover the renal tubule (see the peritubular capillaries and vasa recta in Figures and ). The renal tubule is comprised of Bowman’s capsule, the proximal convoluted tubule, the loop of Henle and the distal convoluted tubule. Many nephrons feed into a collecting duct and, ultimately, many collecting ducts flow into the ureter. In Figure , especially for the juxtamedullary nephron, note the arrangement of the loop of Henle and collecting duct in reference to the renal cortex and medulla. RENAL PROCESSES Filtration - As blood flows through the glomerulus, fluid is filtered into Bowman’s capsule. As we saw in the microcirulation lab, a number of osmotic and hydraulic forces influence this fluid movement. In humans, the glomerular filtration rate is about 125 ml fluid/min. This process is rather indiscriminate since everything except for the cells and large protein molecules filter from the glomerulus into Bowman’s capsule. In other words, many valuable components such as Chapter 7 1 water, ions, amino acids, vitamins and glucose are lost from the blood during filtration. If all of the glomerular filtrate resulted in urine, an individual would excrete (and replace) 180 liters per day. Obviously, further processing steps must recover most of this filtrate. Reabsorption - The proximal convoluted tubule is lined with cells that actively transports solutes from the lumen of the tubule back into the blood (remember that the tubule is cover with peritubular capillaries). This process is specifically referred to as tubular reabsorption. Water movement is linked to this active transport of solutes and results in reabsorption of most of the filtered water. Additional reabsorption of solutes also can occur in other portions of the renal tubule. Sodium for example is mostly reabsorped in the proximal tubule but a small portion is reabsorped in the loop of Henle and in the distal tubule. The reabsorption of sodium in the distal tubule is significant because it is under the control of the adrenal hormone, aldosterone (more on aldosterone, later). Secretion - As the forming urine passes through the renal tubule, some solutes are moved, via active transport, from the blood to the lumen of the tubule. This process is called tubular secretion. In particular, substance such as creatinine, urea, organic acids and potassium are secreted. Potassium secretion in the distal convoluted tubule is of particular interest because it is linked to sodium reabsorption and, thus, is also under the control of aldosterone. Concentration - As the forming urine reaches the end of the distal tubule, the osmotic concentration is about the same as that of the blood (≈300 mosm/liter). If urine was excreted at this concentration, a person consuming a normal amount of fluid would become dehydrated due to a large water loss. In cases of normal hydration, urine must be concentrated before it leaves the kidney. They key to urine concentration is a solute gradient that is established in the tissues of the renal medulla. If we were to measure osmotic concentrations of tissue in the kidneys, we would find that the osmotic concentration in the cortex is about 300 mosm/liter and progressively increases until it reaches 1,200 mosm/liter in the innermost zone of the medulla. Passing through the medullary solute gradient are the loops of Henle, the vasa recta and the collecting ducts. The following diagram depicts this situation: medullary solute gradient in creas ed bloo d os motic co ncentration + brain ADH + = lo op o f Henle vasa recta water moving d own concentration gradient Figure 7.2 Medullary Solute Gradient collecting d uct excreted urine Chapter 7 2 A number of factors contribute to the formation of the medullary solute gradient and include 1) sodium and chloride transport in the upper, thick portion of the loop of Henle, 2) a countercurrent multiplier in the loop of Henle, 3) water impermeability of the distal tubule, 4) urea moving from the collecting duct and 5) the unique, hairpin shape of the vasa recta. The exact mechanism involved in forming this gradient is beyond the scope of this course. As fluid moves down the collecting duct, it encounters an increasingly greater osmotic gradient in the surrounding medullary tissue. Water, in response to the concentration gradient, tends to diffuse out of the collecting ducts into the surrounding tissue. As a result of this water extraction the urine in concentrated. Water, entering the medullary tissue, is then picked up by the vasa recta and returned to the circulation Vasopressin (or antidiuretic hormone, ADH) regulates water extraction from the collecting duct. When increased blood osmotic concentration is sensed in the osmotic center of the brain, ADH is released by the posterior pituitary (neurohypophysis). This hormone travels through the blood, binds to receptors on the collecting ducts and causes increased water permeability. As a result, more water is extracted and the urine becomes more concentrated. In cases of overhydration, ADH is no longer released, the collecting duct becomes less permeable to water and more water is lost to the urine. ADH is also called vasopressin because this molecule promotes increased blood pressure via vasoconstriction (i.e., a vasopressor action). Renin-Angiotensin-Aldosterone System (RAAS) This regulatory system, based in the kidneys, plays a key role in regulating blood sodium concentration, blood potassium concentration, blood volume and blood pressure. Refer, again, to Figure in your lecture packet and note the juxtaglomerular apparatus. The juxtaglomerular apparatus involves a portion of the distal tubule that has folded back toward the glomerulus (called the macula densa) plus a section of cells lining the afferent arteriole (the juxtaglomerular cells): to the glomerulus cross section of the juxtaglomerular apparatus Figure 7.3 juxtaglomerular cells of the afferent arteriole macula dens a of the distal tubule Juxtaglomerular Apparatus afferent arteriole The juxtaglomerular apparatus is able detect changes in sodium levels and renal blood pressure and flow. If sodium levels drop or if pressure or flow in the afferent arteriole drops, renin, a molecule stored in the juxtaglomerular cells in a precursor form, is released into the circulation: Figure 7.4 The Renin-Angiotensin-Aldosterone System Chapter 7 3 aldosterone thirst adren al cortex + Na reabs orption blood press ure + angiotensin I angiotensin II (destroyed by angiotensinase) renin renal blo od flow or pres su re angio tens in converting enzyme + Na vaso con striction ADH plas ma K angiotensinogen brain kidney In the blood, renin converts circulating angiotensinogen into a decapeptide, angiotensin I. As angiotensin I passes through the lungs it is converted into angiotensin II (an octapeptide) by angiotensin converting enzyme (ACE) contained within the endothelial cells of the pulmonary vessels (minor conversion also occurs in other organs). Angiotensin II is a powerful vasoconstrictor and will cause an increase in blood pressure. Note that this action counters the original stimulus of decreased renal blood pressure. Angiotensin II also stimulates thirst via the central nervous system and stimulates ADH release. These actions will eventually increase blood volume. Recall, also, that ADH causes vasoconstriction. A final action of angiotensin II is to stimulate aldosterone production and release from the adrenal cortex. Aldosterone is a steroid hormone that promotes sodium reabsorption in the distal tubule. Increased sodium reabsorption counters the other stimulus that triggers renin release. Increased sodium reabsorption will be accompanied water retention and increased blood volume. Control of Serum Potassium The renin-angiotensin-aldosterone system also plays a crucial role in regulating plasma potassium levels. Recall that hyperkalemia, increased serum potassium, causes cardiac paralysis (chapter 4). An increase in serum potassium directly stimulates the adrenal cortex to produce and release aldosterone. The increased sodium reabsorption in the distal tubule, caused by aldosterone, is linked to potassium secretion; the end result will be a reduced serum potassium concentration. Relation of the RAAS to other Vasoactive Substances The renin-angiotensin-aldosterone system is closely linked to a clotting factor, plasmin and the kallikrein-kinin system. Kinins are vasodilators that are formed from tissue substrates called kininogens. This conversion is promoted by the action of kallikreins, a class of proteolytic enzymes. These interrelationships are shown below: Figure 7.5 The Kallikrein-Kinin System Chapter 7 4 activated clotting Factor XII plas min kinog ens prekallikrein prorenin ?? kallikrein angiotens ino gen renin kinins angiotens in I ACE inactive fragments angiotens in II Diuretics Diuretic therapy is commonly used to treat cardiovascular disorders such as congestive heart failure. The actions of some types of diuretics are listed below. Water, alcohol, caffeine and acidifying salts are typically not used in clinical situations. Keep in mind that when a solute is excreted water will follow. The following table (Table 7.1) summarizes the actions of common diuretics. Chapter 7 5 Table 7.1 Actions of Diuretics Diuretic Agent Water Ethanol Caffeine Acidifying salts (CaCl2, NH4Cl) Carbonic anhydrase inhibitors acetazolamide (Diamox) Metolazone (Zaroxolyn) and thiazides such as chlorothiazide (Diuril) Loop diuretics such as furosemide (Lasix) and ethacrynic acid (Edecrin) Potassium sparing, sodium diuretics spironolactone (Aldactone) Potassium sparing, sodium diuretics triamterene (Dyrenium), amiloride (Colectril) Mechanism of Action Inhibits ADH release Inhibits ADH release Constricts efferent arteriole, glomer. filtration H+ buffered, Na+ excreted with excess anions Decrease H+ excretion, results in increased Na+ and K+ excretion Inhibit Na+/K+/Cl- cotransport in early distal tubule Inhibit Na+/Cl- reabsorption in loop of Henle Decreases Na+/K+ exchange pump in distal tubule by inhibiting aldosterone Decreases Na+/K+ exchange pump in distal tubule by inhibiting Na+ reabsorption Chapter 7 6