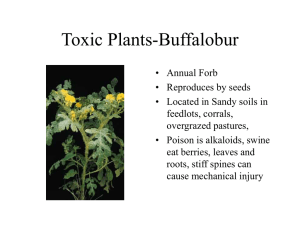
Other poisons
advertisement

POISONS • Cyanide • Carbon monoxide • Arsenic and other metals • Organophosphates & Nerve Agents • Inhalants (Toluene) POISONS Definitions Therapeutic Index: The absolute difference between a tolerable (or therapeutic) concentration and a toxic concentration Poisons: Substances with little or no therapeutic index; we’ll use…‘Toxic’ Index Poisons in our environment •Plant Alkaloids, e.g. Strychnine •Venoms (Insect/Scorpion/Reptilian/Snake) •Mushrooms •amatoxin •Microbial (Botulinus toxin) •Chemical compounds (Cyanide CN) •Metals Cyanide CN Poison in the environment-background levels (sources/natural&industrial) • Many natural sources of CN or CN producing substances (cyanogenic) • Peach pits, Cassava fruit, apple seeds • Vitamin B12 (cyanocobalamin); many metabolic processes produce CN of cyanogenic chemicals; liver possesses enzymatic pathways to detoxify CN Cyanide CN Poison in the environment-background levels • Salts NaCN & KCN used widely (electroplating, gold production and recovery) • Many industrial uses • Rodenticides/Pesticides - fumigants • Nitroprusside used as an antihypertensive (action through effect of NO on relaxing vascular muscle) • CN (HCN) produced by burning synthetic materials Cyanide CN Mechanism of poison’s action • Reversibly binds to a critical component of the respiratory chain (cytochrome c oxidase) causing a reversible stop in oxidative energy production • Other enzyme systems are affected; oxidate energy production is the most important Cyanide CN Mechanism of poison’s action • Without oxidative energy production, glucose and other sugar energy pathways are the only source of energy • Two tissues in particular are obligate oxygen users: Brain and Heart Cyanide CN Onset of action • Toxic effects depend upon “route of administration” and concentration • HCN gas when breathed is the fastest; death can occur within minutes; individuals can be incapacitated in HCN vapour within seconds • Swallowed CN salts or cyanogenic substances take longer (absoprtion/ first pass effect) Cyanide CN Course of toxic effect • • • • CNS stimulation (counter effect) excitation headache and stiff neck giddiness change in breathing pattern (dyspnea); can be confused for hyperventilation • nausea and vomiting Cyanide CN Course of toxic effect • • • • *** asphyxia without cyanosis*** the oxygen remains in the blood and individuals color looks good convulsions and muscular contortion breathing: short inhalation-long exhalation heart races (tachycardia) then slows (bradycardia) Cyanide CN Course of toxic effect • Death due to asphyxia, cardiac and respiratory arrest, with severe brain damage (depending on time to death Cyanide CN Disease states with similar (masking) symptoms • Heart attack • Acute asthma Cyanide CN ‘Toxic’ Index • Relatively small • 50 mg HCN 200-300 mg of NaCN or KCN Response PPM • Immediately fatal 270 • Fatal in 10 min 181 • in 30 min 135 • 1 hr or dangerous to life 110-135 • slight symptoms (e.g. headache) 18-36 Cyanide CN Routes of Absorption • Primarily by breathing vapor or oral administration • Dermal and Occular Cyanide CN Pharmacokinetics – dynamics • Bioavailability: up to 77% by inhalation/ 50% orally/ also dermal (slow) and occular absorption • Vd 0.4 L/kg • t ½ - approximately 1- 2 hr / converted to thiocyante by rhodanase enzyme Cyanide CN Pharmacokinetics – dynamics Blood concentrations • No symptoms • Flushing/tachycardia • Toxicity-death • Coma-Death mg/100 mL 0.01-0.05 0.05-0.1 0.1-0.25 > 0.25 Cyanide CN Pharmacokinetics – dynamics Overdose Treatment/Antidote • Lilly antidote kit (sodium bicarbonate, amyl nitrate and sodium thiosulfate) with 100% oxygen Carbon Monoxide CO Poison in the environment-background levels (sources/natural;industrial) • Primary source is incomplete combustion Carbon Monoxide CO Mechanism of poison’s action • Binds reversibly to hemoglobin - affinity of hemoglobin for CO > O2 Carbon Monoxide CO ‘Toxic’ Index • Based on saturation of whole blood • Endogenous < 1 % • Up to 12% environmental (smokers living in high pollution areas) with no sequelae • Toxicity 12-35% • Fatal > 35% if acute/ >50% if gradual (i.e. accumulation over time.) Carbon Monoxide CO Onset of action • Depends strictly with saturation levels • e.g. Response PPM Headache (20%) 60 min @ 200 20 min @ 500 Death (50%) 80 min @ 500 20 min @ 1500 In an area of high concentration - minutes to incapacitation and death Carbon Monoxide CO Course of toxic effect • Headache, drowsiness, dizziness, NV, blurred vision, confusion, disorientation, dementia, bradycardia-tachycardia, hyperglycemia, seizures, coma, death • Depends on concentration Carbon Monoxide CO Disease states with similar (masking) symptoms • Severe headache often not recognized as a symptom by victims Carbon Monoxide CO Pharmacokinetics – dynamics • Inhalation • Half-life 5-6 hrs. • Binds to hemoglobin carboxyhemoglobin Carbon Monoxide CO Overdose Treatment/Antidote • Oxygen and Hyberbaric pressure chamber • Half-life 5-6 hrs in std atmosphere • 30-90 minutes with 100% oxygen • 30 minutes in hyperbaric chamber METALS Poison in the environment-background levels (sources/natural;industrial) • Most are relatively abundant in the environment or vital ligands for enzymes/co-enzymes and other macromolecules • Metals vital to Health Iron, Copper, Selenium, Zinc • Some Common Toxic Metals Arsenic, Lead, Mercury, Thallium, Nickel, Cadmium, Iron METALS Mechanism of poison’s action • As- Multisystem disease due to inhibition of oxidative energy pathway attacks SH groups • Pb - Same as As (SH groups) • Tl - SH groups + subtitutes for K in ATPase (energy) pump. METALS Mechanism of poison’s action • Fe - Corrosive for GI tract -blood coagulation & cardiovascular collapse • Hg - Binds to thiol and sulfhydryl groups METALS ‘Toxic’ Index Metal Background As 1 ng/mL Fe Hg Pb Tl 65 - 175 mcg/ 100 mL < 2 mcg/100 mL Tolerable intake = 5 mcg/Kg < 10 mcg/100 mL US intake 1980 - 82 = 50 mcg/day < 5 ng/ mL Toxic > 0.5 mg/ 100 mL Fatal > 1 mg/100 mL > 350 mcg/ 100 mL > 1 gm 50 mcg/ 100 mL > 50 mcg/ 100 mL 12-15 mg/Kg or 0.05 mg/100 mL METALS Onset of action • As - 30 min - 2 hr; 200 mg Fatal 24 hr - 4 days • Fe - 30 min - 6 hr; Fatal within 6 hrs or longer • Hg - usually long, slow build up • Pb - usually long, slow build up • Tl - GI symptoms within 12-24 hrs. METALS Course of toxic effect Arsenic • • • • • Nausea &Vomiting, bloody diarrhea, abdominal pain, burning on soles of feet, sensory loss in extremities (lines in nail bed 4-6 weeks; Aldrich-Mees lines) • death due to circulatory collapse METALS Course of toxic effect Fe (Iron) • Primarily GI- affects lining; NV, GI pain, cardiovascular collapse Hg (Mercury) • CNS - tremor and loss of memory Pb (Lead) • CNS - difficulty concentrating, lead (blue-black) line on gums METALS Course of toxic effect Tl (Thallium) • • • • • • Abdominal pain, Nausea, Vomiting & Diarrhea, peripheral neuropathy, Aldrich-Mees lines, *hair loss (2-4 weeks), depressed respiration, delirium, seizure, coma, and death METALS Disease states with similar (masking) symptoms • • • • • As -gastroenteritis, neurological disease Fe - gastroenteritis, but easily detected Hg - classic symptoms Pb - classic symptoms Tl - Viral disease; Guillain - Barre syndrome (often misdiagnosed) METALS Routes of Absorption • Mostly through industrial exposure or surreptitious consumption (poisoning) or suicide. METALS Pharmacokinetics – dynamics Metal As Fe Hg Pb Vd t1/2 Elimination* 0.2 L/Kg 42-48 hrs total body store 3-4 gm hemosiderin in liver ? Elemental form poorly absorbed Iron, Zinc, Ca deficiencies increase absorption 50%; Widely distributed Depends on body burden 40-70 days blood = 28-36 days; bone = 20-30 years renal detected in urine for 30 hrs > 100 ng/mL skin via desquamation; ~ 1 mg/day 1.5 L/Kg *Most metals eliminated by the kidney Tl 2-4 days renal 24 hrs, then fecal METALS Overdose Treatment/Antidote Specific chemicals sequester metals • As - Dimercaprol, Penicillamine, Succimer • Fe -Deferoxamine, Polyethylene glycol • Hg - Dimercaprol, Succimer • Pb - Dimercaprol, Penicillamine, Succimer • Tl - Prussian blue (exchanges K for Tl) not FDA approved; acetylcysteine investigational Organophosphates & Chemical Warfare Nerve Agents Poison in the environment-background levels (sources/natural;industrial) • Organophosphates were designed as pesticides against eukaryotic pests (e.g. they will also affect all pets and family members) • Most warfare nerve agents attack the same metabolic pathways, but take minutes to kill rather than hours - days. • Organochlorines (DDT; 2,4 D) are generally less toxic. Parathion treated Cotton Chemical Nerve Agents Organophosphates & Chemical Warfare Nerve Agents Poison in the environment-background levels (sources/natural;industrial) • Organophosphates: e.g. Parathion, (phosphorothionic acid O,Odiethyl O-(4-nitrophenyl) ester), Diazinon & Malathion • Nerve agents: Sarin (isopropyl Methylphosphonofluoridate), Soman, Tabun, VX (Methylphosphothionic acid S-(2-bis(1Methyl-Ethyl)Amino)Ethyl)O-Ethyl Ester) Organophosphates & Chemical Warfare Nerve Agents Mechanism of poison’s action • • • • • Acetylcholinesterase inhibitors Three stage action Stage 1&2: Reversible for a period of time Stage 3 : Becomes irreversible Acetylcholinesterase has 2 binding sites for these agents; the first can be reversed, the second can not. • Nerve agents may slao penetrate the brain & disrupt GABA transmissions Organophosphates & Chemical Warfare Nerve Agents ‘Toxic’ Index • Small to virtually non-existent • Parathion • Nerve agents: Sarin 4000x more potent than parathion • Lethal inhaled doses of sarin, tabun & soman is 1mg • VX - oily liquid absorbed dermally - 6 mg is lethal Organophosphates & Chemical Warfare Nerve Agents ‘Toxic’ Index • Maximum Control Limits (over 8 hrs) Agent PPM Sarin & Tabun 1 x 10-5 (0.00001) VX 1 x 10-4 (0.0001) CN 36 5 to 6 orders of magnitude (100,000 to 1 M) more potent than Cyanide. Organophosphates & Chemical Warfare Nerve Agents Onset of action • Organophosphates: depends on amount consumed hours to days to weeks & months • Nerve agents: within 5 minutes • Aging of nerve agent-acetylcholinesterase complex (stage 3): Sarin 5 hours Soman 2 minutes Organophosphates & Chemical Warfare Nerve Agents Course of toxic effect • Insomnia fatigue, memory loss, seizures, ataxia, coma, salivation, sweating, tearing, diarrhea, bradycardia, meiosis (pinpoint pupils) muscle twitching, weakness or paralysis. • Death by respiratory arrest Organophosphates & Chemical Warfare Nerve Agents Disease states with similar (masking) symptoms Cholinergic symptoms: – – – – – – salivation, sweating, tearing, diarrhea, bradycardia, meiosis (pinpoint pupils) and memory loss/confusion are classic symptoms for these agents Organophosphates & Chemical Warfare Nerve Agents Routes of Absorption • Readily absorpable by all routes • Inhalation of gas and/or dust • Dermal/Occular absorption (especially VX) • Oral possible Organophosphates & Chemical Warfare Nerve Agents Pharmacokinetics – dynamics • Bioavailability not 100% • hepatic conversion of organophosphates to weakly active compounds • onset of irreversible acetylcholinesterase binding and extent of GABA inhibition (pharmacodynamics) determine toxicity despite kinetics Organophosphates & Chemical Warfare Nerve Agents Pharmacokinetics – dynamics • Organophosphates are cumulative • Vd’s ? • t 1/2 Malathion ~ 3hr others ? Organophosphates & Chemical Warfare Nerve Agents Overdose Treatment/Antidote • Anticholinergic - 1o Atropine • Specific competative inhibitor of stage 2 binding is Pralidoxone (PAM) • PAM binds phosphotase (or related) portion of the toxin and reactivates the ACH ase INHALANTS Poison in the environment-background levels (sources/natural;industrial) • • • • • Toluene, Benzene, Gasolene Chloroform, trichloroethylene CFC’s Anaesthethics Other volatile substances • Most are industrial/medicinal • Focus on Toluene Toluene Mechanism of poison’s action • Toluene - solvent (causes CNS depression and confusion) specific mechanism unknown • Similarities to alcohols • May alter lipid structure of membranes • May effect receptor sites/membrane bound enzymes • May affect cell proteins &/or RNA Toluene ‘Toxic’ Index • Tolerable limits are 50 PPM (188mg/m3 ) • Moderate • Intoxicating - 0.1 to 0.25 mg/mL ...significant tolerance can develop! • Fatal - 0.25 to 1.0 mg/mL • Est. daily dose by inhalation 300 mcg • Lethal oral dose 625 mg/kg Toluene Forensic Caution • Volatile solvent • Sample concentrations can decrease over time • Factors: – storage temperature – Type of cap/tube and tightness of seal – Amount of head space in tube/container Toluene Onset of action • Rapid as with all solvents/volatiles, especially when inhaled, effects begin within minutes • “rapid in - rapid out”, but toluene is highly lipophillic, therefore: “rapid in - delayed out” and extended action Toluene Course of toxic effect • Marked intoxication, mental confusion, slurred speech, inability to concentrate, memory loss, hallucinations, coma, death Toluene Disease states with similar (masking) symptoms • Alcoholic Toluene Routes of Absorption • Absorption via all routes: • Inhalation is fastest (30 minutes, e.g. glue or paint thinner sniffing) • Oral - up to 2 hrs. • Dermal - time? Toluene Pharmacokinetics – dynamics • Vd: unkown but likely high…significantly retained in body • Half life 48-72 hrs, but at least bi-phasic • Initial blood concentrations drop within hours… then level out for days, especially in overdose (e.g. industrial accident) cases. • Eliminated by kidneys, conversion to benzoic acid conjugated to form hippuric acid…excreted for days. Toluene Overdose Treatment/Antidote • Supportive therapy, oxygen if signifcant respiratory depression develops • Many standard treatments e.g. epinephrine contra-indicated, due to combined cardiotoxicity or other toxicities POISONS The Bitter End! METALS ‘Toxic’ Index • Metal Background • As - 1 ng/mL; Toxic > 0.5 mg/ 100 mL; Fatal > 1 mg/100 mL • Fe - 65 - 175 mcg/ 100 mL; Toxic > 350 mcg/ 100 mL • Hg - Background < 2 mcg/100 mL; Toxic > 50 mcg/ 100 mL; Tolerable intake = 5 mcg/Kg • Pb - Background < 10 mcg/100 mL; Toxic > 50 mcg/ 100 mL; US intake 1980-82 = 50 mcg/day • Tl - Background < 5 ng/ mL 12-15 mg/Kg toxic; 0.05 mg/100 mL in blood METALS ‘Toxic’ Index Metal Background Toxic Fatal As 1 ng/mL > 0.5 mg/100 mL > 1 mg/100 mL Fe 65 - 175 mcg/ 100 mL < 2 mcg/100 mL Tolerable intake = 5 mcg/Kg > 350 mcg/ 100 mL > 1 gm Pb < 10 mcg/100 mL US intake ‘80 - 82 = 50 mcg/day > 50 mcg/ 100 mL Tl < 5 ng/ mL 12-15 mg/Kg or 0.05 mg/100 mL Hg 50 mcg/ 100 mL METALS Pharmacokinetics – dynamics • As - Vd = 0.2 L/Kg; t 1/2 = 42-48 hrs; Elimination - renal; detected in urine for 30 hrs > 100 ng/mL • Fe - total body store 3-4 gm; hemosiderin in liver; Elimination - skin via desquamation; ~ 1 mg/day • Hg - Elemental poorly absorbed; t 1/2 = 40-70 days; • Pb - Iron, Zinc, Ca deficiencies increase absorption 50%; Widely distributed; t 1/2 blood = 28-36 days; bone = 2030 years • Tl - Vd = 1.5 L/Kg; t 1/2 = 2-4 days; Elimination - renal 24 hrs, then fecal *Most metals eliminated by the kidney