6 Red Urine a mystery story June 11
advertisement

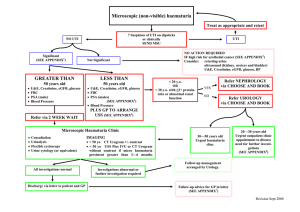
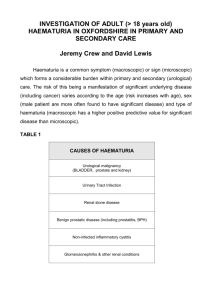
Red Urine – a mystery Shaila Sukthankar Haematuria Common presenting symptom of renal tract disorders Prevalence 0.5 - 6% on population screening in children Haematuria - Definition Urine microscopy RBC > 5/uL in a fresh uncentrifuged specimen RBC > 5 -10/high power field in a midstream sample RBC morphology & presence of casts Case Presentation - May 09 5 years, male Painless gross haematuria – frequent episodes 1 week Initially red, later pink – no clots No history of – – – – – – Fever, dysuria, back/ abdo pain rashes, joint pains Swelling Trauma Bleeding diathesis Recent medication No family h/o renal disease/ deafness/ renal stones/ haematuria Tonsillitis 6 weeks before Examination Normal vitals, BP 110/68, apyrexial No pallor or oedema No bruises or rash Systems review NAD ENT normal Macroscopic haematuria with no features of glomerulonephritis Painless – – – – IgA nephropathy Benign familial nephropathy/ Alport’s syndrome Exercise induced Coagulopathy Painful – – – Infection Trauma Malignancy Haematuria with features of glomerulonephritis Primary renal diseases – – – IgA nephropathy MPGN 1 and 2 Anti GBM disease Secondary renal diseases – – – Postinfectious GN HSP nephritis SLE Initial Investigations FBC, coagulation – normal Urea 6.5, creatinine 40, Albumin 46 Electrolytes, bone profile normal crp <3 Urine microscopy (X2) - <10 WCC, 50-100 RBC, no bacterial growth, trace to 1+ proteinuria Renal USS - NAD Subsequent Investigations C3 and C4 normal ANA, dsDNA negative Immunoglobulins normal ASOT 100 U/mL antiDNASe B 600 U/mL Urine calcium/ creatinine ratio 0.45 Intermittent 3+ blood on dipstick, no proteinuria and well with normal BP over next 4 weeks Urine dipstick Useful screening tool Very sensitive Haematuria - Diagnosis Do not use urine dipstick to diagnose haematuria 12 weeks later (Aug 09)… Recurrence of painless gross haematuria for 1 week Always towards the end of the day – – Clear in the morning Bright red or cola coloured in the evening Worse with exercise and vigorous activity Some discomfort with micturition No other significant positive history Urine microscopy confirmed RBCs in some but not all red urine samples Causes of red or pink urine Haemoglobinuria Myoglobinuria Porphyrins Urates (pink) Foods – beetroot, blackberries Drugs – – Rifampicin (orange) Chloroquine, desferoxamine Possibilities - 1 Recurrent gross haematuria - ? Alport’s/ IgA nephropathy/ thin basement membrane disease ? Bladder pathology (polyp, interstitial cystitis) Exercise induced haematuria ? Not blood (Hburia or myoglobinuria) ? Renal AV malformation Management Repeat haematology, biochemistry and immunology normal Presence of blood without RBCs on some urine samples Myoglobin screen positive on one occasion No infection MR renal angiogram (limited views) – normal Cystoscopy – NAD Family members’ urine microscopy – NAD Review by haematology – no e/o intravascular hemolysis Intermittent painless asymptomatic gross haematuria continues Possibilities - 2 Exercise induced haematuria – exercise test with urine microscopy before and after Nutcracker syndrome – Repeat MR/ direct renal angiogram under GA – parents not keen for further invasive procedures/ GA Evolving nephropathy (IgA/ Alport’s/ TBM) – no indication for biopsy as asymptomatic, normotensive, no proteinuria and normal renal function Nutcracker syndrome Compression of L renal vein between the aorta and sup mesentric artery 40% of children with unexplained haematuria Investigations in a child with haematuria Urine microscopy and culture Urine protein creatinine ratio FBC, coagulation U&E, creatinine, albumin Urine calcium creatinine ratio ASOT, C3 and C4 US renal tract Haematuria - Indications for renal biopsy Associated proteinuria Persistent low C3 Impaired renal function Systemic disease with proteinuria – SLE, HSP, ANCA associated vasculitis Family history suggestive of Alport’s syndrome Recurrent gross haematuria of unknown aetiology with extreme parental anxieties Haematuria - cystoscopy Seldom useful Consider – – – – – Negative preliminary investigations Suspected bladder or urethral pathology Vascular malformations Bladder mass on US To lateralise the source of bleeding Progress – June 10 (12 months on) Well Normally active Occasional brown urine (once in 2-3 months) Lasts for a day, resolves spontaneously Occurs with activity Occurs towards the end of the day Normotensive Parents and child opted for non-invasive observation for now Haematuria - Summary In the absence of proteinuria is not usually indicative of serious pathology Investigation are to be guided by presentation and likely diagnosis In asymptomatic children, ensure serious conditions are not missed and guidelines for further investigations are in place if change in clinical course Latest update (March 11) Well until 3 weeks before review! Febrile coryzal illness with sore throat and recurrence of haematuria Initially bright red, subsequently cola coloured Lasted for 7-10 days, progressively cleared over 2-3 days thereafter Asymptomatic (no headaches, oedema, oliguria etc) DID NOT SEE GP, COMMUNITY NURSES OR HOSPITAL TEAM When attended clinic, back to normal self, urine NAD!! Repeat haematology, biochemistry and immunology normal. ΔΔ??