Hot Topic - Hematuria
advertisement

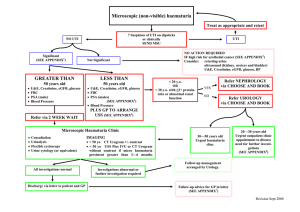
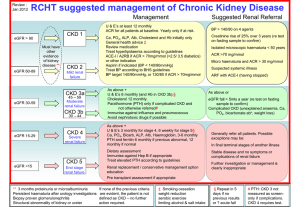
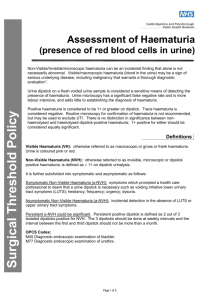
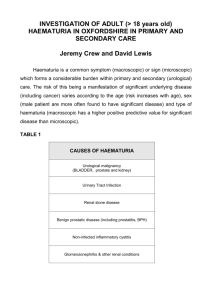
SAIMA USMAN HAEMATURIA Common finding Incidental DEFINING HAEMATURIA Visible haematuria Non visible haematuria (dipstick and microscopic) Indication for urine dipstik testing Lower urinary tract symptoms Upper urinary tract symptoms Diagnosis of hypertension Diabetes(at least annually) Newly detected renal dysfunction(e GFR<60ml/min) Suspected multisystem disease with possible renal involvement. Innocent haematuria Haemoglobinuria Myoglobinuria Menstruation Sexual intercourse Acute intermittent porphyria Food :beet root, black berries, rhubarb Drugs: nitrofurantoin,senna,rifampicin,phenolphthalein,chlo roquine,doxorubicin Chronic lead or mercury poisoning HAEMATURIA UTI typically causes non visible transient haematuria and if simple doesn't require further investigations. Presence of bacterial peroxidases can cause a false positive dipstick test Dipstick testing for blood is less sensitive in the urine with high specific gravity and heavy proteinuria CAUSES OF HAEMATURIA PRE RENAL CAUSES Bleeding diathesis Purpura Atrial fibrillation Leukaemia Infective endocarditis Thrombocytopenia Scurvy haemophilia CAUSES OF HAEMATURIA RENAL CAUSES NEPHROLOGICAL IgA nephropathy Polycystic kidney disease Glomerulonephritis Haemolytic uremic Polyarteritis nodosa syndrome Alport’s syndrome Good pasture’s syndrome Acute pyelonephritis Causes of haematuria UROLOGICAL GENERALIZED Malignancy Benign tumour Trauma Renal toxins Calculus SLE PKD Renal vasculature problems Medullary sponge kidney CAUSES OF HEMATURIA POST RENAL CAUSES BLADDER/PROSTATIC Tumour URETERIC BPH Prostatic cancer Calculus Carcinoma Papilloma schistosomiasis Calculus Cystitis Injury/FB Purpura Schistosomiasis CAUSES OF HAEMATURIA URETHRAL Acute urethritis Calculus Injury Carcinoma Papilloma Urethral meatal ulcer F.B Approach to haematuria Thorough history including Urinary symptoms Recent history (trauma/muscle injury/causes of factitious haematuria/exercise/foreign travel) Systemic features (fever, weight loss) other symptoms(bleeding,bruising) Co-morbidity Drug history Occupation Family history EXAMINATION Anaemia , wt. loss , skin colour, bruising/bleeding General Pulse rate, blood pressure, temp. Vital signs Signs of infective endocarditis, murmur Cardiovascular Lung signs (rare) Respiratory Palpable masses, distended bladder Abdominal Prostatic enlargement-BPH/cancer Rectal examination INVESTIGATING HAEMATURIA Urine MCS To exclude UTI .Red cell cast indicates glomerulonephritis Urine albumin:creatinine ratio Perform if proteinuria on dipstick of 1+ or more. 24 hrs protein collection is rarely necessary Full blood count Anaemia, signs of infection, thrombocytopenia ESR/PV Raised in infection or malignancy U&Es For renal function and eGFR INVESTIGATING HAEMATURIA Clotting screen Remember that haematuria in those on anti coagulants can occur with normal clotting screen PSA Not in context of UTI that may give a false high reading. Measure 4-6 weeks later. Kidney ,Ureter and Bladder X-ray To look for stones Ultrasound scan To look for abnormalities of the renal tract and the kidneys. USS is as sensitive to hydronephrosis and renal masses as IVU and is more cost effective. REFERRAL CRITERIA URGENT (2 WEEKS WAIT) REFERRAL (urology) Visible haematuria (unless GN is suspected) Haematuria with recurrent or persistent UTI in adult over 40 years Persistent non visible haematuria in adult over 50 years. Abdominal mass identified clinically or on imaging that is thought to arise from urinary tract. REFERRAL CRITERIA UROLOGY All patient with symptomatic non-visible haematuria who don't meet the criteria for urgent referral. Patient with persistent asymptomatic non-visible haematuria age 40-50 years. REFERRAL CRITERIA NEPHROLOGY Evidence of decline of eGFR (by >10ml/min in previous 5 years or by >5ml/min in the last year). Stage 4 or 5 kidney disease. Significant proteinuria (ACR 30 or more or PCR 50 or more). Isolated haematuria with hypertension in those under 40 years. Visible haematuria coinciding with intercurrent ,usually upper respiratory, infection. If no cause established Annual assessment(while haematuria persists)of BP, eGFR and ACR/PCR Re referral to urology if; Significant or increasing proteinuria(ACR>30 or PCR>50) Estimated GFR <30ml/min(Confirmed on at least 2 readings and without an identifiable reversible cause) Deteriorating eGFR(>5ml/min in 1 year or>10ml/min in 5 years. .