Lung Function Tests
advertisement

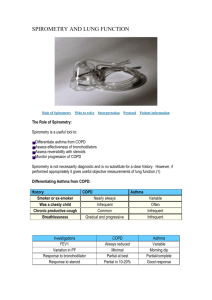
Lung Function Tests Normal and abnormal Prof. J. Hanacek, MD, PhD Introduction Pulmonary function tests are valuable investigations in the management of patients with suspected or previously diagnosed respiratory disease. They aid diagnosis, help monitor response to treatment and can guide decisions regarding further treatment and intervention. The interpretation of pulmonary functions tests requires knowledge of respiratory physiology. Normal or predicted ranges of values are obtained from large population studies of healthy subjects. Values are taken for people matched for age, height, sex and where appropriate ethnicity. PFTS should be performed three times to ensure that the results are reproducible (less than 200ml variation) and accurate. Dynamic studies are performed first (spirometry, flow volume curves, peak expiratory flow rates), followed by lung volumes, bronchodilator testing and finally diffusion capacity. Spirometry is the most frequently used measure of lung function and is a measure of volume against time. It is a simple and quick procedure to perform: patients are asked to take a maximal inspiration and then to forcefully expel air for as long and as quickly as possible (a forced vital capacity manoeuvre). normal spirometry obstructive lung disease restrictive lung disease Parameters of spirographic curve Common Terminology of Spirometry Tests Critical in Diagnosing COPD VC-Vital Capacity - The amount of air that can be forcibly exhaled from your lung after a full inhalation. FVC-Forced Vital Capacity - The amount of air which can be exhaled from the lungs by maximal effort after taking the deepest breath possible. FEV1-Forced Expiratory Volume in One Second - The amount of air which can be forcibly exhaled from the lungs in the first second of a forced exhalation. FEV1/FVC = FEV1-Percent (FEV1%) - The ratio of FEV1 to FVC and tells the clinician what percentage of the total amount of air is exhaled from the lungs during the first second of forced exhalation. PEFR- Peak Expiratory Flow Rate- Measures if treatment is effective in improving airway diseases such as COPD. FEF-Forced Expiratory Flow - A measure of how much air can be exhaled from the lungs. It is an indicator of large airway obstruction. MVV-Maximal Voluntary Ventilation - A value determined by having the patient inhale and exhale as rapidly and fully as possible in 12 seconds. The results reflect the status of the muscles used for breathing, how stiff the lungs are and if there is any resistance in the airways when breathing. This test tells surgeons how strong a patient's lungs are prior to surgery. If patients demonstrate poor performance on this test, it suggests to the doctor that respiratory complications may occur after surgery. Lung volume changes under physiological and pathological conditions GOLD Spirometric Criteria for COPD Severity I. Mild COPD: FEV1/FVC < 0.7 FEV1 >/= 80% predicted The patient is probably unaware that lung function is starting to decline II. Moderate COPD: FEV1/FVC < 0.7 50% </= FEV1 < 80% predicted Symptoms during this stage progress, with shortness of breath developing upon exertion III. Severe COPD: FEV1/FVC < 0.7 30% </= FEV1 < 50% predicted Shortness of breath becomes worse at this stage and COPD exacerbations are common IV. Very Severe COPD: FEV1/FVC < 0.7 FEV1 < 30% predicted or FEV1< 50% predicted with chronic respiratory failure Quality of life at this stage is gravely impaired. COPD exacerbations can be life threatening Flow volume curves are produced when a patient performs a maximal inspiratory manoeuvre which is then followed by a maximal expiratory effort. A graph is produced with a positive expiratory limb and a negative inspiratory limb The maximal flow rate during expiration can also be measured (peak expiratory flow rate PEFR). Furthermore the maximal flow rates between 25%-75% of the vital capacity (FEF25-75%) can also be measured and these provide important information regarding small airway function. Physiological Obstructive Restrictive