Chronic Kidney Disease
advertisement

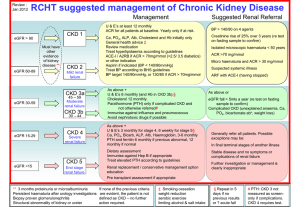
Important Updates in the Early Detection & Management of Chronic Kidney Disease General Practitioner Workshop This workshop was conceived and developed by the Kidney Check Australia Taskforce with particular thanks to A/Prof Robyn Langham & A/Prof Timothy Mathew 2013 Learning Objectives List the eight major risk factors for developing chronic kidney disease (CKD) Explain and apply the changes in recommendations for the detection and staging of CKD focusing primarily on early detection and management Summarise the treatment options to delay progression of kidney disease Outline the importance of developing a system to identify patients at higher risk of CKD for a Kidney Health Check What is CKD? Chronic kidney disease is defined as: Glomerular Filtration Rate (GFR) < 60 mL/min/1.73m2 for ≥3 months with or without evidence of kidney damage. OR Evidence of kidney damage (with or without decreased GFR) for ≥3 months: • • • • albuminuria haematuria after exclusion of urological causes pathological abnormalities anatomical abnormalities. CKD is a major public health problem • 1 in 9 Australian adults has CKD • You can lose up to 90% of your kidney function before experiencing any symptoms • Major risk factor for cardiovascular disease • Usual setting for initial assessment and diagnosis is in general practice • Common, harmful & treatable What is the role of the GP? • early detection and management of CKD • management of early CKD without referral to specialist • assessing and modifying cardiovascular risk factors • treatment to slow or prevent progression of kidney failure • avoiding nephrotoxic drugs Kidney disease in Australia Australians aged ≥ 25 years CKD staging is according to the CKD-EPI equation Stage 5 CKD 19,000 40,000 827,000 856,000 5 MILLION AT RISK Stage 4 CKD Stage 3 CKD Stage 1 – 2 CKD Hypertension Diabetes AusDiab Report, 2001; White et al 2010; Jun 10 ABS data; 2011 ANZDATA report Growth in incidence rate of new treated ESKD and projections to 2020 AIHW, 2011. Projections of the incidence of treated End-Stage Kidney Disease in Australia, 2010-2020 Costs of treating current and new ESKD cases to 2020 $13,000 $12,000 Cumulative Cost ($millions) $11,000 $10,000 In 2009 dollars the cumulative cost of RRT between $11.3 billion and $12.3 billion by the end of 2020 $9,000 $8,000 $7,000 $6,000 $5,000 $4,000 Annual cost of RRT service provision between $1.58 billion and $1.86 in 2020 dollars $3,000 $2,000 $1,000 $0 2009 2010 2011 2012 2013 2014 Cumulative present value costs, Model 1 2015 2016 2017 2018 2019 2020 Cumulative present value costs, Model 2 Cass et al, 2010, economic impact ESKD in Australia, KHA Number of treated or non-treated cases by age group at ESKD onset 2003-2007 No dialysis / transplant dialysis / transplant Source: Linked ANZDATA Registry, AIHW National Mortality Database and National Death Index What’s new in CKD? New CKD staging New recommendations for testing for urine protein New recommendations for eGFR and elderly people with CKD New blood pressure targets The new CKD staging system for Australia 2012 sees the introduction of a new CKD staging system because it: Had a better correlation with progression Factored in albuminuria Resulted in quantification of risk for • CKD progression • CV events What’s new in CKD? Staging of Chronic Kidney Disease Old New Rationale CKD staging Determined by Determined by kidney function Recommended by all system eGFR (eGFR) and the level of Australian and albuminuria in all stages of CKD international guidelines and is a better indicator of overall risk Stage 3 CKD Stage 3 CKD (eGFR 30-59 mL/min/1.73m2) Divided into Stage 3a (eGFR 45-59 mL/min/1.73m2) Stage 3b (eGFR 30-44 mL/min/1.73m2) More accurately reflects risk stratification Risk of ESKD related to baseline proteinuria (dipstick) over 18 year period N= 106,000 Iseki et al, Kidney Int 2003;63:1468-1476 Blue – normal ACR Green – microalbuminuria Red - macroalbuminuria Note log scale on Y axis for Hazard Ratio Adapted from Levey et al, 2010, Kidney International The new Australian CKD staging schema Albuminuria Stage GFR Stage (mL/min/1.73m2) 1 ≥90 2 60-89 3a 45-59 3b 30-44 4 15-29 5 <15 or on dialysis GFR Normal (urine ACR mg/mmol) Male: < 2.5 Female: < 3.5 Not CKD unless haematuria, structural or pathological abnormalities present Microalbuminuria (urine ACR mg/mmol) Male: 2.5-25 Female: 3.5-35 Macroalbuminuria (urine ACR mg/mmol) Male: > 25 Female: > 35 Using the new CKD staging schema ‘CKD Management in General Practice’ booklet has colour-coded action plans for overall risk of • Progression of CKD • Cardiovascular events Normal Low Moderate High The new CKD staging system for Australia CKD Stages are described by both • eGFR & Albuminuria status • Underlying cause of CKD e.g Mrs S is a 55 year old lady with CKD 3b with microalbuminuria secondary to type 2 Diabetes People at increased risk of CKD Eight major risk factors for CKD Diabetes High blood pressure Age over 60 years Smoking Obesity Family history of kidney disease Aboriginal or Torres Strait Islander origin Established cardiovascular disease 1 in 3 Australian adults is at increased risk of CKD due to the above risk factors! How do we detect CKD? New Recommendations for CKD detection Test Kidney Function Blood test for eGFR (creatinine) Test for Albuminuria Urine test for albumin / creatinine ratio (ACR) Test for Hypertension Check patient’s blood pressure Remember… Kidney Health Check Blood Test Urine Test BP Check CKD screening should be undertaken as a part of a systematic chronic disease assessment What is GFR? GFR = Glomerular Filtration Rate • GFR is accepted as the best measure of kidney function • May fall substantially before serum creatinine is outside the normal range • Normal GFR in healthy adults is >90mL/min/1.73m2 and declines with age • A GFR consistently <60mL/min/1.73m2 indicates CKD • A GFR of 60-90mL/min/1.73m2 should not be considered abnormal unless there is evidence of kidney damage. • A fall in GFR always precedes kidney failure • There is no direct way of measuring GFR • GFR can be estimated from serum creatinine using prediction equations • The eGFR is reported by all Australian pathology labs How will eGFR help me and my patients? Early detection & management of CKD: • slows progression • prevents complications • reduces cardiovascular risk • reduces morbidity & mortality Early detection and treatment may reduce the rate of progression of kidney failure and cardiovascular risk by 20 – 50% What’s new in CKD? eGFR – estimated Glomerular Filtration Rate What Old New Rationale eGFR & elderly If aged >70 years, stable eGFR between 45-59 mL/min/1.73m2 may be ok for age in some cases Age-related decision points are not recommended eGFR<60 mL/min/1.73m2 is associated with significantly increased risks of adverse clinical outcomes irrespective of age It is now recommended that the CKD-EPI formula is used to calculate eGFR instead of the previously used MDRD formula This will lead to improved risk stratification and will make little or no difference to your practice What is eGFR? Since 2005 it has been recommended that eGFR be automatically reported with every request for serum creatinine in adults. This is consistent with USA, UK & Australian clinical guidelines CKD-EPI formula is now recommended because: Thoroughly validated equation in adults Superior to other equations and to 24-hour urine collections (when GFR <60 mL/min/1.73m2) No requirement for additional measurements of BSA See calculator at http://www.kidney.org.au Advantages of eGFR eGFR is a more sensitive marker for mild/moderate CKD than creatinine alone Serum creatinine concentration is an insensitive marker for detecting mild to moderate kidney failure Patients may lose 50% or more of their kidney function before the serum creatinine rises above the upper limit of normal Normal serum creatinine measurements do not exclude serious loss of kidney function Comparing eGFR and creatinine CKD 1&2 Serum creatinine CKD 3 120 90 60 GFR mL/min CKD 4 CKD 5 30 Normal Serum Creatinine Level Actual Serum Creatinine Level 0 Limitations of eGFR Clinical situations where eGFR results may be unreliable and/or misleading: • acute changes in kidney function • people on dialysis • exceptional dietary intake (e.g. vegetarian diet, high protein diet, recent consumption of cooked meat, creatine supplements) • extremes of body size • diseases of skeletal muscle, paraplegia or amputees (may overestimate eGFR) or high muscle mass (may underestimate eGFR) • children under the age of 18 years • severe liver disease present • eGFR values above 90 mL/min/1.73m2 • drugs interacting with creatinine excretion (eg fenofibrate, trimethoprim) eGFR and drug dosing • Where an eGFR (using CKD-EPI or MDRD) is on hand it is clinically appropriate to use this to assist drug dosing decision making Recommendation: • Dose reduction of some drugs is recommended for patients with reduced kidney function • Both eGFR (mL/min/1.73m2) and estimated CrCl (mL/min) provide an estimate of relative renal drug clearance • If using eGFR for drug dosing body size should be considered, in addition to referring to the approved Product Information • For drugs with a narrow therapeutic index, therapeutic drug monitoring or a valid marker of drug effect should be used to individualise dosing Remember… Kidney Health Check Blood Test Urine Test BP Check CKD screening should be undertaken as a part of a systematic chronic disease assessment What’s new in CKD? Urine Tests for proteinuria What Old New Urine testing for proteinuria Non-diabetes ? dipstick ? 24 hr urine protein ? PCR ? ACR Diabetes ACR recommended Urine Albumin/ Creatinine ratio (ACR) recommended for everyone Clinical Tip The preferred method for assessment of albuminuria in both diabetes and nondiabetes is urinary ACR measurement in a first void spot specimen Where a first void specimen is not possible or practical, a random spot urine specimen for urine ACR is acceptable Urine Albumin / Creatinine Ratio (ACR) • Exhibits greater sensitivity than protein:creatinine ratio (PCR) • An initial ACR test should be repeated on a first void sample • Albuminuria is present if at least two out of three ACR tests are positive (including the initial test). CKD is present if the albuminuria is persistent for at least three months • Dipsticks for protein in the urine are now no longer recommended for this purpose as their sensitivity and specificity is not optimal Albuminuria • There is an association between albuminuria and progressive kidney disease in population studies • The severity of albuminuria is predictive of outcome • Therapeutic intervention can delay progression of disease and is most effective where there is significant albuminuria • Microalbuminuria is predictive of progressive renal disease in people with diabetes and Indigenous people. • Urine ACR accurately predicts renal and cardiovascular risks in population studies and reduction in urine ACR predicts renoprotective benefit in intervention trials Approximate equivalents between urine ACR & other measure of albumin & protein Kidney Health Check Blood Test Urine Test BP Check CKD screening should be undertaken as a part of a systematic chronic disease assessment What’s new in CKD? Blood Pressure Targets What Old New Blood Pressure Targets People with >1g proteinuria/ day – BP target 125/75 mmHg People with CKD - should maintain a BP consistently below 140/90 mmHg People with CKD (or other conditions) – BP target 130/80 mmHg All other conditions – BP target 140/90 mmHg People with diabetes or microalbuminuria should maintain a BP consistently below 130/80 mmHg Case study Rita Rita is a new patient to your practice • 63 years old • Accountant • History of mild asthma Case study - Rita Past medical history • Overweight (BMI 29) • Mild intermittent asthma • Chronic low back pain • Mild hypertension • Smoker 25 pack year history Family history • Maternal grandmother died of a heart attack in her 60’s but also had a history of ‘kidney problems’ • Mother has type 2 diabetes • Father has angina and hypertension Case study - Rita Smoker: 20-25 cigarettes per day Alcohol: 1-2 glasses of wine 3-4 nights per week Allergies: Nil known Salbutamol 100mcg/dose Medications: as needed Case study - Question Groups at increased risk of CKD Risk factors for CKD High blood pressure Smoking Age over 60 years Family history of kidney disease Diabetes Obesity Aboriginal or Torres Strait Islander origin Established cardiovascular disease Rita has 4 of the 8 Risk Factors CKD risk factors: Diabetes • Patients who have diabetes develop CKD in up to 25% of cases. • 1% of adult Australians develop diabetes each year (Barr et al. 2006, Int. Diab Institute) CKD risk factors: Obesity Being overweight (BMI 25-29 kg/m2 did not increase CKD risk, but all classes of obesity (BMI ≥ 30kg/m2) increased risk *CKD with eGFR <45mL/min/1.73m2 Hallan et al, Am J Kid Dis 2006 Relative Risk of CKD* (95% CI) CKD risk factor: Smoking Smokers with a 25-49 pack-year history had an increased risk of 42% compared with non-smokers and those with >50 pack years had 105% increased risk *CKD with eGFR <45mL/min/1.73m2 Hallan et al, Am J Kid Dis 2006 CKD risk factors: High blood pressure High Blood pressure can damage the small blood vessels in the kidneys. The damaged vessels cannot filter waste products from the blood the way they should. Parenchymal Renal Disease Hypertension Or……damaged kidneys cause high blood pressure and high blood pressure damages kidneys CKD risk factors: Age > 60 Years Relationship of eGFR to age 160 eGFR (mL/min/1.73m2) 140 120 100 80 60 40 2.50% Median 97.50% 20 20-24 25-29 30-34 35-39 40-44 45-49 50-54 55-59 60-64 65-69 70-74 75-79 80-84 85-90 90+ Age (years) Australasian Creatinine Consensus group. MJA 2007; 187(8): 459-463 CKD risk factors: Family history 22.9 23.9 Family history (%) of ESKD in incident dialysis patients 20 14.4 14.6 10 Caucasian men Caucasian women AfricanAmerican men AfricanAmerican women Freedman et al., JASN 1997 CKD risk factors: Aboriginal or Torres Strait Islander Origin Indigenous Australians starting treatment for ESKD Age group (years) Australian Institute of Health and Welfare, 2011 Case study - Answer Rita has 4 risk factors for CKD • Smoking • Age over 60 • Family history • High blood pressure Case study - Question Who should be tested for kidney disease? Risk Factor Recommended Tests Frequency Urine ACR eGFR Blood Pressure Every 1-2 years* Smoker Diabetes Hypertension Obesity Established cardiovascular disease Family history of CKD Aboriginal or Torres Strait Islander origin aged over 30 years *yearly for people with diabetes or hypertension If an individual has multiple risk factors, follow the more frequent regime Case study - Rita You determine that Rita should have a kidney health check every year Kidney Health Check Blood Test Creatinine & eGFR Urine Test Albumin / Creatinine Ratio (ACR) to check for albuminuria BP Check Blood pressure should be consistently below 140/90 mmHg If all 3 tests are normal then the kidneys are in good shape and need only be tested again as indicated by the applicable risk factors Case study - Rita Rita’s Kidney Health Check Results Creatinine 118 µmol/L eGFR 55 mL/min/1.73m2 Urine ACR 5.7 mg/mmol Blood Pressure 155 / 95 mmHg Case study - Rita Albuminuria Stage GFR Stage GFR (mL/min/1. 73m2) Normal (urine ACR mg/mmol) Male: < 2.5 Female: < 3.5 1 ≥90 2 60-89 Not CKD unless haematuria, structural or pathological abnormalities present 3a 45-59 Microalbuminuria Macroalbuminuria (urine ACR (urine ACR mg/mmol) mg/mmol) Male: 2.5-25 Male: > 25 Female: 3.5-35 Female: > 35 RITA’S RESULTS PUT HER HERE 3b 30-44 4 15-29 5 <15 or on dialysis Case study - Question Not yet! Case study - Rita To classify Rita as having CKD, her urine ACR & eGFR will need to be repeated • If the first ACR is a random spot, then repeat tests should ideally be first morning void specimens • CKD is present if at least 2 out of 3 ACR tests (including the initial test) in the next three months are positive • When initial eGFR is <60 mL/min/1.73m2 consider clinical situations where eGFR results may be unreliable/misleading • To confirm CKD, the repeat eGFR in 3 months time should also be below 60mL/min/1.73m2 Repeating the urine ACR Factors other than CKD know to increase urine albumin excretion… Urinary Tract Infection High dietary protein intake Congestive cardiac failure Acute febrile illness Heavy exercise within 24 hours Menstruation or vaginal discharge Drugs (especially NSAIDs) Case study - Question Rita comes back to see you three months later and you repeat her urine ACR, eGFR and blood pressure… Test 1st Visit eGFR 55 mL/min/1.73m2 Urine ACR 5.7 mg/mmol BP 155/95 mmHg This Visit 52 mL/min/1.73m2 8.4 mg/mmol 160/95 mmHg Case study - Rita You can now diagnose Rita as having CKD stage 3a with microalbuminuria Albuminuria Stage GFR Stage GFR (mL/min/1.73m2) 1 ≥90 2 60-89 3a 45-59 3b 30-44 4 15-29 5 <15 or on dialysis Normal (urine ACR mg/mmol) Male: < 2.5 Female: < 3.5 Microalbuminuria (urine ACR mg/mmol) Male: 2.5-25 Female: 3.5-35 Not CKD unless haematuria, structural or pathological abnormalities present RITA FITS HERE Macroalbuminuria (urine ACR mg/mmol) Male: > 25 Female: > 35 Case study - Rita Orange Clinical Action Plan eGFR 30-59 mL/min/1.73m2 with microalbuminuria or eGFR 30-44 with normoalbuminuria Goals of Management • • • • • Investigations to exclude treatable disease Reduce progression of disease Reduce cardiovascular risk Early detection & management of complications Avoidance of nephrotoxic medications or volume depletion • Adjustment of medication doses to levels appropriate for kidney function • Appropriate referral to a Nephrologist Case study - Rita Orange Clinical Action Plan eGFR 30-59 mL/min/1.73m2 with microalbuminuria or eGFR 30-44 with normoalbuminuria Monitoring 3-6 monthly clinical review Blood pressure Clinical assessment Weight Urine ACR Biochemical profile including urea, creatinine, electrolytes Laboratory eGFR assessment HbA1c (for people with diabetes) Fasting lipids Full blood count Calcium and phosphate Parathyroid hormone (6-12 monthly if eGFR <45 mL/min/1.73m2) Case study - Rita Orange Clinical Action Plan eGFR 30-59 mL/min/1.73m2 with microalbuminuria or eGFR 30-44 with normoalbuminuria It is also important to consider… • • • • • Absolute Cardiovascular Risk assessment Lifestyle modification Blood pressure reduction Lipid lowering treatments Glycaemic control Case study - Question Cardiovascular risk reduction • Individuals with CKD have a 2-3 fold greater risk of cardiac death than individuals without CKD • People with CKD are at least 20 times more likely to die from cardiovascular disease than survive to need dialysis or transplant • CKD is one of the most potent known risk factors for cardiovascular disease • It is important to calculate Rita’s cardiovascular risk using the Australian cardiovascular risk tool at www.cvdcheck.org.au Australian Cardiovascular Risk Tool Rita’s Cardiovascular Risk (www.cvdcheck.org.au) • The tool is approved by NH&MRC • If Rita had moderate to severe CKD defined as eGFR <45 mL/min/1.73m2 or macroalbuminuria (ACR >25mg/mmol men; >35mg/mmol women) she would be at the highest CVD risk and in this case the tool should not be applied Blood pressure reduction • CKD can cause and aggravate hypertension and hypertension can contribute to the progression of CKD • Reducing blood pressure to below target levels is one of the most important goals of CKD management • ACE inhibitor or ARB is recommended first line therapy • Combined therapy of ACE & ARB is not recommended • Maximal tolerated doses of ACE inhibitor or ARB is recommended • Hypertension may be difficult to control and multiple (3-4) medications are frequently required Rita has stage 3a CKD with microalbuminuria so her blood pressure needs to be maintained consistently below 130/80 mmHg Blood pressure reduction Clinical Tips • ACE inhibitors and ARBs can cause a reversible reduction in GFR when treatment initiated • If the reduction is less than 25% and stabilises within two months of starting therapy, the ACE inhibitor or ARB should be continued • If the reduction in GFR exceeds 25% below the baseline value, the ACE inhibitor or ARB should be ceased and consideration given to referral to a Nephrologist for bilateral renal artery stenosis Adequate BP management delays the progression of CKD 160/95 If Rita’s blood pressure was consistently below target, the GFR loss per year would be reduced by 80% Bakris et al., Am J Kid Disease, 2000 Lifestyle modification Lifestyle approaches are essential in reducing the overall cardiovascular risk the key elements are: ‘SNAP’ (smoking, nutrition, alcohol, physical activity) Stop smoking A low calorie diet to reduce BMI A low salt diet Weight reduction A reduction in alcohol intake Physical activity Lifestyle modification effects on BP Modification Recommendation Approx SBP reduction Weight reduction BMI 18-24.9 kg/m2 5-20 mmHg / 10kg lost Dietary salt restriction <100 mmol/day 2-8 mmHg DASH* diet Fruit, vegies, low saturated and total fat 8-14 mmHg Physical activity Aerobic activity for 30mins most days 4-9 mmHg Moderate alcohol consumption only 1-2 standard drinks/day 2-4 mmHg * Dietary Approaches to Stop Hypertension Lipid lowering & glycaemic control Lipids • Margaret’s lipids should be assessed • Lipid-lowering treatment should be considered for CVD risk reduction Glycaemic control • Margaret’s glycaemic control should be assessed • For people with diabetes, blood glucose control significantly reduces the risk of developing CKD, and in those with CKD reduces the rate of progression Case study - Question Referral to a Nephrologist is recommended if: • eGFR <30mL/min/1.73m2 • Persistent significant albuminuria (urine ACR ≥ 30mg/mmol) • Rapidly declining eGFR from a baseline of <60 mL/min/1.73m2 (a decline of >5mL/min/1.73m2 over a six-month period which is confirmed on at least three separate readings) • CKD and hypertension that is hard to get to target despite at least three anti-hypertensive agents • glomerular haematuria with macroalbuminuria Anyone with an acute presentation and signs of acute nephritis (oliguria, haematuria, acute hypertension, and oedema) should be regarded as a medical emergency and referred without delay Clinical tip When referring to a Nephrologist ensure patient has had a recent urine ACR, current blood chemistry and haematology and a urinary tract ultrasound. Referral is NOT usually necessary if: • Stable eGFR ≥30 mL/min/1.73m2 • Urine ACR < 30mg/mmol (with no haematuria) • Controlled blood pressure The decision to refer or not must always be individualised and particularly in younger patients the indications for referral may be less stringent. Useful Tips Pay attention to CVD risk reduction Consider discussing management issues with a Nephrologist in cases where uncertainty regarding referral exists. Don’t refer to Nephrologist if targets of therapy are achieved Spiral CT angiogram for hypertension is not recommended without specialty advice Case study – Action plan Orange Clinical Action Plan eGFR 30-59 mL/min/1.73m2 with microalbuminuria or eGFR 30-44 with normoalbuminuria • Follow the ‘Orange’ clinical action plan (found in ‘CKD management in General Practice’ 2nd ed) • Cardiovascular risk reduction • Blood Pressure should be consistently below 130/80 mmHg – use of ACE or ARB as appropriate • Lifestyle modification • Avoid nephrotoxic medications • Adjust dose of other medications to levels appropriate for her kidney function • No need for Nephrology referral at this stage • Continue to monitor 3-6 monthly Treatment target for people with CKD Parameter Target Blood Pressure ≤ 140/90 mmHg or ≤ 130/80 mmHg if albuminuria is present (ACR > 2.5 mg/mmol males; >3.5 mg/mmol females) Treatment Lifestyle modification ACE inhibitor or ARB Albuminuria >50% reduction of baseline value ACE inhibitor or ARB Cholesterol Total < 4.0 mmol/L LDL < 2.5 mmol/L Dietary advice statins Blood glucose (for people with HbA1c <7.0% / 53 mmol/mol diabetes) Lifestyle modification Oral hypoglycaemic Insulin Case study - Question CKD diagnosis, management & patient outcomes The diagnosis of CKD brings with it the need to identify risk reduction measures both for kidney and cardiovascular diseases • Treatment targets and choices of therapy may differ with a CKD diagnosis • Early detection and management of CKD complications • Greater consideration of any prescribing - avoidance of nephrotoxic medications and ensuring dosages of other prescribed drugs are appropriate for the level of kidney function • Timely referral of CKD patients to a Nephrologist for more severe CKD or complications Summary… • CKD is common, harmful and treatable • Early detection is beneficial • Systematically identify patients at high risk of CKD (the 8 risk factors) • Perform a Kidney Health Check (urine ACR, eGFR, blood pressure) on at risk patients • CKD is present if 2 /3 urine ACR tests in 3 month period are positive • Repeat the eGFR if <60mL/min/1.73m2 • Maintain blood pressure consistently below the relevant threshold • Refer to the CKD staging table and clinical action plans in ‘CKD Management in General Practice (2nd ed)’ • GPs play a vital role in the management of CKD • Most CKD patients can be managed in general practice Remember… New CKD staging New recommendations for testing for urine protein New recommendations for eGFR and elderly people with CKD New blood pressure targets Further resources… CKD Management in General Practice 2012 Guidelines booklet New Edition! now available at www.kcat.org.au Kidney Health Information Service • Free call information service for people living with / affected by kidney disease Join the Kidney Community… KIDNEY COMMUNITY members receive a monthly newsletter from KHA allowing you to access: Information and invitations to KHA's education and support activities Updates on medical research in kidney disease Updates on clinical trials and research opportunities Information on advocacy opportunities and government relations issues Information on community and corporate events held by Kidney Health Australia To join the kidney community, email community@kidney.org.au Use of eGFR in different ethnic populations recommendations • The CKD-EPI formula is a useful tool to estimate GFR in all people, including various ethnic populations • The CKD-EPI formula has been validated as a tool to estimate GFR in some non-Caucasian populations, including South-East Asian, African, Indian and Chinese individuals living in Western countries • The different methods to estimate GFR from serum creatinine concentration have not been validated in Indigenous Australians, although these studies are currently underway Australasian Creatinine Consensus statement, 2012 Urine tests Albuminuria or Proteinuria? That is the question!! • The term albuminuria includes increased urinary excretion of albumin and increased urinary excretion of other proteins • It is very rare for a patient to have increased excretion of non-albumin proteins without concomitant increased excretion of albumin • Excessive amounts of proteins in the urine are a key marker of kidney damage and of increased renal and cardiovascular disease risk • These proteins are mainly albumin (albuminuria), but also consist of low molecular weight immunoglobulin, lysozyme, insulin and beta-2 microglobulin Australasian Proteinuria Consensus statement, 2012
![Risk Adjustment Factor [RAF]](http://s2.studylib.net/store/data/005748329_1-97f04b2983127ae4930cafa389444167-300x300.png)