AEDs - BC Epilepsy Society
advertisement

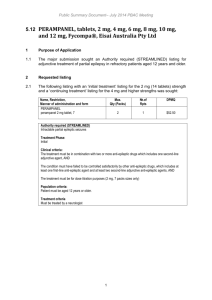
AEDs Martin del Campo MD UHN Toronto, Ont. Disclosures • Speakers Bureau • Ad-boards: – UCB Canada – Boehringer-Ingelheim Outline • Review the new AEDs including Lacosamide • Canadian experience with Lacosamide • Example cases Old vs New The Bad News 470 patients who never received treatment before 222 controlled on the 1st AED (47%) 151 received old drug 71 received a new drug 248 not controlled 168 received an old drug 80 received a new drug 18 responded to a 3rd or multiple drugs (4%) 61 responded to a 2nd AED (13%) •At the last visit 423 patients were on a single AED (68% seizurefree) 53 patients took 2 AED’s (23% seizure-free) 5 patients were on 3 AED’s (none were seizure-free) Kwan, P. and Brodie, M. NEJM 2000; 342: 314-319 Lamotrigine (Lamictal) • • • • • • Good “broad spectrum” AED BID dosing (soon to be OD) Useful as mood stabilizer Metabolism inhibited by VPA Insomnia Skin rash - SJS Lamotrigine (Lamictal) • 5/564 incidence of oral clefts (3 palate, 2 lip) in North American registry • 4/1623 had oral cleft in other registries • Non-teratogenic in doses <200 mg/day (2.6% mono, 10.8% with VPA) Holmes LB et al. Birth Defects Research (Part A); 2006; v76:5 Gabapentin (Neurontin) • • • • • • • Structural analog of GABA Weak AED (30% responder rate) Mode of action unknown Excreted unchanged in urine No drug interactions Quick titration Dizziness, fatigue Topiramate (Topamax) • • • • • Various mechanisms of action Minimally protein-bound Plasma levels ‘d by PHT, CBZ and VPA Partial renal excretion Responder rate 30-50% in partial onset or primarily generalized convulsive Sz’s • Useful in Lennox-Gastaut and infantile spasms • Weight loss, renal stones, oligohydrosis, hallucinations, cognitive impairment • Rare acute narrow-angle glaucoma. Vigabatrin (Sabril) • • • • Another GABA look-alike Designed as a GABA transaminase inhibitor Excreted unchanged in urine GABA levels elevated 120 hrs after single dose • Responder rates inferior to CBZ • Decreases PHT and CBZ levels • 20-30% incidence of visual field constriction Clobazam (Frisium) • • • • • 1,5 benzodiazepine Active metabolite: desmethylclobazam GABAa agonist Efficacy in myoclonic and absence status Usually used as adjunct for partial Sz’s with or without generalization • Tachyphylaxis • Sometimes difficult to taper down Oxcarbazepine (Trileptal) • • • • • CBZ analogue Converted to MHD, active metabolite Renal excretion Traditional AED’s induce its metabolism 25% of pts with CBZ hypersensitivity will react to OXC • No reports of aplastic anemia • hypoNa especially in older pts Oxcarbazepine (Trileptal) • • • • 50-60% responder rate 12% Sz-free Indicated as monotherapy Not on ODB or LU Levetiracetam (Keppra) • Plasma half-life: 6 to 8 hours in adults • Steady state: after 2 days of BID dosing • Renal elimination – 66% eliminated as unchanged drug – Correlated with creatinine clearance Levetiracetam (Keppra) • No interaction with other AEDs included in placebo-controlled clinical studies in patients with epilepsy1 • No interaction with phenytoin2 and valproic acid3 confirmed by clinical pharmacokinetic studies 1. Keppra® Product Monograph 2. Browne TR et al. J Clin Pharmacol 2000;40:590-5. 3. Coupez R et al. Epilepsia 2003;44(2):171-8. Responder Rate % of patients with 50% reduction in Sz frequency 45 *p<0.001 vs. placebo * 40 % of Patients 35 30 25 42.1 20 15 10 5 16.7 0 Placebo (n=105) Ben-Menachem et al. Epilepsia 2000;41:1276-83. LEV 3000 mg/day (n=181) AEDs: Molecular and Cellular Mechanisms Phenytoin, Carbamazepine – Block voltage-dependent sodium channels at high firing frequencies Barbiturates – Prolong GABA-mediated chloride channel openings – Some blockade of voltage-dependent sodium channels Benzodiazepines – Increase frequency of GABA-mediated chloride channel openings AEDs: Molecular and Cellular Mechanisms Gabapentin – Increases neuronal GABA concentration – Enhances GABA mediated inhibition Lamotrigine – Blocks voltage-dependent sodium channels at high firing frequencies – May interfere with pathologic glutamate release AEDs: Molecular and Cellular Mechanisms Ethosuximide – Blocks low threshold, “transient” (T-type) calcium channels in thalamic neurons Valproate – May enhance GABA transmission in specific circuits – Blocks voltage-dependent sodium channels Vigabatrin – Irreversibly inhibits GABA-transaminase AEDs: Molecular and Cellular Mechanisms Topiramate – Blocks voltage-dependent sodium channels at high firing frequencies – Increases frequency at which GABA opens Clchannels (different site than benzodiazepines) – Antagonizes glutamate action at AMPA/kainate receptor subtype – Inhibition of carbonic anydrase AEDs: Molecular and Cellular Mechanisms Levetiracetam – Binding of reversible saturable specific binding site – Reduces high-voltage- activated Ca2+ currents – Reverses inhibition of GABA and glycine gated currents induced by negative allosteric modulators Oxcarbazepine – Blocks voltage-dependent sodium channels at high firing frequencies – Exerts effect on K+ channels Lacosamide: Metabolism and Elimination About 95% of dose excreted in urine 40% as unchanged lacosamide ~30% as O-desmethyl metabolite (no known pharmacological activity) CYP2C19 enzyme responsible for O-desmethyl metabolite No clinical difference in pharmacokinetics in poor vs. extensive metabolizers for CYP2C19 No clinical relevant changes in pharmacokinetics with omeprazole (CYP2C19 inhibitor) t½: ~13 hours (steady-state achieved in 3 days) Low intra- and inter-subject variability EU SmPC; Doty 2007 Pharmacokinetics of Lacosamide: Special Patient Populations and Drug-Drug Interaction • Mild and moderate renal impairment: No dose adjustment needed – Maximum dose of 300mg/day recommended for patients with severe renal impairment (CLCR ≤30 mL/min) or end-stage renal disease. – Supplement of up to 50% of the divided daily dose directly after the end of hemodialysis is recommended. – In all patients with renal and/or hepatic impairment, dose titration should be performed with caution. • Low potential for drug-drug interactions – No clinical relevant changes in the plasma concentrations of concomitant AED’s (carbamazepine, valproic acid, phenytoin, gabapentin, lamotrigine, levetiracetam, oxcarbazepine or zonisamide). – No clinical relevant interaction with digoxin, metformin, omeprazole (CYP2C19 inhibitor), or ethinyl estradiol + levonorgestrel-containing oral contraceptives. – Caution should be exercised when VIMPAT is given with other drugs that prolong the PR interval (eg. carbamazepine, pregabalin, lamotrigine or beta-blockers), and in patients treated with class I anti-arrhythmic drugs as further PR prolongation is possible. UCB data on file; Canadian Product Monograph. Pivotal trials: Patient demographics and baseline characteristics (ITT) • 1294 patients received trial medication and had ≥1 post-baseline efficacy assessment (ITT) – Mean age: 38.6 years – 51.1% female – 91.7% Caucasian – BMI: 26.8 kg/m2 – Time since diagnosis 23.7 years – Lifetime use of AEDs • 32.2% tried 4 to 6 • 45.2% tried 7 or more – Number of concomitant AEDs • 1 AED: 15.5% • 2 AEDs: 62.4% • 3 AEDs: 22.0% AED=antiepileptic drug; BMI=body mass index ITT= all patients with ≥1 post-baseline efficacy assessment 24 UCB data on file Pivotal trials: Seizure freedom during maintenance (Pooled data) Seizure-free rates for completers 14 14 12 12 Median change in percentage of seizurefree days during maintenance phase 10 8 6 4.8% 4 2 2.7% 3.3% Median increase (%) Seizure-free patients (%) 12.1% 9.3% 10 7.4% 8 6 5.4% 4 2 0.9% 0 0 PBO n=326 200 mg n=225 400 mg n=366 Lacosamide 600 mg n=124 PBO n=337 200 mg n=244 400 mg n=393 Lacosamide 600 mg n=142 Rosenfeld study: ≥50% responder rate N=370 Patients responding (%) 70 65.5 60 60.7 57.7 55.4 50 48.3 40 47.4 44.2 30 20 10 0 n=370 >0−6 n=326 >6−12 n=284 n=248 >12−18 >18−24 Months n=224 >24−30 n=206 >30 n=370 Treatment period Percentages were based on the number of patients in each modal dose group with an evaluable responder status during the relative time interval. Responders were defined as patients who experienced ≥50% reduction in seizure frequency during the time interval from baseline (where baseline was from the previous trial). A month was defined as 28 days. 26 Pivotal Trials Pooled Results: ≥ 50% Responder Rate During Maintenance By Dose (ITT) 45% Patients Responding (%) 40% 35% *P <.05; ** P <.001 versus placebo N = 1294 * ** ** 40% 40% LCM 400 mg/day LCM 600 mg/day § 34% 30% 25% 20% 23% 15% 10% 5% 0% Placebo n = 359 LCM 200 mg/day n = 267 n = 466 n = 202 ITT = all randomized patients receiving ≥1 dose of trial medication with ≥1 post-baseline efficacy assessment,; § Lacosamide is approved up to a dose of 400 mg/day Chung AES 2008 Pooled Pivotal Trials: Most Common AEs During Titration and Maintenance* Titration Maintenance Placebo n = 364 % Lacosamide n = 944 % Placebo n = 337 % Lacosamide n = 781 % Dizziness 7 25 2 8 Headache 6 9 5 6 Nausea 4 9 1 3 Diplopia 1 9 1 3 Vomiting 2 8 1 4 Fatigue 5 8 1 2 Coordination Abnormal 1 7 <1 3 Vision Blurred 2 7 1 2 Tremor 3 5 1 2 Nystagmus 3 4 1 1 Adverse Event, MedDRA Preferred Term * Safety population, N = 1308. Lacosamide in Canada Patient characteristics Age (yrs) 19-63, avg. 32.5, med. 19.5 Gender 46 F, 38 M Duration of epilepsy (yrs) 1-46, avg. 19.5, med. 18.5 Sz’s/ mo. baseline 1-315, avg. 67.5, med. 25 Co-AEDs # 1:17, 2:34, 3:26, 4:7 Surgery 11 lobectomy/cortical resection, 2 CCS. Devices 16 VNS, 2 DBS Imaging 39 normal, 9 conformational disorders, 7 FCD, 7 encephalomalacia, 7 neoplasm/AVM. 5 MTS, 4 other Lacosamide in Canada LCM Total daily dose (mg) 300 35 Number of patients 30 25 400 20 15 10 200 5 0 100 50 75 150 450 250 350 500 600 Lacosamide in Canada Responder rate (N=83) 18 14 10 7 21% 16% 12% >30 8% >50 >75 Sz-free Lacosamide in Canada Reasons for discontinuation SE's (nausea, dizziness, discoordination, blurred vision), 4 Psychiatric SE's (paranoia, panic attacks), 2 increased seizures, 2 no improvement, 5 rash, 4 Lacosamide in Canada Case 1 •22 y.o. woman with 6 month h/o episodes of unresponsiveness, associated with lip smacking, lasting 2-3 min., occurring 2-4/month. •Lives with boyfriend. •No consistent contraception •EEG shows left temporal spikes •MRI shows left mesial temporal sclerosis Mesial Temporal Sclerosis Case 1 Issues • Young female in childbearing age • Compliance • Cosmetic side effects • Weight control – Long-term side effects – Birth control – Risk to baby Case 1 options • • • • • Lamictal Tegretol Trileptal Surgery Nothing Case 2 • 65 y.o. man with high blood pressure, irregular heart beat, high cholesterol and a recent stroke. – Reports 3 episodes of head turning to the left and involuntary jerking of the left arm and face lasting 1 min. – On several drugs for control of his various conditions including warfarin Case 2 issues • Multiple drugs – Compliance – Side effects – Interactions – Organ failure Case 2 options • • • • Neurontin Keppra Lacosamide Surgery? Case 3 • Twenty-one y.o. man, obese, with a 6 year history of several Grand Mal seizures per year. On Epival but does not always take it (drowsy, hand tremor) – Sister has seizures too Case 3 issues • Non-compliance – Side effects • Strong potential for social issues – Depression – Inability to buy drugs Case 3 options • • • • • • Tegretol Dilantin Lamictal Topamax Keppra Surgery? Case 4 • 45 y.o lady, single, works as a town librarian in St. Joseph’s Island, gives a history of temporal lobe seizures since mid-teens. They used to occur every week but as she got older, they happen 3-4 times/ y. • Has always been on Tegretol, 4 pills/day. Higher doses make her see double and get dizzy Case 4 issues • Social and geographic isolation – Can’t drive – Can’t find a job in the city – Can’t access specialty care easily • Has read about other drugs but local GP says “this is as good as she’ll ever be” Case 4 options • • • • • • • Lacosamide Tegretol CR Trileptal Lamictal Keppra Topamax Surgery? Summary • Numerous pharmacological choices • Newer AEDs have less potential for drugdrug interaction • Choose AED according to patient profile • If no success, consider surgery