Geriatric Cough Assessment
advertisement

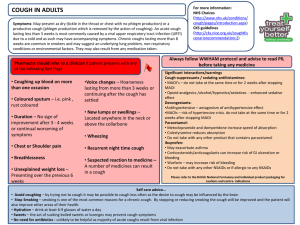
Approach to the Vexing Cough Syndrome Ross Summer M.D. Pulmonary/Critical Care Medicine No conflicts of interest Learning Objectives • Learn the anatomy and neurophysiology of the cough reflex. • Learn the common classification system for cough. • Learn to manage the most common conditions causing cough in the outpatient setting. • Learn the most effective treatments for cough. Cough is common • 5th most common symptom presenting to the primary care setting. • Represents up to 40% of all office visits to a general pulmonary clinic. • Results in 30 million office visits/year in the United States. Braman SS, Prim Care. 1985;12:217–25 Cough is associated with significant morbidity • Health-related effects – Physical - conjunctiva hemorrhage, sleep disturbance, GERD, hernia, rib fractures, intracranial hemorrhage. – Psychological – anxiety, frustration, social stigma. Cough is a costly condition • Decreased productivity (e.g. absenteeism) • 600 million spent/year on OTC cough medications. Anatomy and neurophysiology of the cough reflex Receptors “Cough center” Afferent GN Glossopharyngeal Nerve PN Phrenic Nerve TN Trigeminal Nerve VN Vagus Nerve ?N Cortical Input Efferent RL Recurrent Laryngeal PN Phrenic nerve SMN Spinal Motor nerves Irritants Mechanical Pollutants Tumor Stomach acid Foreign body Cigarette smoke Fibrosis Drugs Airway stricture Enlarged lymph node Cerumen Enlarged Heart Inflammatory Cigarette smoke Asthma, chronic bronchitis Eosinophilic bronchitis Bronchiectasis Post-infectious Upper airway cough syndrome ACE-I , other drugs Common classification system Based on duration of symptom 1. Acute - less than 3 weeks • Most commonly due to an acute respiratory tract infection. 2. Subacute – exists longer than 3 weeks but less than 8 weeks • Most commonly due to a post-infectious process. 3. Chronic - exists greater than 8 weeks • Non-smokers it is most commonly due to drug side effect, chronic rhinitis, asthma or gerd. • In smokers – add COPD and lung cancer Case presentations Chief compliant: “Cough for 6 days” HPI: 75 year-old man presents with acute cough. Initially associated with rhinitis, sore throat, subjective fever but other symptoms have since resolved. Pt states cough occurs throughout the day, but worse at night and it is productive of white-yellow sputum. No post-tussive emesis or sick contacts. ROS: negative PMH: HTN, hypercholesterolemia, osteoarthritis SH: Non-smoker MEDS: HCTZ, lipitor, NSAIDs prn EXAM: Afebrile, hr 80’s, BP 125/80, sats 98% HEENT: boggy nasal mucosa. Chest: clear, normal expiratory time, no crackles, no egophony Heart: normal Abd: unremarkable. Ext: no edema WHAT IS THE MOST APPROPRIATE DIAGNOSIS? A. B. C. D. Lower respiratory tract infection Post-infectious cough Common cold Acute bronchitis Pratter Cough and the Common Cold ACCP Evidence-Based Clinical Practice Guidelines 2006. Wenzel, R. Acute Bronchitis. NEJM 2006. WHAT MICROBES ARE LIKELY RESPONSIBLE FOR PT’S ACUTE BRONCHITIS? • Viral (>90%) – – – – – – Influenza Parainfluenza Metapneumovirus Adenovirus Rhinovirus Coronavirus • Bacterial – Chlamydia pneumoniae – Mycoplasma pneumoniae – Bordetella pertussis Wenzel, R. Acute Bronchitis. NEJM 2006. WHAT IS THE ROLE FOR PATHOGEN TESTING IN ACUTE COUGH? • No role except when Bordetella pertusis is suspected. • This assumes pt is a non-smoker and does not have a history of bronchiectasis. Wenzel, R. Acute Bronchitis. NEJM 2006. IS A CXR NECESSARY IN THE WORK-UP OF ACUTE BRONCHITIS? • No need for CXR unless: – – – – Fever Tachycardia Low oxygen sats Abnormal lung exam • Elderly – 30% with pneumonia do not report a fever. – Only 37% of elderly patients with pneumonia have tachycardia at presentation to the doctor. • Productive cough should not influence your decision – 50% of patients with acute bronchitis will report a productive cough. RAÚL RIQUELME et al Am. J. Respir. Crit. Care Med.1997 Community-acquired Pneumonia in the Elderly WHAT IS THE PRIMARY OBJECTIVE WHEN TREATING ACUTE BRONCHITIS? Patient perspective Get symptom relief Physician perspective Manage expectations. TREATMENT OPTIONS FOR ACUTE BRONCHITIS • Antibiotics • Beta-2 agonists/steroids • Anti-tussive agents (e.g. tesselon pearles, codeine, dextromethorphan). • Anti-inflammatory medications (e.g. steroids, NSAIDS) • Expectorants (e.g. guaifenesin) Antibiotics in acute bronchitis • Little to no role in acute cough in patients without pre-existing lung disease (e.g. COPD, bronchiectasis). – 60% of all patients receive antibiotics – 85% of all elderly patients – 90% of all smokers without COPD • Possible role in early Bordetella pertussis Other treatments in acute bronchitis • Beta-2 agonists – No clear benefit – Viral infections can be a trigger of asthma exacerbations – 40% of all patients have evidence of airflow obstruction • Anti-tussive agents – benefit but studies are mixed. – Codeine – central acting opioid – Dextromethorphan (DM) – central acting non-opioid – Benzonatate (Tessalon pearles) – peripheral-acting anesthetizing agent – Anti-histamines – anticholinergic side effects Other treatments in acute bronchitis • Anti-inflammatory medications – No clear benefit of steroids – Naprosyn – Sperber et al Ann Intern Med 1992 • Expectorants – Guaifenesin (Mucinex) – no evidence to support its use Chief complaint: “Cough is driving me crazy” HPI: Mr W returns to clinic 3 weeks later for further evaluation. States cough is present at all times of day but is made worse by cold air and deep inspiration. Cough is non-productive, and patient denies hemoptysis, fever, chills, rhinitis, shortness of breath, postnasal drip or gastroesphageal reflux symptoms. ROS- frustration, anxiety, chest wall pain, headaches Exam: afebrile, vitals normal HEENT: normal nasal mucosa, no cobblestoning noted. Chest: few wheezes, normal expiratory time. Heart: rrr, no murmurs Abd: unremarkable. Ext: no edema Dx: POST-INFECTIOUS COUGH • Cough lasting > 3 weeks. • It is basically a fancy term for “acute bronchitis that won’t go away.” • Patients are often very frustrated at the time of diagnosis. • Managing frustration is the major challenge for the treating physicians. MANAGE EXPECTATIONS EARLY • Patients with acute bronchitis should be told that cough may last a long time. – 50% of patients with acute bronchitis (>5 days) will still be coughing at 3 weeks (NEJM 2005). – 5-10% of patients will still be coughing at 8 weeks. Braman, S. Postinfectious Cough ACCP Evidence-Based Clinical Practice Guidelines. 2006 WHAT IS THE ROLE FOR CXR IN POSTINFECTIOUS COUGH? • No role unless – Smoker – Immunocompromised – Elderly WHAT IS THE ROLE FOR ANTIBIOTICS IN POST-INFECTIOUS COUGH? • No role unless suspect sinus disease. WHAT IS THE TREATMENT FOR POSTINFECTIOUS COUGH? • Airway injury • Hypersensitive cough reflex – cough often worse with deep inspiration. • Treat with peripheral or central acting anti-tussive agents . (I use chlorpheniramine 4mg tid) • Airway inflammation • Lower airway leading to bronchospasm (e.g. bronchdilators) – cough associated with chest tightness. • Upper airway inflammation leading to upper airway cough syndrome (e.g. inhaled steroids). • Secondary complication • GERD (anti-acid therapy) – cough worse at night HPI: 75 yo man with presents for evaluation of chronic cough. Cough began 2 months ago. Pt doesn’t recall any inciting events. Cough is productive of whitish sputum. Denies association with meals or position. Denies hemoptysis, weight loss, fever, chills, night sweats, nasal congestion, reflux symptoms, shortness of breath or wheezing. ROS: Denies prior lung infections. PMH: HTN, DM, mild proteinuria ALL: NKDA SH: Currently unemployed. Previously worked in construction. Divorced. Lives alone. Never smoked cigarettes. MEDS: enalapril for 10 years Exam: afebrile, hr 80’s, BP 125/80, sats 98% General: well nourished, well developed. HEENT: unremarkable Chest: clear, slightly prolonged expiratory time. Heart: rrr, no murmurs Abd: unremarkable. Ext: no edema, nicotine stained fingers Chronic cough • Cough lasting greater than 8 weeks. WHAT ARE THE MOST COMMON CAUSES OF CHRONIC COUGH? • Upper airway cough syndrome – Allergic – Perennial non-allergic – Sinusitis • Cough variant asthma 1) Non-smoker 2) Not on medication associated with cough. 3) Normal CXR. • GERD/Laryngopharyngeal reflux Irwin et al. The Diagnosis and Treatment of Cough NEJM 2000. Surinder Birring. Controversies in the Evaluation and Management of Chronic Cough AJRCCM 2011 WHAT IS THE ROLE FOR CHEST IMAGING IN CHRONIC COUGH? • All patients should have a CXR evaluation after 8 weeks. WHEN SHOULD AN ACE-INHIBITOR BE STOPPED? • Very high incidence (up to 15% with some ACE-I) • Symptoms are sometimes a clue. Presents with a tickling, scratchy, or itchy sensation in the throat, but can have variable presentation. • It usually begins within one week of instituting therapy, but the onset can be delayed up to 1 year. • It is a more common complication in women than in men, and is also more common in those of Chinese ancestry. • It does not occur more frequently in asthmatics than in nonasthmatics. WHEN SHOULD THE COUGH GO AWAY AFTER STOPPING ACE-I? • Typically resolves within one to four days of discontinuing therapy but can take up to EIGHT weeks! ALMOST ANY DRUG IS ASSOCIATED WITH COUGH! • ANTI-HYPERTENSIVES – Beta-blockers – Ca channel blocker – (e.g. norvasc) – ARB (up to 3%) Practical approach to managing chronic cough in a non-smoker Evaluate for specific cause by H&P Cause not clearly identified Treatment ineffective Obtain CXR CXR normal Initiate treatment for 1 of the 3 most common causes of chronic cough Treatment effective Continue treatment for defined period Cause highly suspected Initiate treatment Treatment effective CXR abnormal Evaluate and treat abnormality Continue treatment for defined period Treatment ineffective Consider referral to subspecialist Pratter MR, Bartter T, Akers S, DuBois J. An algorithmic approach to chronic . cough. Ann Intern Med. 1993;119:977–83 Asthma and cough • Paucity of randomized control trials. • PFTs can be normal. • Role for bronchoprovocation testing is unclear. These tests have a low positive predictive value in healthy controls and may be worse in patients chronic cough. • Trial of steroid + b2 agonist is recommended, but no clear evidence what is the right regimen. • Failure of treatment may relate to ineffective delivery or compliance. UACS • Allergic and non-allergic upper airway symptoms are common but chronic cough is not. • Paucity of randomized control trials. • Anti-histamines will suppress cough through their anti-cholinergic side effects. GERD and Cough • GERD is very common but chronic cough is not. • In patients with chronic cough + low esophageal pH treatment with PPIs improves symptoms in less than 30% of patients (Patterson ERJ 2004). • A Cochrane review concluded that the effect of antireflux therapy is inconsistent and of uncertain magnitude (Chang BMJ 2006). • Randomized control trials have not confirmed the success of earlier uncontrolled studies (Fathi et al Thorax 2008). • Trials rarely have a placebo. • Surgical interventions for GERD do not effectively decrease cough frequency over the long-term. • New trends in treatment of non-acid related reflux. • Skepticism over the diagnosis of laryngopharyngeal reflux is warranted. New Paradigm: Cough reflex hypersensitivity • Abnormally sensitive cough reflex (stretch, cold, flow) is a feature of most patients with chronic cough. • Can be assessed by history or by measuring response to irritants (e.g. citric acid, capsaicin). • Elevated levels of substance P, bradykinin, prostaglandins are found in airways of patients with chronic cough. • Drugs that target the cough receptors need to be developed. Conclusion • Cough is common • Knowledge of anatomy and physiology of cough reflex may prove helpful in identifying a cause. • Treatment is limited but a logical pharmacological approach may prove more effective. Thank you WHEN SHOULD YOU RECOMMEND THAT PATIENTS BE REFERRED TO A SUBSPECIALIST? • Subacute cough – – When primary care physician is no longer able to manage patient expectations (usually occurs when cough lasts > 4 weeks). Subspecialist will provide reassurance. • Chronic cough – – After removal of offending agent (e.g. ACE-I) and treatment for at least one of the most likely etiologies has been ineffective.