COUGH – BTS guidelines
DR O ADEYO
GPVTS ST2
16/04/13
Cough
Acute cough
Chronic cough
History
Examination
Investigation
Specific cough syndromes
Cough clinic referral
Questions/discussion
Acute cough
< 3 weeks
Mostly associated with viral URTI
In absence of significant co-morbidity, usually self-limiting
Little evidence for OTC preparations but patients report benefit
Impact on UK economy
£875 million to loss of productivity
£104 million cost to the healthcare system and OTC medication
Acute cough
Further investigate
Haemoptysis
Prominent systemic illness
Suspicion of inhaled FB
Suspicion of lung Ca
Chronic cough
> 8 weeks
10-20% of adults
Female and obese
10% of respiratory ref to 2◦ care
Decrement in QOL comparable with severe COPD
Most have dry or minimally productive cough
Significant sputum - 1◦ lung pathology
Heightened cough reflex is the 1◦ abnormality
History
Age + sex
Smoking
Characteristic
Onset
Duration
Relation to infection
Sputum
Diurnal variation
Severe coughing spasms/paroxysms
Incontinence
Origin of sensation
Cough triggers + aggravants
Food
Cough on phonation
History
Medication
Occupation/hobbies/pets
PMH
FH
May be familial (inherited anatomical abnormality,
neurological condition)
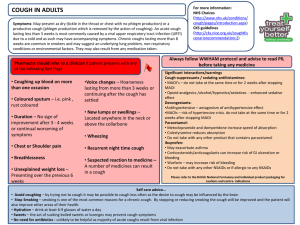
Physical examination
Signs of respiratory disease or cardiac failure
More often examination reveals less specific findings
ENT exam
If FH - neuro exam of legs to look for signs of familial
neuropathy.
Baseline investigations in 1◦ care
CXR
All chronic cough
Acute cough with atypical sx
Assessment of pulmonary function
Spirometry – all chronic cough
Helpful in identifying cough caused by chronic airway obstruction
Normal does not exclude asthma
Avoid using single PEF or PEF to assess bronchodilator
response in diagnosis of airflow obstruction as cause of cough
Specific cough syndromes
Specific cough syndromes
Cough variant asthma
Eosinophilic bronchitis
GORD
Upper airway disease and cough
Undiagnosed or idiopathic cough
Cough due to other common respiratory disease
Cough variant asthma
Chronic cough is the main (if not the sole) symptom
present
it is considered to be a variant type of asthma as well as a
precursor to the development of classical asthma
Clinical indicators include
Nocturnal, post-exercise, post-allergen exposure
Progresses to typical asthma in 17–37% of patients
Hyperresponsiveness is present
Cough variant asthma
In these patients eosinophils in sputum, bronchoalveolar
lavage (BAL) fluid, and in bronchial biopsy specimens is
characteristic
Measurement of airway hyperesponsiveness
Inhalation of methacoline
If negative excludes asthma but does not rule out steroid responsive cough.
Management
Follow guidelines for asthma except no evidence for LABA
Evidence exists for use of Leukotriene receptor agonist
Responds to treatment with inhaled steroids
Eosinophilic bronchitis
Patients have cough and eosinophils in sputum but
spirometric tests and airway hyperresponsiveness is normal
50% of patients with CVA have associated EB
Management
Responds to inhaled steroids
Use BTS asthma guidelines for guidance on dose, preparation and
duration
GORD
Pt’s have increased cough reflex sensitivity which improves
with antireflux therapy
Microaspiration of gastric content into larynx and tracheobronchial
tree
Vagally mediated oesophageal reflex stimulated by acid or non-acid
volume reflux
Oesophageal motor dysfunction and reduced oesophageal clearance
GORD
Management
PPI – omeprazole 20 -40 BD before meals – at least 8 weeks
Prokinetic agents – metoclopramide 10mg TDS may be required in
some
Consider stopping medication that can potentially worsen GORD (
biphosphonates, nitrates, ca channel blockers, theophylline,
progesterones)
Antireflux surgery in carefully selected cases
Upper airway disease and cough
Cough commonly accompanied by
Nasal stuffiness
Sinusitis
Post-nasal drip
In presence of prominent upper airway sx
1 month trial of topical steroid recommended
Can be a diagnostic approach
Undiagnosed or idiopathic cough
Chronic cough should only be considered idiopathic
following thorough assessment at a specialist cough clinic
Clinical hx of reflux is usually present
A typical lymphocytic airways inflammation is seem
Middle aged women
Present with chronic dry cough which starts at time of menopause
Often appears to follow a viral respiratory tract infection
Undiagnosed or idiopathic cough
Organ specific autoimmune disease is present in up to 30%
- autoimmune hypothyroidism is particularly common
Treatment is disappointing and is largely limited to non-
specific antitussive therapy such as dextromethorphan and
drugs with weak evidence of benefit such as baclofen and
nebulised local anaesthetics (lidocaine, mepivicaine)
Low dose morphine recently shown to be helpful
Cough due to other common respiratory diseases
Cough suppression undesirable in certain conditions
LRTI (acute tracheobronchitis + pneumonia)
COPD
Control of sx and reduction of exacebations
No studies on effectiveness of any particular treatment on the cough
itself
Lung Ca
Radiotherapy
Opiod and non-opiod antitussives recommended
Diffuse parenchymal lung disease
Mostly breathlessness though frequently reported
Limited information on treatment
Referral to cough clinic
Lack of availability of relevant diagnostic testing in 1◦ or 2◦ care
Failed trial of empirical treatment directed at asthma, GORD or
rhinosinusitis
History suggestive of serious cough complication such as syncope
or chest wall trauma
Patient preference
Recruitment and participation in clinical trials of antitussive
therapy
References
BTS Guideline. Recommendations for the management of cough in adults. A H
Morice, L McGarvey, I Pavord, on behalf of the British Thoracic Society Cough
Guideline Group
Gp Practice Notebook – a UK medical reference
Cough
Thanks for listening
Any questions?