Tuberculosis Presentation - Wyoming Department of Health
advertisement

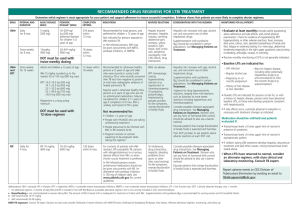
Tuberculosis Wyoming Department of Health Communicable Diseases 307-777-8939 What is Tuberculosis? •An infection caused by Mycobacterium tuberculosis •Spread person to person through droplets released from an infected person by sneezing, coughing, singing or laughing •Can be classified as: •Active TB Disease •Latent TB Infection (LTBI) Transmission •Occurs when an individual inhales infected droplets •Depends on •Infectiousness of TB infected individual •Environment in which the exposure took place •Closed, tight environments pose a greater risk of transmission •Length of exposure •The longer the exposure, the greater the risk •Virulence of TB bacteria Who is at risk? •HIV Infected Individuals •Individuals born in TB endemic countries •Individuals who have been in contact with someone with TB •Alcohol and illicit drug users •Individuals with conditions that may compromise the immune system •Individuals who were previously treated incorrectly for TB infection TB Worldwide •1/3 of the World’s population is infected with TB •Approximately 9 million people became infected with TB in 2010 •1.4 million people die from TB each year •TB is the leading cause of death among individuals with AIDS TB in the United States •The rate of TB in the US in 2010 was 3.6 cases per 100,000 population •The rate has been steadily decreasing since 1992 •A total of 11,182 cases were reported in 2010 •Hawaii reported the highest case rate of 8.8 cases per 100,000 population •Maine reported the lowest case rate of 0.6 cases per 100,000 population Center for Disease Control and Prevention (2011, October 7). Reported Tuberculosis in the United States, 2010. TB in Wyoming •Wyoming is a low incidence state •Reported case rate of 1.3 per 100,000 population in 2010 •This number increased by 0.9 cases per 100,000 population from 2009 •Wyoming had the 42nd highest case rate in 2010 •Active TB Disease is a REPORTABLE disease in Wyoming Active TB Disease •Infectious stage of TB •Manifests six or more weeks after exposure •Occurs when the body cannot control the TB bacteria in the body •Symptoms may include: •Prolonged Cough •Unexplained Weight Loss •Fever •Night Sweats •Chest Pain •Blood in Sputum •Patients diagnosed with active TB disease should: •Be isolated and provided with a mask to wear for doctor appointments, etc •Immediately start a treatment regimen •If HIV status is unknown, an HIV test should be done in order to correctly prescribe the best treatment regimen Diagnosis of Active TB •Physical Exam/Symptom evaluation •Chest X-ray •Cannot confirm TB Disease •Used to detect lung abnormalities or rule out disease •Bacteriologic Cultures (AFB smears) •Used to confirm/rule out TB disease •Sputum sample, bronchoscopy, gastric washing •Sputum Sample •Most cost-effective •Patient coughs sputum into a sterile container at least 3 different times in 8-24 hour intervals, at least one being an early morning specimen Active TB Treatment •Treatment must last 6 months or more (depends on patient’s response to the treatment regimen) •2 phases of treatment •Initial Phase •First 8 weeks of treatment •4 drugs used •Isoniazid (INH) •Rifampin (RIF) •Pyrazinamide (PZA) •Ethambutol (EMB) •Kills most bacteria •Continuation Phase •Starts after the first 8 weeks of treatment until treatment is complete •At least 2 drugs used •Kills remaining bacteria Active TB Treatment •Adherence to proper treatment is essential in treating active TB and avoiding drug resistance •Drugs should be taken as prescribed •This time should be convenient for the patient •Can be monitored by Direct Observed Therapy (DOT) •A medical provider watches the patient take the medication in person, by webcam or other means •Drug resistance can occur if •An improper treatment regimen is prescribed •The patient does not take all of their medication as prescribed Active TB Treatment Evaluation •The patient should be evaluated regularly to ensure the patient is properly responding to treatment by •Symptom evaluation •Chest x-ray •Sputum smears or other bacteriologic specimens •Patients should be reevaluated and treatment regimen should be assessed if: •Symptoms do not improve after 2 months of therapy •Symptoms worsen •Positive cultures remain after 2 months of treatment •Culture results become positive after having a negative culture Active TB Treatment Evaluation •Liver function tests •INH can impact the liver causing hepatitis, liver function tests should be routinely performed on individuals that: •Are HIV positive •Have conditions that may cause hepatitis •Are taking other medications which may cause hepatitis •Are pregnant •Use alcohol regularly •Have symptoms of hepatitis Extrapulmonary TB •More common in young children and HIV infected individuals •Symptoms often coincide with the location of infection •Infection can spread to: •Brain •Kidneys •Bones/Joints •Pleura •Lymph nodes •Larynx •Miliary (Disseminated) TB (very rare) •All parts of the body can be infected •Travels through blood stream Tuberculous lymphadenitis http://www.aafp.org/afp/2005/1101/p1761.html Extrapulmonary TB Tests for Extrapulmonary TB are bacteriologic tests of samples taken from affected areas such as: •Urine sample for kidney •Spinal fluids for TB meningitis •Etc. •Extrapulmonary TB can be treated with 9 months of INH or RIF •Duration of treatment can be shortened to 6 months if a combination of four drugs are used daily for the first two months •For more information visit http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6048a3.htm?s_cid=mm6048a3_w Latent TB Infection (LTBI) •Occurs when an individual inhales infected droplets but the bodies immune system keeps the bacteria under control in the body •Can progress to active TB disease if the immune system cannot continue to control the infection •Asymptomatic •Should be treated to prevent progression to active disease •Is not infectious at this stage Targeted Screening for TB The CDC recommends that the following should be screened for TB: •Close contacts to individuals with active TB disease •HIV Infected individuals •Injection drugs users and users of other high risk substances •Individuals with medical conditions that are at greater risk for TB •Individuals/Employees in high risk congregate settings •Healthcare workers who serve high-risk clients •Individuals born in countries with high prevalence/incidence •Infants and children exposed to high risk adults •WDH recommends that all healthcare facilities conduct the CDC evaluation to determine the frequency for employee screening. Diagnosis •TARGETED Screening/Risk Assessment •A risk assessment should be completed to determine if someone is at risk for TB •This assessment and other resources can be found at http://www.health.wyo.gov/phsd/tb/comptherapy.html •TST/IGRA •If risks are present, a TST test should be placed •BCG status should be ignored after 1 year of vaccination •IGRA is another option but there is limited availability and should be approved by WDH TB Program staff before testing •Chest x-ray •A chest x-ray should be done to rule out active infection if the TST or IGRA is positive Tuberculin Skin Test (TST) •Administration •0.1 mL of PPD tuberculin solution •Inject intradermally on the forearm •Produce a 6 to 10 mm wheal •Reading •Read the test 48-72 hours later •Measure the induration, NOT the erythema •Measure transversely across forearm •Record induration in mm, no induration = 0mm •Positivity depends on risk factors! http://www.health.state.mn.us/divs/idepc/diseases/tb/tst.html LTBI Treatment •Treatment of LTBI is essential in preventing progression into active disease •Treatment regimen is recommended for 9 months but can be done in 6 under specific circumstances •6 month regimen is not recommended for those living with HIV, previous TB disease, or children •INH is the recommended medication •RIF can be given to people who cannot take INH •RIF should not be used in conjunction with certain antiretroviral medications •For more information visit http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6048a3.htm?s_cid=mm6048a3_w Progression of Disease •Progression of LTBI to Active TB Disease is 7%-10% over the lifetime unless other conditions exist •Individuals with LTBI are more likely to progress to active infection within 2 years of becoming infected •Progression of LTBI to Active TB is more likely if: •LTBI is untreated •LTBI is treated improperly •The immune system is compromised (HIV, certain cancers, immune suppressants, etc.) •HIV infected individuals with LTBI have a 7%-10% chance of progression to active infection EVERY YEAR. http://www.answersingenesis.org/articles/am/v2/n3/antibiotic-resistance-of-bacteria Prevention •The spread of TB can be prevented by: •Quickly identifying individuals with TB by targeted testing of those at risk •Isolating individuals with active disease •Correctly utilizing PPE when dealing with an Active TB patient •Promptly starting appropriate treatment for those diagnosed with TB •Verifying that patients are compliant with and complete treatment (DOT) http://www.health.state.mn.us/divs/idepc/diseases/tb/tst.html References Center for Disease Control and Prevention. (2011, May 25). Tuberculosis- Testing and Diagnosis. Retrieved from www.cdc.gov/TB/topic/testing/default.htm Center for Disease Control and Prevention. (2011, October 11). Tuberculosis- Data and Statistics. Retrieved from www.cdc.gov/TB/statistics/default.htm Center for Disease Control and Prevention. (2011, November 2). Tuberculosis- Treatment. Retrieved from www.cdc.gov/TB/topic/treatment/default.htm Center for Disease Control and Prevention. (2010, July 1). Tuberculosis- Basic TB Facts. Retrieved from www.cdc.gov/TB/topic/basics/default.htm Center for Disease Control and Prevention. (2010, July 1). Tuberculosis- Infection control and prevention. Retrieved from www.cdc.gov/TB/topic/infectioncontrol/default.htm