Anesthesia for Infectious Diseases
advertisement
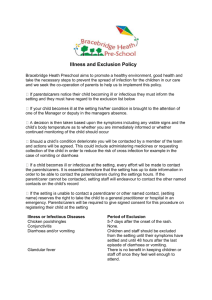
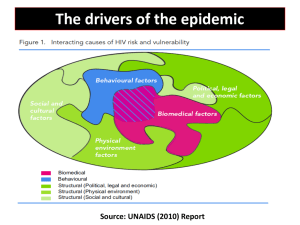
Anesthesia for Infectious Diseases Kanya Kumwilaisak MD Department of Anesthesiology Faculty of Medicine Chulalongkorn University Infectious Disease An infectious disease is a clinically evident illness resulting from the presence of pathogenic microbial agents Mode of Transmission Respiratory system : contact with aerosolized droplets, spread by sneezing, coughing, talking, kissing or even singing Gastrointestinal system : are often acquired by ingesting contaminated food and water Sexually transmitted diseases :are acquired through contact with bodily fluids, generally as a result of sexual activity AIMS Prevent transmission Patient to patient Patient to personal health care provider Know pathophysiology of the infectious diseases Know side effects of medications Respiratory diseases Tuberculosis H1N1 influenza H5N1 influenza SARS Tuberculosis Tuberculosis Diagnosis Symtoms : Persistent cough (eg, lasting longer than 2 weeks),fever, night sweats, weight loss, shortness of breath, haemoptysis, and chest pain. Positive tuberculin skin test Sputum exam and culture Medications Drug Dose Side effect First Line Drugs Isoniazid 5 mg/kg (300mg) Hepatoxicity peripheral neurotoxicity drug interactions Rifampin 10 mg/kg (600mg) Hepatoxicity thrombocytopenia gastrointestinal upset drug interactions Pyrazinamide Based on weight Hepatotoxicity Ethambutol 50 mg/kg (2 g) gastrointestinal upset Arthraglia 15– 20 mg/kg daily Ocular neuritis Anesthetic management Elective surgery should be postponed until they are no longer contagious (three negative sputum smears, improving symptoms and chest X ray) Anesthetic management Liver function test, serum creatinine and platelet count should be performed If ethambutol is used, visual acuity and color vision should be assessed Anesthetic management Type of anaesthetic technique will depend on the type of surgery and degree of involment of respiratory tract regional anaesthesia, patient must wear N95 mask Anesthetic management OR with an antechamber or separated from other areas The fewest health care workers HEPA filters are placed between patient and the ventilator N95 mask in infectious particles area Anesthesia management CO2 absorber should be discarded Two bacterial filters at Y-piece and expiratory limb— a case report Should delay at least 1 hour for the next case No O2 flush for checking circuit H1N1 infection Spread of infection to others Hyper reactive airway Reduced pulmonary functions and Involvement of other body organs H1N1 infection Postpone elective surgery till patient is H1N1 negative In emergent H1N1 positive, it is prudent to operate in an Operation theatre with all precautions as per guidelines for infectious diseases like TB Patient should be isolated throughout the stay in the hospital H1N1 infection HEPA filters, connected between patient outlet and standard anaesthesia tubing a closed system suction catheter should be used HIV infection Human immunodeficiency virus (HIV) is a lentivirus (a member of the retrovirus family) that causes acquired immunodeficiency syndrome (AIDS) Infection with HIV occurs by the transfer of blood, semen, vaginal fluid, pre-ejaculate, or breast milk. HIV infection HIV infection Neurologic system Respiratory system Hematologic system Cardiovascular system Gastrointestinal system AIDS Bacterial infection, multiple or recurrent Candida of the bronchi, trachea, lungs, or esophagus CD4+ T lymphocyte count น้อยกวา่ 200 cells/µL3 Cervical cancer, invasive Coccidioidomycosis, disseminated or extrapulmonaryCryptococcosis, extrapulmonary Cryptosporidiosis, chronic intestinal (>1 month) Cytomegalovirus other than liver, spleen, lymph nodes AIDS Cytomegalovirus retinitis or CMV (with loss of vision)Herpes simplex virus with chronic ulcers (> 1 month), bronchitis, pneumonitis, esophagitis HIV related encephalopathy Histoplasmosis, disseminated or extrapulmonaryIsophoriasis, chronic intestinal (>1month) Kaposi’s sarcoma Burkitt’s lymphomaImmunoblastic lymphoma Lymphoma of the brain, primary AIDS Mycobacterium avium complex or kansasii, disseminated or extrapulmonary Mycobacterium tuberculosis, any site Mycobacterium, any other species, pulmonary or extrapulmonary Pneumocystis carinii pneumonia Pneumonia, recurrent Progressive multifocal leukoencephalopathy Recurrent Salmonella septicemia Toxoplasmosis of the brain Wasting syndrome due to HIV Medications Category Examples Nucleoside/Nucleotide Reverse Transcriptase Inhibitors (NRTIs) zidovudine (AZT), didanosine, zalcitabine, stavudine, lamivudine and abacavir Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs) nevirapine, delavirdine, and efavirenz Protease Inhibitors amprenavir, fosamprenavir, atazanavir, saquinavir, ritonavir, indinavir and nelfinavir Fusion Inhibitors enfuvirtide Integrase Inhibitors raltegravir Side Effects Inhibit cytochrome P-450 (CYP)3A4 Glucose tolerances HAART has both direct hepatotoxicity and nephrotoxicity Anesthetic management CD4 count < 200 cells/µL3 be treated with anteretroviral drugs History and physical exam CBC, coagulation profile, LFT, BUN/Cr, electrolyte Chest radiography ECG Anesthetic management GA or RA Universal precaution Prevent transmission Universal Precuation 1. มีสข ุ ภาพอนามัยดีพร อมทัง้ กายและใจ 2. การรักษาความสะอาดของที่ทาํ งาน 3. การระมัดระวังไม ให สัมผัสสารคัดหลัง่ 4. การสวมเครื่องป องกันให เหมาะสม 5. การตระหนักการป องกันการติดเชื้อ เช น มีสมาธิ หมันล ่ างมือ Universal Precuation Precaution Apparatus - ถุงมือ หน ากาก - เสื้อกาวน - รองเท า - Safe use and disposal of sharps ลดขัน้ ตอนการส งต อด วยมือ ไม ควรหักหรืองอของมีคมก อนทิ้ง ไม ควรปลดเข็มออกจากหลอดฉี ดยาก อนทิ้ง ควรทิ้งในที่ที่เหมาะสมทันทีหลังใช งาน ไม ควรใช เข็มที่มีคมดูดยา ทิ้งภาชนะของมีคมเมื่อมีของเต็ม 2/3 แนวทางปฏิบ ัติเมือ ่ ถูกของมีคมตา ล ้างแผลบริเวณผิวหนังด ้วยน้ าสบู่ mucosa ล ้างด ้วยน้ าเกลือ ื้ พบแพททย์ทันทีเพือ ่ ประเมินการติดเชอ Information for an Occupational Exposure Report 1. Date and time of exposure 2. Detailed description of the procedure being performed 3. Details of the exposure 4. Details regarding the exposure source such as known HBV, HCV, or HIV infection 5. Details about the exposed HCW such as a history of hepatitis B vaccination and antibody status 6. Details about counseling, postexposure management, and follow-up HBV HBIG ภายใน 24 ชวั่ โมงเพือ ่ เป็ น passive prophylaxis HBV vaccine Signs and serology until 6 months HCV Check anti-HCV and alanine aminotransferase activity Follow up 4-6 months ถาผล anti-HCV positive ควรตรวจ ้ recombinant immunoblot essay เพือ ่ ยืนยันการติดเชือ ้ HIV antiretroviral agents for postexposure prophylaxis in24-36 hrs Follow up serology after 6, 12 weeks and 6 months Conclusion Blood-borne Universal precaution Precaution apparatus Hand Hygiene Sharps การทําความสะอาด อุปกรณ์ Air-borne Universal precaution Mask n-95 Isolation Prepare anesthesia circuit การทําความสะอาด อุปกรณ์์