Workshop presentation - World Federation for Mental Health
advertisement

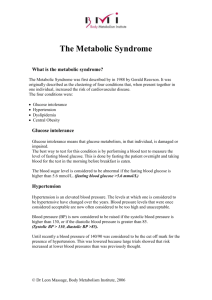
Body and Mind: Metabolic Syndrome and Mental Health A workshop to discuss the management of metabolic issues in people with mental illness Overview • A meeting was convened by the World Federation for Mental Health in September 2004 to discuss mental illness and metabolic syndrome – Attended by ten physicians, consumers and caregiver groups from around the world – Output: “Advancing the treatment of people with mental illness: a callto-action in the management of metabolic issues”, published in Journal of Clinical Psychiatry in June 2005 • Aim of today’s workshop – Summarise the findings published in the JCP article – Discuss practical implementation of the recommendations What is metabolic syndrome? • Metabolic syndrome: – a complex disorder consisting of multiple risk factors that promotes cardiovascular disease and overall mortality and morbidity1,2 – Obesity and insulin resistance are two of the most important causative factors3 – Components may have genetic or environmental basis Hypertension Dyslipidemia 1Ninomiya Impaired glucose tolerance Obesity JK et al. Circulation 2004;109:42-46; 2Malik S et al. Circulation 2004;110:1245-1250; 3Grundy SM et al. Circulation 2005;112(17):e285-90 ATP III definition: the metabolic syndrome • 3 or more risk factors required to meet the definition Factor Measurement Obesity • Waist circumference – Male – Female >102cm (>40in) >88cm (>35 in) Dyslipidaemia • Triglycerides 150 mg/dL (1.7mmol/L) • HDL cholesterol – Male – Female <40mg/dL (<1.0mmol/L) <50mg/dL (<1.2mmol/L) Hypertension 130/85mmHg Fasting glucose 100mg/dL (5.5mmol/L) ATP III = National Cholesterol Education Program Adult Treatment Panel III JAMA 2001; 285: 2486-2497 Prevalence of metabolic syndrome in the general population Country Prevalence of metabolic syndrome USA 20 – 30%1-3 Japan 11.0%4 France 12.4%5 Germany 19.8%6 Italy 14.4%7 Spain 19.5%8 UK 19.6%6 Greece 20%9 Urban Indians 30 – 40%10,11 1Ford ES et al. Diabetes Care 2004;27:2444-2449; 2Park YW et al. Arch Intern Med 2003;163:427-436; 3Haffner S et al. Circulation 2003;108:1541-1545; 4AnuurAD e ET AL. Journal of Occupational Health 2003;45(6):335-43; 5Balkau B et al. Diabetes and Metabolism 2003;29(5):526-32; 6Sattar N et al. Circulation 2003:108(4):414-9; 7Bonora E et al. Int J Obes Relat Metab Disord 2003;27:1283-1289; 8Alverez Leon EE et al. Medicina Clinica 2003;120(5):172-4; 9Panagiotakos DB et al. Am Heart J 2004;147:106112; 10Gupta R et al. Int J Cardiol 2004;97:257-261; 11Ramachandran A et al. Diabetes Res Clin Prac 2003;60:199-204 Metabolic syndrome and mental illness • Metabolic syndrome may be more prevalent in people with mental illness1 – • Their lifestyle factors may contribute to the development of metabolic syndrome2,3 People with mental illness have a reduced life expectancy compared to the general population – Metabolic syndrome (especially CVD) contributes to this4 • Poor diet • Lack of exercise • Smoking • Stress • Medication that causes weight gain • Inadequate self-care • Adherence to prescribed medication • Financial hardship • Poor self-esteem and lack of motivation • Limited availability and co-ordination of medical care 1Holt RI. Diabet Med 2004;21:515-523; 2McCreadie RF et al. Br J Psychiatry 2003;183:534-539; 3Kumar CT. Br J Psychiatry 2004;184:541; 4Marder SR et al. Am J of Psy 2004:161(8);1334-49 Recommendations for metabolic disorder management in people with mental illness Issues • Healthcare professionals (HCPs) need to be fully informed of the increased risk of metabolic disorders and need for intensive monitoring • Collaboration required between HCPs, caregivers and individuals concerned Who should manage physical health monitoring? • Will vary from country to country and from urban to rural setting • Ideally, physical health monitoring should be incorporated into community mental health services – Mental health clinics may be poorly equipped – Psychiatrists may lack familiarity with metabolic monitoring • However, PCPs may be ideally placed – – – – Oversee patients’ complete healthcare programmes Long-term relationship with person and family Co-ordinate general and mental health services But, PCPs often have little specialised training in mental health Conclusion: the prescriber of the medication for the mental disorder should take responsibility for ensuring that monitoring occurs What needs to be monitored? Metabolic risk factor How to monitor When to monitor1 Weight (BMI / waist circumference) Body Mass Index 1 – 3 months Insulin resistance Fasting blood glucose test 4 months – 1 year HbA1c test Blood pressure Standard method 6 weeks – every visit Lipid profile Blood sample (total cholesterol, HDL-cholesterol, LDL-cholesterol and triglycerides) 6 months – 2 years 1Marder SR et al. Am J Psychiatry 2004;161(8):1334-1349 What should be done when evidence of metabolic disorders is identified? • Inform concerned individual of their condition and provide support in making lifestyle changes • Refer for treatment to appropriate HCP – Impaired glucose tolerance / diabetes – Elevated blood pressure – Dyslipidaemia • Review antipsychotic medication – May be associated with weight gain and impaired glucose tolerance1 • Risk / benefit (risk factors vs. efficacy) differs from person to person 1Allison DB et al. Am J Psychiatry 1999;156:1686-96 How can people with mental illness be supported in making lifestyle changes? • HCPs need to provide significant support – Achieving and maintaining weight loss is more likely to be successful when there is a physician-patient partnership1 – Referral of consumers, when relevant, to • Nutritionist or dietician • Substance abuse professionals2 – Motivational interviewing may be helpful when lifestyle changes are being made • Family members / caregivers – Involve where relevant, encourage participation in healthy diet and exercise and provide information 1Hill JO et al. Obes Res 2002;10(suppl 2):124S-130S; 2Steinberg ML et al. Consult Clin Psychol 2004;72:723-728 Conclusions • People with mental illness are at particular risk of developing the components of metabolic syndrome • Prevention of metabolic disorders is key to ensuring the physical health of people with mental illness • Regular and comprehensive monitoring is necessary to ensure proper risk management • Greater overall awareness of metabolic disorders in people with mental illness within the broad medical community is urgently needed • Treatment of people with mental illness is a collaborative effort between clinicians, the person involved and their family / caregivers Discussion Discussion Primary Care Practitioners Goals of discussion • Explore the importance of physical health monitoring in people with mental illness, and how and when monitoring should take place • Develop awareness of key considerations when working with people with mental illness • Discuss tools to facilitate best practice in recording and sharing important information regarding the mental and physical health of people with mental illness • Discuss a best practice checklist for working with people with mental illness Discussion topics • Monitoring metabolic syndrome risk factors – How to monitor – Frequency of monitoring • Encouraging self-monitoring – Obesity – weight change of 3-5kg – Blood sugar – increased thirst / urination • Encouraging healthy behaviour – – – – Healthy eating Increased physical activity Quit / cut down on smoking Decrease alcohol consumption Discussion topics (cont.) • Considerations for people with mental illness – – – – Mental health history Personal stressors / triggers Unusual behaviours to watch out for Other HCPs seen by the individual • Involve families and caregivers – Establish source of support – Build a familiar and trusting relationship with them • Working with mental health specialists – Sharing of information Discussion Mental Health Practitioners Goals of discussion • Share experiences of advising people with mental illness on physical health matters. • Develop awareness of how to listen attentively to people with mental illness and assist them in developing their own healthy living plans • Discuss tools to facilitate and encourage these individuals to take more responsibility for their own health • Discuss a best practice checklist for discussing metabolic syndrome with people with mental illness Discussion topics • Healthy living curve • Identifying unhealthy behaviour – Diet / exercise / smoking • Healthy living pros and cons • Developing a healthy living plan – Diet / exercise / smoking / alcohol / self-help groups / supportive relationships / medication • Implementing a healthy living plan Discussion topics (cont.) • Supportive people – Family members / friends / other HCPs to help put healthy strategies into action • Self-monitoring – Obesity / blood sugar • Medication review Discussion Mental Health Consumer and Family Goals of discussion • Explain how to develop a healthy living plan, and how to talk to physicians and mental health practitioners about metabolic syndrome • Empower you/your relative to take responsibility for physical health and develop a healthy living plan • Discuss tools to facilitate and enable you/your relative to become more involved in decisions about mental and physical health • Discuss a checklist of suggested activities to ensure physical health and help prevent metabolic syndrome Discussion topics • Asking your doctor for physical health monitoring – Weight / blood sugar / blood pressure / fats in blood • Talking to your doctor – Clarify what you want to discuss • Self-monitoring – Weight / blood sugar • Identifying unhealthy behaviour – Diet / exercise / smoking Discussion topics (cont.) • Identifying personal goals • Healthy living plan – Diet / exercise / smoking / drinking / self-help group / supportive relationships / medication • Getting support for a healthy living plan – Family / friends / HCPs • Medication review