Subarachnoid Hemorrhage Management
advertisement
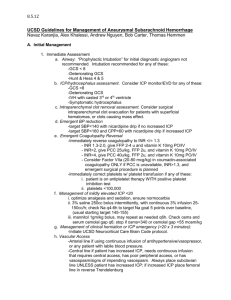
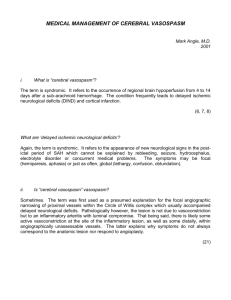
ICU Management of Subarachnoid Hemorrhage Daryl R. Gress, M.D. Louise Nerancy Chair of Neurocritical Care Director of Neurocritical Care ,University of Virginia Disclosures: Scientific Advisory Board Ornim Subarachnoid Hemorrhage Management SAH is complex and fulminate disease •predictable potential complications •need overall treatment strategy •team approach necessary for optimal outcome Subarachnoid Hemorrhage Subarachnoid Hemorrhage –small portion of overall stroke –10-15/100,000 –30,000 cases per year in US –4.5% of all stroke mortality –25% of stroke-related years of life lost <65 Johnston Neurology 1998; 50:1413-18 Subarachnoid Hemorrhage Subarachnoid Hemorrhage –acute mortality 30-50% –survivors have 50% risk of disability –factors •age •clinical status at presentation •medical co-morbidities Subarachnoid Hemorrhage Subarachnoid Hemorrhage- etiologies –trauma –aneurysm –AVM –hypertension –bleeding dyscrasias, malignancies –“angio-negative” Subarachnoid Hemorrhage Subarachnoid Hemorrhage- “angio-negative” –10-20% of spontaneous SAH –benign perimesencephalic •small blood volume •focal, interpeduncular, pre-truncal –other•large blood volume, diffuse or asymmetric pattern •may not have “benign” low risk of recurrence Subarachnoid Hemorrhage – perimesencephalic hemorrhage Subarachnoid Hemorrhage Management Subarachnoid Hemorrhage Clinical Presentation: –headache –transient alteration in consciousness –focal neurologic findings –normal exam possible –Up to 30 % misdiagnosed at initial presentation –Mayer, et al. STROKE 1996 27:1558-63 Subarachnoid Hemorrhage Management Subarachnoid Hemorrhage Diagnosis: –clinical suspicion –non-contrast CT –lumbar puncture –MR- coronal FLAIR images may enhance sensitivity Subarachnoid Hemorrhage Management Subarachnoid Hemorrhage Emergency Treatment: –control MAP- attempt to prevent re-bleed IV labetolol, nicardipine, nitroprusside preserve CPP –anticonvulsants, short term? –need for ventriculostomy? –steroids not necessary –neurocritical care unit admission Subarachnoid Hemorrhage Management Subarachnoid Hemorrhage-Treatment Decisions: Prognosis related to initial Hunt/Hess score- I-V also related to mechanism of brain injury •hydrocephalus •tissue destruction •hypoxia/hypoperfusion Subarachnoid Hemorrhage Management Neurocritical care complications: –neurogenic pulmonary edema –aspiration pneumonia –cardiac ischemic injury –hyponatremia –DVT and pulmonary embolism –fever Subarachnoid Hemorrhage Management Critical Care Complications –cardiac ischemia •EKG changes common: diffuse T wave inversions •arrhythmias: sinus arrest, ventricular fibrillation/tachycardia •CK and troponin leaks •global ischemia: depressed LV function, stunned myocardium •focal ischemia if underlying coronary artery disease –catecholamine excess and calcium injury Subarachnoid Hemorrhage Management Critical Care Complications –cardiac ischemia •Typically apical sparing involving base, sudden onset, CK and troponin leaks •Less commonly apical dilation, delayed onset, less troponin spill, “Takasuba heart” –Spontaneous improvement in LV function over days Subarachnoid Hemorrhage Management Critical Care Complications –hyponatremia •sodium can drop precipitously over hours •typically appears several days after SAH, time course similar to vasospasm •cerebral salt wasting with increases in circulating ANF •some component of SIADH possible in some cases Subarachnoid Hemorrhage Management Critical Care Complications –hyponatremia •sodium supplement always the treatment, enteral or parenteral, may review hypertonic saline •fluid restriction never favored in setting of possible vasospasm –spontaneous resolution of hyponatremia and return of sodium homeostasis over several weeks Subarachnoid Hemorrhage Management Major Problems to Avoid: –aneurysm re-rupture –hydrocephalus –vasospasm Subarachnoid Hemorrhage Management Re-Bleeding following aneurysmal SAH •high risk 2-4% over first 24 hours 20% over 10-14 days •early definitive aneurysm treatment always preferred, even if vasospasm suspected Johnston Ann Neurol 2000;48:11-19 Subarachnoid Hemorrhage Management Hydrocephalus •acute -common at presentation •sub-acute -develops over days •chronic -appears as NPH after weeks/months ventriculostomy or VP shunt increased brain compliance common –altered relationship of ventricular size and pressure Subarachnoid Hemorrhage Management Vasospasm •predictable time course, day 4 to 14 following SAH •predictable location, related to blood clot •some individual variability •Pathology –hemoglobin, oxyhemoglobin likely spasmogen –smooth muscle contraction –inflammatory arteriopathy Subarachnoid Hemorrhage Management Vasospasm Management •nimodipine –small improvement in outcome in early trials –no clear angiographic effect –may work as neuroprotectant –can compromise blood pressure –may need to reduce dose or delete to preserve BP Subarachnoid Hemorrhage Management Standard Vasospasm Management •triple H therapy –hemodilution –hypervolemia –hypertension Subarachnoid Hemorrhage Management Vasospasm Management •hemodilution –rheologic effect –O2 carrying capacity vs. viscosity –optimal hematocrit ~30-35% –rarely need for therapeutic phlebotomy Subarachnoid Hemorrhage Management Vasospasm Management •hypervolemia –increase preload –augment cardiac function, cardiac output –CVP or pulmonary artery catheter monitoring the debate: Is cardiac output an independent variable in determining cerebral perfusion ? Subarachnoid Hemorrhage Management Vasospasm Management •Induced hypertension –cerebral perfusion pressure = MAP - ICP –phenylephrine most useful, norepinephrine –target MAP depends on clinical status, timing, evidence of vasospasm Subarachnoid Hemorrhage Management Vasospasm Management •cerebral perfusion is key •in spasm, blood flow is pressure dependent –not directly related to volume –not directly related to cardiac output –firm belief in absence of adequate data •much of morbidity related to volume overload Subarachnoid Hemorrhage Management Vasospasm Management •vasospasm watch –neurocritical care nursing –CT angiography and CT perfusion –transcranial Doppler •titrate intensity of medical management •maximize therapy to avoid ischemic deficits Subarachnoid Hemorrhage Management Vasospasm Management •maximize therapy to avoid ischemic deficits •if deficits, urgent need for angiography –angioplasty –intra-arterial calcium antagonists –always consider ICP Subarachnoid Hemorrhage Management Vasospasm Management-something new? •endothelin receptor antagonist? •blockade of ETA or ETB prevent/reverse vasospasm in canine models •ET-1 appears as acute phase reactant in CSF •in Phase II clinical trial, clazosentan led to angiographic effect demonstrated without clear clinical effect Subarachnoid Hemorrhage Management Vasospasm Management-something new? •endothelin receptor antagonist? –Conscious II, randomized Phase III trial in surgically clipped aneurysms following SAH –Conscious III, randomized Phase III trial in coiled aneurysms following SAH Subarachnoid Hemorrhage Management Vasospasm Management-something new? •Intravenous sodium nitrite –Nitric oxide donor delivered to vascular endothelium –Vasodilator –Marked effect in primate model of SAH vasospasm –Phase I-II trial at UVA