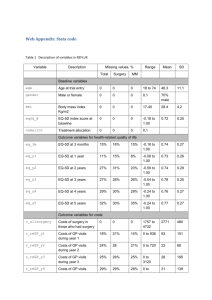
Cost (£) Effect (QALYs)
advertisement

Who is involved in making NICE guidance recommendations and what evidence do they look at? Jane Cowl, Senior Public Involvement Adviser Tommy Wilkinson, Advisor (Health Economics), NICE International Who decides what NICE will recommend? Specialist staff employed by NICE The Department of Health Independent committees of experts Independent committees of NICE staff & experts NICE employed administration staff NHS England Clinical Commissioning Groups NHS finance managers True or False? True or False? True or False? True or False? True or False? True or False? True or False? True or False? Who decides what NICE will recommend? Independent committees Chair At least 2 lay members Health and social care professionals (specialists and generalists) Care providers and commissioners Technical experts e.g. health economist • 2 types: standing committees and topic specific groups • Staff provide technical and administrative support Guidance development phases Scope development and consultation Evidence reviews and economic analysis Draft guidance development and consultation Guidance quality assurance and publication Implementation of guidance Evidence informing committee’s work Reviews of research evidence (all NICE guidance) Grey literature and unpublished data Economic modelling Manufacturers submissions Expert testimony (patient and professional) Stakeholder consultation (all NICE guidance) Occasional additional consultation or fieldwork with practitioners and patients NICE recommendations based on best available evidence The right type of evidence for the question The question dictates the most appropriate study design, for example 'What is the cause of this disease?' Cohort, case-controlled study ‘What does it feel like?’ or ‘What is important to you?’ Qualitative research 'What is the most clinically effective therapy?' Randomised controlled trial (RCT) ‘What works best in diagnosing the condition?’ Observational study or RCT Includes systematic reviews of studies e.g. RCTs where available The nature of evidence Patient evidence High quality patient care (Relevant, effective, acceptable, appropriate) Clinical evidence Economic evidence Acknowledgement: Dr Sophie Staniszewska, RCN Research Institute, University of Warwick Patient evidence Where do we get patient evidence from? RCTs and other quantitative research Qualitative research Both published research and grey literature (e.g. patient surveys) Patient testimonies and commentaries Committee members Consultation The value of patient evidence What insights does patient evidence offer us? Personal impact of living with a condition People’s preferences and values Outcomes that patients want from treatment or care Impact of treatment or care on outcome, symptoms, physical and social functioning, quality of life Risks, benefits and acceptability of a treatment or service Equality issues and considerations for specific sub-groups New information Example – people who self-harm Focus group discussions with people who self-harmed – they were not routinely offered anaesthesia for suturing wounds in the emergency department Nothing in the published research to indicate this was an issue The NICE guideline addresses the issue in its recommendations Adding to the evidence base Example – Psoriasis Clinical research told us the amount of psoriasis was what most affected the quality of life. Patients told us that the location of the flare-up (e.g. face or joints) was more significant. Narrative to contextualise quantitative research Example – promoting physical activity Public health guidance included focus on girls and young women aged 11-18 Evidence from 15 UK qualitative studies of adolescent girls on main barriers and facilitators to being physically active Informed recommendations on supporting girls and young women and helping them to be physically active Patient perspectives – impact and challenges Examples of positive influence of patient evidence on: • • • • Scoping and review questions Evidence reviews Guidance recommendations Research recommendations Challenges • Ensuring patient voices are heard • The weighting of patient evidence • Synthesising with clinical and economic evidence Health Economics at NICE Why consider health economics? Opportunity Cost • If the NHS spends more on one thing, it has to do less of something else (on the margin) • Could we do more good by spending money in other ways? • The ‘opportunity cost’ is the value of the best alternative use of resources Cost effectiveness and the ICER COSTS value of extra resources used Current treatment New treatment CONSEQUENCES (EFFECT) value of health gain “COST EFFECTIVENESS” MEANS TO REFER TO COSTS AND EFFECTS I Incremental: extra, additional C Cost: How much do we have to pay? E Effectiveness: What do we get (in QALYs)? R Ratio: unit per unit e.g. km/h - we use cost per QALY Measuring health outcome – QALY • What is a quality-adjusted life-year (QALY)? – combines both length of life (LY) and health-related quality of life (QA) into a single measure of health gain – The amount of time spent in a health state is weighted by the quality of life (QoL) score attached to that health state – QoL is usually scored with ‘perfect health’=1 and death=0 1 QALY = = = one year of ‘perfectly healthy’ life for one person two years of life with QoL of 0.5 for one person one year of life with QoL of 0.5 each for two people health-related quality of life (utility) Quality-Adjusted Life-Years time (years) Assessing cost effectiveness The Threshold Probability of rejection 1 • Uncertainty • Features of condition • Equity judgments • Availability of treatments • Innovation • Uncaptured health gain 0 £10K £20K £30K Cost per QALY £40K £50K Assessing cost effectiveness Weighing up the benefits, harms and costs Cost (£) New treatment more expensive... ... but some savings from reduced need for care in future New treatment Current practice New treatment more effective... ... but harmful side effects for some people Effect (QALYs) Assessing cost effectiveness Value for money Cost (£) Treatment options in the shaded region are judged to provide good value for money (are ‘cost effective’) New treatment dominated Cost-per-QALY threshold (‘willingness to pay’) High extra cost; low QALY gain Low extra cost; high QALY gain Effect (QALYs) New treatment dominates Considerations beyond efficiency “Decisions about whether to recommend interventions should not be based on evidence of their relative costs and benefits alone. NICE must consider other factors when developing its guidance, including the need to distribute health resources in the fairest way within society as a whole.” NICE Social Value Judgement report http://www.nice.org.uk/aboutnice/howwework/socialvaluejudgements/socialvaluejudgements.jsp