Falls Prevention presentation
advertisement

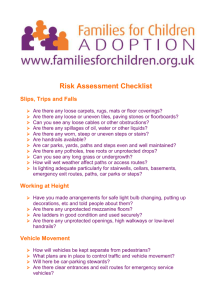
Sara Taylor Senior physiotherapist Jan Benfold Senior Occupational Therapist Babington Specialist Falls Cilinc September 2014 Contents • Introduction to falls and statistics • Discussing risk factors for falls • Effects of falls • Discussion of falls prevention (tips to staying steady) • Outline of falls service for Amber Valley • Practical session on balance • Questions and open discussion to finish Introduction to falls World Health Organisation defines a fall as: “An event which results in a person coming to rest inadvertently on the ground or floor or other lower level”. Excluded: - major internal event e.g. stroke - being hit by an external force e.g. knocked over Falls statistics Approx one third of people >65 fall each year Approx half of people >80 fall each year Approx 9% of older people who fall will become too afraid to leave their homes due to fear of falling again Every year >223,000 people aged over 60 have a fracture as a result of a fall. This is more than the whole population of Northampton. Falls in people aged over 60 account for a cost of £2billion a year 10% of hip-fracture patients will die within 1 month of their fracture and 30% will die within the first year Risk factors for falls Medical Polypharmacy Postural hypotension Medical conditions e.g. PD Poor hydration Anaemia Psychological Reduced motivation/ depression Memory problems/ confusion e.g. dementia Physical Reduced balance Walking problems Reduced muscle strength in legs and arms Poor vision Poor hearing Loss of sensation in feet Environmental Unsafe walking aids Inappropriate footwear Home hazards- lighting, dogs, loose mats, grandchildren, wires, hosepipes Transfers- bath, stairs, bed, chair Effects of falls Psychological Loss of confidence Loss of motivation Isolation/loneliness Depression/anxiety Fear of further falls Physical (Hip) fractures Pain Bruising Head injury Hypothermia Infection Other MSK injuries Functional Loss of independence/increased dependence - impact on social care costs Reduced mobility/activity - impact on quality of life Quality of life Negative circle Risk factor(s) for falls Depression, reduced motivation Reduced activity e.g. socialising Fall Loss of confidence What can we do? Falls prevention 8 tips to Staying Steady: 1. Exercise Tailored exercise programmes can reduce falls by 54% 2. Check your eyes and hearing 3. Look after your feet 4. Ask about you medicines 5. Get enough vitamin D 6. Eat a diet rich in calcium 7. Check for home hazards 8. Visit your GP/local falls service MDT roles and falls Physio: Assess and treat physical problems e.g. - balance - strengthening - increasing movement - exercise tolerance/ stamina Supply aids to help improve safety of mobility OT: Look to return patient back to full function, by working on the following aspects: - physical - emotional - social Look into safety aspects within the home environment Lifestyle changes Nurse: Look at medical issues associated with falls: - Obs- BPs etc - BMs - Skin checks - Continence - Medication checks RSWs: Glue in team Follow physio/Ot treatment plans Complete nursing obs Trained in specialist falls groups- chair based, OTAGO Deliver equipment to patient's homes Named key workers for individual patients Feedback info to therapists and nurses Falls service- AV Runs weekly on Mondays or Fridays 7 week duration 10.30- 15.00 Full multidisciplinary assessment (Physio, OT, Nurse) with outcome measures: - Berg, TUAG, FES, Number of falls Structure group therapy: - Chair based exercise class - OT therapy group - Balance circuit exercises - Tai chi style exercises, Wii rehab or relaxation - Educational talks and group discussions (diet, home safety, getting up of the floor, correct foot ware, medication, benefits of exercise) Week 7: - retested for outcome measures - ongoing rehab (e.g. OTAGO) arranged Ideally telephone follow up in 6 months Linked in services Hearing support services GP Sight support Orthotics Day centres e.g. the Glebe Nurses Strictly no falling Dr Skelly (PD consultant) Walking groups Dietician Active Derbyshire- village games Health trainers Be Active Care coordinators Waistwise Neuro outpatients- Ripley Age UK Future homescapes- alarms, adaptations Medequip Practical Can you walk on a “tight rope”? Can you stand on one leg for 10seconds with your eyes shut Can you walk backwards on your tiptoes Time to exercise Tai chi Chair based exercises Spot the hazards Did you miss anything? Falls hazards: Stairs without handrail Loose extension cords in traffic areas Outdated medications in cabinet Open bottles of medicine Loose rugs Clutter on staircase Flip-flop slippers No handle and no deadbolt on door. Other hazards: Deactivated fire alarm Overloaded outlets Cloth on space heater Smoking. Cigarettes left unattended No automatic shut-off on coffee maker Newspapers too close to lamp Thank you for listening! Any questions? References C. Todd and D. Skelton (2004) What Are the Main Risk Factors for Falls amongst Older People and What Are the Most Effective Interventions to Prevent These Falls? Copenhagen, WHO Regional Office for Europe (Health Evidence Network report. Available at: www.euro.who.int/document/E82552.pdf Age UK http://www.ageuk.org.uk/professional-resources-home/services-andpractice/health-and-wellbeing/falls-awareness-week-18-22-june-2012/ Spotlight Report 2008 (2008) Help the Aged Age UK and Department of Health calculation combined health and social care based on 2010 Department of Health and Personal Social Services Research Unit figures (unpublished) and 2011 census Age UK and Department of Health calculation combined health and social care based on 2010 Department of Health and Personal Social Services Research Unit figures (unpublished) J. Roche et al. (2009) ‘Effect of Comorbidities and Postoperative Complications on Mortality after Hip Fracture in Elderly People: Prospective observational cohort study’, British Medical Journal, 331 (7529): 1374 http://www.who.int/mediacentre/factsheets/fs344/en/ http://www.phac-aspc.gc.ca/seniors-aines/index-eng.php