Unique Anticoagulation Issues 2013
advertisement

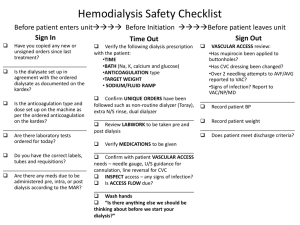
Anticoagulation Issues at University Hospitals Case Medical Center AKA – ALMOST everything you need to know for successful AC management Teresa L. Carman, MD Director, Vascular Medicine Case Medical Center Pager 33515 Office 41261 Discussion • • • • • • Use of the heparin protocol Anti-Xa assay vs. aPTT monitoring Anticoagulation quality measures Safe warfarin dosing Safe discharge of patients Anticoagulation monitoring service referrals Heparin Order Set IV Heparin Protocol • Diagnosis / Weight Based Dosing Low intensity dosing • ACS, Stroke High intensity dosing • VTE, CVT, Afib • Nurse Driven Titration Titration table based on 4 hr anti-xa lab value obtained after initial dosing or titration changes With the change in monitoring the titration table will change to reflect a 6 hr interval for required titrations IV Heparin Protocol • Full Protocol Includes: Initial Loading Bolus Titrated Drip – know the drip rate Additional (Repeat) Bolus (as required) IV Heparin Protocol Ordering Choose the “Loading Dose” to order the initial bolus IV Heparin Protocol Ordering Choose “Continuous Infusion” to order the drip • Includes standard nurse driven titration protocol IV Heparin Protocol Ordering Choose the “Repeat Bolus” for nursing to give a bolus based on Q 4 hr aPTT (anti-Xa) lab value X IV Heparin Protocol Why order the full protocol? Clinical Results: • If the full protocol is NOT ordered 39 hr average time to therapeutic • Full protocol ordered 11 hr average time to therapeutic • All patients were either therapeutic or supratherapeutic within 6 hrs IV Heparin Protocol Why the 4 hour dosing change to the protocol? • With a 6 hour protocol it usually takes 8 hours between dose adjustments • The 4 hour protocol should decrease this interval to approximately 6 hours • This should allow patients to a reach consistent therapeutic range sooner thus impact the risk for recurrent events aPTT VS. Heparin Assay Monitoring Overview of aPTT • The aPTT is used in most clinical laboratories to monitor coagulation and specifically monitor anticoagulants ie. intravenous unfractionated heparin and direct thrombin inhibitors • Clinicians have familiarity with assay • Readily automated • Current targets were established based on data from a post-hoc analysis of a 1972 study which suggested 1.52.5 times aPTT control reduced risk the of recurrent thromboembolism Eikelboom JW. Thromb Haemost 2006;96:547-52. Francis JL. Pharmacotherapy 2004;24:108S-19S. Disadvantages of Using aPTT to Monitor Heparin • aPTT has variable a response to heparin determined by the different coagulometers and the reagents There is no aPTT “standard” When the tissue thromboplastin lot changes, a new therapeutic range needs to be established for the new lot of reagent • Test may be affected by numerous factors other than heparin concentration Baseline elevated aPTT makes titration difficult and inaccurate Eikelboom JW. Thromb Haemost 2006;96:547-52. Francis JL. Pharmacotherapy 2004;24:108S-19S. Conditions that May Prolong the Baseline aPTT • Lupus anticoagulants • Other antiphospholipid antibodies • Prekallikrein, High Molecular Weight Kininogen Level • Low levels (<40%) of: Fibrinogen Prothrombin Factors V, VIII, IX, X, XI, and XII Eikelboom JW. Thromb Haemost 2006;96:547-52. Francis JL. Pharmacotherapy 2004;24:108S-19S. Current Recommendations from CHEST Guidelines • Each coagulation laboratory determines the therapeutic range for their aPTT reagent that correlates with a heparin assay level of 0.3 to 0.7 international units (IU)/mL (by anti-Factor Xa assay) • Each laboratory must determine its own therapeutic range for heparin for the aPTT whenever the aPTT reagent changes or with a change in instrumentation Therefore, the range changes almost annually Hirsh J. Chest 2008;133:141-59 Monitoring Update on Monitoring • As of summer 2011 the “aPTT” is not available for monitoring IV unfractionated heparin therapy at University Hospitals Case Medical Center. (no correlations have been done; no target range exists) • The “aPTT” has been replaced by anti-Xa monitoring using the “heparin assay, UFH” • The use of the “heparin assay, UFH” will standardize IV unfractionated heparin monitoring and make the use of the aPTT inaccurate Heparin Assay • Specifically determines anticoagulant activity of IV unfractionated heparin by measuring ability of heparinbound antithrombin to inhibit a single enzyme • More specific than aPTT since it measures inhibition of a single enzyme • Major advantage is lack of biologic factors that affect its result Eikelboom JW. Thromb Haemost 2006;96:547-52. Francis JL. Pharmacotherapy 2004;24:108S-19S. Comparison of Monitoring with aPTT vs. Anti-Factor Xa Assay • Prospective, single-center study 1.8 P<0.0001 1.6 • 268 patients on IV heparin for variety of indications 1.4 1.2 P<0.0001 1 • Utilizing anti-Factor Xa assay led to fewer tests and dose adjustments N= APTT 0.8 0.6 0.4 0.2 • Cost increase of $1.09/day more using anti-Factor Xa assay Anti-Factor Xa Assay 0 Monitoring Tests/24 hours Dosage Changes/24 Rosborough TK. Pharmacotherapy 1999;19:760-66. Current “High-Intensity Therapeutic Heparin” Anticoagulation Orders Using Heparin Assay for Adult Patients (VTE etc) Current “Low-Intensity Therapeutic Heparin” Anticoagulation Orders Using Heparin Assay for Adult Patients (ACS, stroke) No Changes for the Monitoring of Other Anticoagulants • Prothrombin time/INR is still used to monitor warfarin • Therapeutic monitoring of direct thrombin inhibitors (bivalirudin and argatroban) still use the aPTT • Special monitoring for enoxaparin (Lovenox®) is done by Heparin assay, Lovenox Summary #1 • UH uses the heparin assay, UFH for monitoring all intravenous unfractionated heparin therapy. • The order set will change to reflect the therapeutic ranges for “High-dose” and “Low-dose” indications “high-dose” anti-Xa = 0.3-0.7 IU/ml “low-dose” anti-Xa = 0.3-0.6 IU/ml • The time between adjustments and monitoring will decrease to 4 hours in an effort to shorten the time to therapeutic Anticoagulation Core Quality Measures What are Core Measures ? • Evidence based clinical measures that assess quality of care • • • • • • Impact large populations of patients Tracks outcomes over time Framework to rate healthcare performance Publicly reported Comparison data available Currently used in pay for performance initiatives 4/8/2015 University Hospitals Case Medical Center Quality Assurance/Peer Review Report Privileged Pursuant to O.R.C. Section 2305.24, .251, .252 25 Where is Data Publicly Reported? • Hospital Compare www.hospitalcompare.hhs.gov/ • The Joint Commission www.qualitycheck.org • Ohio Department of Health www.odh.ohio.gov • Leapfrog www.leapfroggroup.org • Health Grades www.healthgrades.com/ 4/8/2015 Quality Assurance/Peer Review Report Privileged Pursuant to O.R.C. Section 2305.24, .251, .252 VTE Core Measure • New Core Measure for 2013 • Includes: • VTE prophylaxis within 24 hours of arrival • ICU VTE • Incidence of potentially preventable VTE • Platelet monitoring for unfractionated heparin • Anticoagulation overlap therapy • Comprehensive discharge instructions • Also part of Meaningful Use Anticoagulation Committee •Approach – Fit compliance into current clinician workflow • No additional resources • No retrospective chart abstraction Basic Essentials 1. All patients require DVT prophylaxis screen on admission 2. The proper prophylaxis is ordered or an appropriate reason for omission is documented Hospital acquired VTE is considered a “never event” 3. VTE treatment transition must meet current guidelines and this is documented and supported by the discharge orders VTE Quality Measure • To meet certain care standards to prevent and treat DVT/PE • Must complete the DVT Risk Assessment Screening on admission Helps determine DVT risk: low, moderate, high or very high – Includes orders based on risk score for both pharmacologic and mechanical prophylaxis – Be sure to enter omission reason if choosing not to order prophylaxis Deep Vein Thrombosis Risk Screening Deep Vein Thrombosis Risk Screening Deep Vein Thrombosis Risk Screening Deep Vein Thrombosis Risk Screening Deep Vein Thrombosis Risk Screening Deep Vein Thrombosis Risk Screening Summary #2 • All patients are risk stratified on admission • All patients have prophylaxis ordered – or – a specific indication for not ordering prophylaxis is required. UFH, LMWH, Fondaparinux Overlap with Warfarin to a Therapeutic INR Rational for a 5 Day Overlap and Discharging Patients on Warfarin Anticoagulation Caveats • When short-acting parenteral anticoagulants are chosen as the starting therapy a minimum of 5 days of overlap between parenteral, short-acting drugs and warfarin is required to complete anticoagulation Unfractionated heparin (UFH) LMWH • Lovenox/enoxaparin, Fragmin/dalteparin, Innohep/tinzaparin Fondaparinux (Arixtra) • The target INR is typically 2.5 (range 2-3) • The INR must be > 2 on 2 consecutive days before stopping the parenteral agent Warfarin Anticoagulant effect (VII, IX) vs. Antithrombotic effect (X, II) Anticoagulant effect can be seen within 2 days Antithrombotic effect takes minimum of 4-5 days due to the t ½ of prothrombin (24-48 hours) Parenteral Anticoagulant to Warfarin Conversion • The anticoagulant effect of warfarin on the INR can be seen within 2 days of initiating warfarin therapy. Laboratory prothrombin time effect due to FVII depletion Does not equate to therapeutic anticoagulation • The antithrombotic effect of warfarin takes minimum of 5 days overlap between the drugs. Minimum time required to achieve a therapeutic level of anticoagulation and reliable thrombin depletion Warfarin Effects • Water soluble, readily absorbed from the GI tract • Interferes with Vitamin K dependent γcarboxylation Coagulant factors • II, VII, IX, and X Anticoagulants • protein C and S How Does Warfarin Work? • Warfarin inhibits the production of active clotting factors in the body Inhibits the activity of Vitamin K • Does not effect the activity of clotting factors that have already been made by the body May take several days to see effects Need overlap therapy with an immediate acting anticoagulant if rapid response is desired • Heparin, Lovenox, Arixtra Parenteral Anticoagulant to Warfarin Conversion • Due to the long half-life of prothrombin (60-72 hours) and the need to fully delete preformed circulating thrombin and replace it with terminally modified prothrombin protein the minimum time to complete anticoagulation is 5 days. • INR rises before this time DO NOT reflect therapeutic anticoagulation. Summary • FVII is a vitamin K dependent protein • It has the shortest t½ of all the vitamin K dependent coagulant proteins • FVII activation initiates the prothrombin time reaction • The initial rise in the INR may be due to rapid depletion of FVII • This does not correlate with depletion of FX and FII (prothrombin) FX and prothrombin have long t½ and take 4-5 days to be adequately depleted – hence the need for 5 days of overlap therapy Parenteral Anticoagulant to Warfarin Conversion • In addition, to ensure consistency the INR must be >2 on 2 consecutive days before the parenteral agent is stopped. • Therefore the MINIMUM time to achieve a therapeutic INR is 5 days. • Most patients will require approximately 7 days to complete anticoagulant conversion to a stable INR on warfarin. Anticoagulation Medication Reconciliation • New drop down box specific to anticoagulant drugs Show screen shot of the drop down • Will include a question about whether the patient had a DVT or PE confirmed during this hospital admission. If yes, then you must enter in the date of the diagnostic test that gave the confirmation • May enter up to 2 anticoagulants that the patient is being discharged on. Anticoagulation Medication Reconciliation New drop down box specific to anticoagulant drugs • May enter up to 2 anticoagulants prescribed at the time of discharge Anticoagulation Medication Reconciliation • Will include a question about whether the patient had a DVT or PE confirmed during this hospital admission. If yes, then you must enter in the date of the diagnostic test that gave the confirmation. Question Date Summary #3 • Overlap therapy for a MINIMUM of 5 days and until a stable therapeutic INR > 2 on 2 consecutive days is required for patients with VTE treated with AC. • Med reconciliation and documentation is imperative for success Safe Discharge on Anticoagulation Why do we care about Warfarin? • It is the most commonly prescribed anticoagulant >31 Million prescriptions dispensed in 2004 • It is the medication most commonly responsible for serious & life-threatening adverse reactions therapeutic window fine line between being helpful & harmful Narrow • Among the top 5 drugs contributing to ER visits • Among the top 2 drugs causing hospitalization Warfarin Anticoagulant effect (VII, IX) vs. Antithrombotic effect (X, II) Anticoagulant effect can be seen within 2 days Antithrombotic effect takes minimum of 4-5 days due to the t ½ of prothrombin (24-48 hours) Dosing Variability The average warfarin dose is 5 mg. Loading doses do not help achieve a therapeutic INR more quickly given the need for a 5 day overlap From Mol Interventions 6: 223-227 Warfarin • Current ACCP guidelines recommend 5-10 mg initial dosing In the elderly, patients who are debilitated, malnourished, have CHF, liver disease or recent surgery or who are taking medications which increase sensitivity to warfarin - initial dose should be ≤ 5 mg • Hospital patients should RARELY receive more than 5 mg initial warfarin dosing • “Loading doses” do not alter the need for overlap and may increase the risk of bleeding • Higher initial doses may be suitable for stable, healthy outpatients Chest 2008;133(3Suppl):454-545. Warfarin Follow Up Appointment All patients discharged on Warfarin: • Discharge instructions must include an appointment for Warfarin follow up monitoring. • Discharging provider enters this information in the follow up section on patient profile (CMC) which has a new option specific to Warfarin follow up. • Includes: The clinic or physician that will cover the follow up monitoring • UH “Coumadin Clinic” is called “Anticoagulation Monitoring Service” Phone number Date next PT/INR is due Summary #4 • Choose warfarin initiation doses based on patient characteristics • NOT 5 mg for everyone • Usually after hospital dc warfarin dose requirements decrease ABX Diet interruption Co-morbid/intervening illness Anticoagulation Monitoring Service AKA – Coumadin Clinic Anticoagulation Monitoring Service Referral AMS Referral Anticoagulation Monitoring Service Referral Steps to schedule an initial visit to the Anticoagulation Monitoring Service: 1. An appointment must be scheduled for the patient to be seen; they are not "walk-in" visits. 2. Complete this form and fax to 216-844-1780 along with recent office note or discharge summary. (Concord Health Center only fax to (440)358-5481 and Geauga only fax to (440)285-6110). 3. Call 216-844-3800 to notify Anticoagulation Monitoring Service of patient and confirm receipt of order form; this will ensure transition of patient and help to prevent gaps in care. An initial appointment can be made for the patient at this time or the scheduling office will contact the patient to schedule. Our goal is to see your patient within 3-5 business days. 4. Orders cannot be taken from Residents, Fellows, CNP's or PA's; a managing physician MUST be listed. 5. The referring physician must ensure an interim management plan is in place until the patient can be seen. 6. The referring physician must ensure that there is a managing physician responsible for the ongoing needs of the patient. The managing physician will be contacted by the Anticoagulation Monitoring Service staff for any patient care related issues. 7. Compliance with appointments and/or medication regimen is expected, otherwise patients will be discharged from the anticoagulation monitoring service with ample warning. Anticoagulation Monitoring Service Responsibilities of the Anticoagulation Monitoring Service Staff: 1. If we are unable to schedule the visit within 3-5 business days of receiving the form or being discharged from the hospital, you will be contacted by our office. 2. The clinic staff cannot initiate anticoagulant therapy, nor can they bridge therapy without orders from the managing physician. Furthermore, they will not assume responsibility for the monitoring of the patient's anticoagulation until the patient has been seen for the initial visit. 3. Progress notes will be sent to the managing physician's office via fax after each visit. Criteria for patient enrollment in the Anticoagulation Monitoring Service: 1. Patient is ambulatory and able to come to the clinic for appointments. The clinic will not provide anticoagulation monitoring for patients receiving home health, hospice or those getting venous punctures at a laboratory. 2. Patients without a managing physician will not be enrolled in the Anticoagulation Monitoring Service. 3. Patients/caregiver should have no previous compliance issues documented and is a willing, active participant in their care. Therefore – engage the PCP early and often Begin the referral process early Anticoagulation Management • Must document and “manage” all aspects of anticoagulation • Minimum of 5 days overlap required • INR max 3 days after starting therapy • Min every 2 days during the transition • Need 2 checks the week following Anticoagulation Monitoring Service SUMMARY • Monitor anticoagulation for a MANAGING PHYSICIAN Nurse driven protocol following the orders of the physician • We ARE NOT responsible for the patient until the first visit – usually 3-5 days after dc If the visit is delayed someone else needs to be monitoring If the visit is missed someone else is responsible • We do NOT dose adjust without orders • Expectations are that the orders are followed – any desirable adjustments may be made and will be followed ie. shorter or longer intervals for management • If warfarin or lovenox etc are required the managing physician must be engaged We will facilitate referrals for the physician with the pharmacy Warfarin Follow Up Appointment All patients discharged on Warfarin: • Discharge instructions must include an appointment for Warfarin follow up monitoring. • Discharging provider enters this information in the follow up section on patient profile (CMC) which has a new option specific to Warfarin follow up. • Includes: The clinic or physician that will cover the follow up monitoring • UH “Coumadin Clinic” is called “Anticoagulation Monitoring Service” Phone number Date next PT/INR is due Referral Numbers • Phone: 216-286-7010 • Fax: 216-201-6012 SUMMARY #5 • When anticoagulation is going to be required engage the PCP early and often • Begin the referral process early Conclusions • On admission ALL patients require DVT risk assessment and prophylaxis orders • Heparin when required - use the order sets High dose vs. Low dose • Anti-Xa monitoring is the UHCMC standard for adult patients • Overlap therapydocumented is required AND must be • Discharge on anticoagulation requires effort PCP contact for follow up/monitoring AMS referral Interim plan for delays in presenting to the AMS ****LMWH or other anticoagulants may require pre-authorization so request SW/pharmacy approvals early