Presentation
advertisement

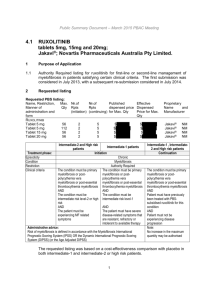
JAK inhibitors update from ASH Claire Harrison Guy’s and St Thomas’ Hospitals London INCB18424 - Ruxolitinib – a JAK 1 and 2 inhibitor Structure and activity in biochemical and cellular assays Enzyme IC50 mean±SD (nM), at 1 mM ATP1 JAK1 3.3±1.2 JAK2 2.8±1.2 JAK3 428±243 TYK2 19±3.2 IC50 Ruxolitinib demonstrated >100-fold selectivity against a broad panel of kinases Ba/F3-EpoR-JAK2V617F cell proliferation assay1 pJAK2/pSTAT5/pERK (Ba/F3-JAK2V617F cells)1 127±17 nM (mean±SD) 128–320 nM Quintás-Cardama et al. Blood 2010;115:3109–17. COMFORT: Phase 3 trials with ruxolitinib (INCB018424) COntrolled MyeloFibrosis study with ORal JAK inhibitor Therapy COMFORT- 1 COMFORT- 2 Design Randomized, Doubleblind, Placebo-controlled Randomized, compared to best-available therapy Random 1:1 2:1 Location USA, Australia, Canada Europe (9 countries) Patient number 309 219 Primary-end point Reduction of spleen size >35% by MRI or CT at 24-w Reduction of spleen size >35% by MRI or CT at 48w Status Reached primary and secondary end-point of symptomatic improvement by MSAF * Reached primary endpoint Verstovsek S N Engl J Med. 2012;366:799-807; Harrison C et al. N Engl J Med. 2012;366:787-798 COMFORT-I Primary Endpoint: % of Patients With ≥35% Decrease in Spleen Volume at Week 24 • Patients who discontinued prior to week 24 or crossed over prior to week 24 were counted as non-responders 5 COMFORT-I and COMFORT-II Comparison of Spleen Volume Reductions 40 P < .0001 Ruxolitinib COMFORT-II At Week 48a Change From Baseline, % Change From Baseline, % COMFORT-I At Week 24a 20 P < .0001 0 -20 35% decrease -40 -60 Ruxolitinib -80 COMFORT-I Week 24 Week 24 Week 48 ≥ 35% spleen vol. ↓, n (%) 95% CI P value 65 (41.9)a (34.1, 50.1) < 0.0001 46 (31.9)b (24.4, 40.2) < 0.0001 41 (28.5)a (21.3, 36.6) < .0001 Percentage spleen vol. ↓, mean (SD) Median –31.6 (18.9) –33.0 –29.2 (19.5) –27.5 –30.1 (22.1) –28.3 Ruxolitinib Arm aPrimary endpoint; bKey secondary endpoint. COMFORT-II Spleen progression criteria ≥ 25% inc from BL ≥ 25% inc from nadir Percent Change From Baseline in Spleen Volume by JAK2V617F Mutation Status Change From Baseline, % At Week 48a Primary endpoint Ruxolitinib BAT JAK2V617F positive (n = 75) JAK2V617F negative (n = 22) Unknown mutation status (n = 1) JAK2V617F positive (n = 24) JAK2V617F negative (n = 8) Unknown mutation status (n = 2) • At week 48, the vast majority of patients receiving ruxolitinib experienced spleen volume reductions, including JAK2V617F-positive (88% [66/75]) and JAK2V617F-negative (91% [20/22]) patients a For patients with spleen volume assessments by MRI/CT at both baseline and week 48. 12 Harrison CN,. Blood (ASH) 2011:Abstract 279. Total Symptom Score: Modified MFSAF v2.0 • uestions 1 to 6 comprise Total Symptom Score • uestion 7 queries inactivity, an impact of MF 0 (Absent) 1 2 3 4 5 6 7 8 9 10 (Worst Imaginable) • dministered 1.During thedaily past 24 hours, how severe were your worst night sweats (or feeling hot or flushed) due to MF? 2. During the past 24 hours, how severe was your worst itchiness due to MF? 3. During the past 24 hours, how severe was your worst abdominal discomfort (feel uncomfortable, pressure or bloating) due to MF? 4. During the past 24 hours, how severe was your worst pain under the ribs on the left side due to MF? 5. During the past 24 hours, what was the worst feeling of fullness (early satiety) you had after beginning to eat due to MF 6. During the past 24 hours, how severe was your worst bone or muscle pain due to MF (diffuse non-joint or arthritis pain)? 7. During the past 24 hours, what was the worst degree of inactivity (including work and social activities) you had due to MF? Mesa RA, et al. Leukemia Res. 2009;33:1199-1203. 8 Mean % Change in Individual Symptoms Ruxolitinib • Worsening n=100 n=124 Abdominal discomfort n=86 n=109 Pain under left ribs n=96 n=122 Early satiety n=90 n=103 Night sweats n=77 n=98 Itching n=89 n=108 n=97 n=119 Improvement Mean % Change From Baseline Placebo Bone/muscle Inactivity pain For all individual symptoms above, comparisons between ruxolitinib- and placebotreated groups were highly statistically significant (P < 0.01) 9 Anemia and Thrombocytopenia Worst Lab Value on Study*,† Grade 1 n (%) Grade 2 n (%) Grade 3 n (%) Grade 4 n (%) Ruxolitinib (n = 146) 24 (16) 55 (38) 50 (34) 12 (8) BAT (n = 70) 16 (23) 28 (40) 15 (21) 7 (10) Ruxolitinib (n = 146) 46 (32) 41 (28) 9 (6) 3 (2) BAT (n = 69) 11 (16) 3 (4) 2 (3) Hemoglobin Platelet count • • • 4 (6) *Occurring on the randomized treatment phase only. †Percentage is based on baseline total67% n. BAT) had grade 1/2 anemia at baseline The majority of patients (63% ruxolitinib; In both arms, all patients who entered the study had grade 0-1 thrombocytopenia at baseline Discontinuations: 1 patient in each arm due to thrombocytopenia and 1 patient due to anemia on the ruxolitinib arm Nonhematologic Adverse Events Regardless of Study Drug Relationship (≥ 10% in Any Group) COMFORT-II Diarrhea Ruxolitinib (n = 146) Nausea All grades Grades 3/4 BAT (n = 73) Pain in extremity Headache Pruritus All grades Grades 3/4 No serious adverse effects on dose interruption……. 12 Long-Term Outcome of Ruxolitinib Treatment in Patients With Myelofibrosis: Durable Reductions in Spleen Volume, Improvements in Quality of Life, and Overall Survival Advantage in COMFORT-I Srdan Verstovsek1, Ruben A. Mesa2, Jason Gotlib3, Richard S. Levy, Vikas Gupta5, John F. DiPersio6, John V. Catalano7, Michael W.N. Deininger8*, Carole B. Miller9, Richard T. Silver10, Moshe Talpaz11, Elliott F. Winton12, Jimmie H. Harvey Jr.13, Murat O. Arcasoy14, Elizabeth O. Hexner15, Roger M. Lyons16, Ronald Paquette17, Azra Raza18, Kris Vaddi4, Susan Erickson-Viitanen4, William Sun4, Victor Sandor4 and Hagop M. Kantarjian1 1University of Texas MD Anderson Cancer Center, Houston, TX; 2Mayo Clinic, Scottsdale, AZ; 3Stanford Cancer Institute, Stanford, CA; 4Incyte Corporation, Wilmington, DE; 5Princess Margaret Hospital, University of Toronto, Toronto, ON, Canada; 6Washington University School of Medicine, St. Louis, MO; 7Frankston Hospital and Department of Clinical Haematology, Monash University, Frankston, Australia; 8Oregon Health & Science University, Portland, OR; 9Saint Agnes Cancer Institute, Baltimore, MD; 10Weill Cornell Medical Center, New York, NY; 11University of Michigan, Comprehensive Cancer Center, Ann Arbor, MI;12Emory University School of Medicine, Atlanta, GA; 13Birmingham Hematology and Oncology, Birmingham, AL; 14Duke University Health System, Durham, NC; 15Abramson Cancer Center at The University of Pennsylvania, Philadelphia, PA; 16Cancer Care Centers of South Texas/US Oncology, San Antonio, TX; 17UCLA Division of Hematology/Oncology, Los Angeles, CA; 18Columbia Presbyterian Medical Center, New York, NY *Currently at Division of Hematology and Hematologic Malignancies and Huntsman Cancer Institute, University of Utah, Salt Lake City, UT Durability of Spleen Volume Reduction 1.0 ≥10% reduction (n=90) Probability 0.8 0.6 ≥35% reduction 0.4 0.2 0 0 8 16 24 32 48 56 64 72 80 88 96 104 41 35 4 4 4 112 Weeks from Onset No. at risk 90 40 84 75 72 63 57 52 47 43 • 90/155 (58%) had a 35% reduction at any time point during the study • 64% maintained a ≥35% reduction for at least 2 years ≥35% reduction: Time from first 35% reduction to <35% reduction and 25% increase from nadir. ≥10% reduction: Time from first 35% reduction to <10% reduction from baseline. EORTC QLQ-C30 Over Time Mean Change From Baseline Global Health Status/QoL Fatigue 20 10 15 5 10 0 5 -5 0 -10 -5 -15 -10 -20 -25 -15 BL 12 24 36 48 60 72 84 BL 96 12 24 36 Ruxolitinib 60 72 84 96 Placebo Role Functioning Mean Change From Baseline 48 Weeks Weeks Physical Functioning 15 15 10 10 5 5 0 -5 0 -10 -5 -15 -20 -10 BL 12 24 36 48 60 Weeks Arrows indicate improvement. 72 84 96 BL 12 24 36 48 Weeks 60 72 84 96 Overall Survival: ITT Population 1.0 Survival Probability 0.8 Ruxolitinib Placebo 0.6 HR=0.58 (95% CI: 0.36, 0.95); P=0.028 No. of deaths: Ruxolitinib=27; Placebo=41 0.4 Median follow up: 102 weeks 0.2 Age adjusted HR*=0.61 (95% CI: 0.37, 0.99); P=0.040 0 0 12 24 36 48 60 72 84 96 108 120 132 Weeks No. at risk Ruxolitinib 155 154 148 145 136 125 121 113 96 44 6 Placebo 154 148 142 133 117 111 102 95 74 32 7 Note: For this unplanned analysis, P-values are descriptive and nominally significant. *Age was the only baseline characteristic that differed significantly between treatment groups as reported in Verstovsek S, et al. N Engl J Med 2012;366:799-807 (median age: ruxolitinib, 66 years; placebo, 70 years; P<0.05). Mean Platelet Counts Over Time • Platelet counts remain stable with longer-term therapy Mean Percentage Change From Baseline 10 Ruxolitinib Placebo 0 -10 -20 -30 -40 -50 -60 BL 12 24 36 48 60 72 Weeks Median platelet count at baseline: Ruxolitinib, 262.0×109/L; Placebo, 238.0×109/L. 84 96 Long-Term Efficacy, Safety, and Survival Findings From COMFORT-II, a Phase 3 Study Comparing Ruxolitinib With Best Available Therapy for the Treatment of Myelofibrosis Francisco Cervantes,1 Jean-Jacques Kiladjian,2 Dietger Niederwieser,3 Andres Sirulnik,4 Viktoriya Stalbovskaya,5 Mari McQuitty,4 Deborah S. Hunter,6 Richard S. Levy,6 Francesco Passamonti,7 Tiziano Barbui,8 Giovanni Barosi,9 Heinz Gisslinger,10 Alessandro M. Vannucchi,11 Laurent Knoops,12 Claire N. Harrison13 1Hospital Clínic, IDIBAPS, Barcelona, Spain; 2Hôpital Saint-Louis et Université Paris Diderot, Paris, France; 3University of Leipzig, Leipzig, Germany; 4Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA; 5Novartis Pharma AG, Basel, Switzerland; 6Incyte Corporation, Wilmington, DE, USA; 7Ospedale di Circolo e Fondazione Macchi, Varese, Italy; 8A.O. Ospedali Riuniti di Bergamo, Bergamo, Italy; 9IRCCS Policlinico San Matteo Foundation, Pavia, Italy; 10Medical University of Vienna, Vienna, Austria; 11University of Florence, Florence, Italy; 12Cliniques Universitaires Saint-Luc and de Duve Institute, Université catholique de Louvain, Brussels, Belgium; 13Guy’s and St. Thomas’ NHS Foundation Trust, London, UK Draft Oral Presentation Duration of Spleen Response Probability of Maintaining Spleen Response Loss of response: no longer a ≥ 35% reduction that is also a > 25% increase over nadir. 1.0 0.9 Ruxolitinib 0.8 0.7 0.6 0.5 0.4 0.3 Ruxolitinib 0.2 No. of Patients Events Censored 0.1 70 18 (25.7%) 52 (74.3%) BAT 1 0 1 (100%) 0.0 0 12 24 36 48 60 72 Weeks • 58% of patients maintain a response at week 84 • The median duration of spleen response has not yet been reached 19 84 96 Draft Oral Presentation Overall Survival 1.0 0.9 0.8 Probability 0.7 0.6 0.5 Ruxolitinib 0.4 BAT Ruxolitinib No. of Patients 146 73 Events 20 (13.7%) 16 (21.9%) Censored 126 (86.3%) 57 (78.1%) 0.3 BAT 0.2 0.1 0.0 n= 146 73 136 61 127 51 116 49 109 45 30 11 0 0 0 24 48 72 96 120 144 Weeks 20 • Suggests a relative reduction in the risk of death with ruxolitinib compared with BAT (HR = 0.51; 95% CI: 0.26-0.99) Biological effects beyond spleen and symptoms? Subjects With ≥ 20% Absolute Allele Burden Reduction at Week 48 or Week 72 PET PMF PPV JAK2 V617F Allele Burden (%) 80 60 40 20 0 0 6 12 24 48 72 Time (weeks) 84 96 • Among patients who achieved a ≥ 20% reduction in allele burden, 39% had PMF, 39% had PPV-MF, and 22% had PET-MF – This distribution was similar to that of the overall study population Percentage of Responders in Each Allele Burden Reduction Group Responders (≥ 35% Spleen Volume Reduction at Week 48) by Absolute Allele Burden Reduction Status % % % % % % % % N = 16 24 14 15 N= 9 23 8 13 • In the ruxolitinib arm, a higher proportion of patients with a ≥ 20% allele burden reduction achieved a ≥ 35% reduction in spleen volume compared with those with a < 10% reduction at both week 48 and week 72 • There were no responders in the BAT arm Phase 3 COMFORT studies • First phase 3 studies in MF • Highly significant reduction of spleen volume and resolution of disabling symptoms • Median duration of response NOT reached • BOTH studies demonstrate survival advantage • Effective regardless of JAK V617F status • Anaemia and thrombocytopenia occur but no increase in grade 4 • No new safety features including no AEs related to discontinuation after 2 year update Spleen Reduction by Palpation on Ruxolitinib Implies Survival Advantage Patients with a confirmed reduction >50% of spleen size had better survival than those with <25% Verstovsek et al, ASH 2011 abstract 3851 Exploring different strategies for use of JAK inhibitors • Earlier disease? • Other drugs? • Combination strategies? Courtesy of Ruben Mesa Trials with Other JAK2 Inhibitors in MF TG101348/SAR302503 CYT387 Study characteristics Phase I, dose escalation Phase I/II, dose escalation Patients, N 59 60 MTD 680 mg/d, G3 elevated amylase 300 mg/d, G3 elevated lipase, headache Spleen reduction , CI 45% 47-53% Constitutional symptoms YES YES Leukocytosis, Thrombocytosis YES, 72% V617F allele burden YES, 39-45% Anaemia response NO Fibrosis response YES ? G3/4 haematological toxicity Anaemia 35%, thrombocytopenia 24%, neutropenia 10% Thrombocytopenia 25% Side effects, non-haematological Nausea, vomiting (G3, 3%) Modest. “First-dose effect" with grade 1 light-headedness and hypotension Pardanani et al. JCO 2011; 29:789-96. Pardanani et al. Blood 201; 116:206 (abstract) YES, 50-57% CI 28 SAR302503 Phase III Study Design Multinational, multicenter, double blind, placebo-controlled randomized study - Intermediate-2 or High risk Primary MF -Post-Polycythemia Vera Myelofibrosis -Post-Essential Thrombocythemia Myelofibrosis No Stratification factor Randomization 1/1/1 RA ND O M I Z A T I ON 75 pts 75 pts 75 pts Q 4 weeks SAR302503 500mg Daily oral doses End of C6 Q 4 weeks SAR302503 400mg Daily oral doses Q 4 weeks Placebo Daily oral doses • 225 pts, Sites ~125, Recruitment: 9 months, 25 countries • Safety data monitored by DMC (Q 6 months) • Cross over possible 30 03/03/13 Cross over 1/1 End of C6 or PD EOT SAR302503 Phase II Study Design: ARD12181 JAKARTA 2 Phase 2, single arm, multicenter, open-label study - Subjects who previously received Ruxolitinib treatment for PMF or Post-PV MF or Post-ET MF or PV or ET for at least 14 days and discontinued the treatment for at least 14 days prior to study entry Recent amendment changing discontinuation period from 30 days to 14 days 70 pts - Intermediate or High risk Primary MF - Post-Polycythemia Vera Myelofibrosis Post-Essential Thrombocythemia Myelofibrosis according to the 2008 World Health Organization (WHO) criteria Dose regimen • SAR302503 once daily, • Starting dose: 400mg/day • Continuously in 28-day cycles • Titration allowed: 200mg, 300mg, 400mg, 500mg or 600mg • Primary endpoint: • % of patients who achieve ≥35% reduction in spleen volume from baseline at C6 EOC by MRI/CT. • Secondary endpoint: • - % of subjects with a ≥50% reduction from baseline to the end of Cycle 6 in the total symptom score using the modified MFSAF • Safety, PK/PD, JAK2V617F allele burden, JAK-STAT and other signaling pathways, OS 32 Country participation 10 Countries – 50 Sites – 70 patients • • Austria (AT) Italy (IT) 2 sites (2 pts) 4 sites (4 pts) Belgium (BE) The Netherlands (NL) 3 sites (6 pts) 2 sites (11 pts) Canada (CA) Spain (SP) 1 site (2 pts) 3 sites (3 pts) France (FR) United Kingdom (UK) 6 sites (8 pts) 1 site (2 pts) Germany (DE) United States 7 sites (11 pts) 21 sites (21 pts) 26 Subjects Enrolled at 12 sites (6 Countries) 23 Subjects under treatment Data cut off: December, 4 Exploring different strategies for use of JAK inhibitors • Earlier disease? • Other drugs? • Combination strategies? Rationale •To reduce unwanted side effects (anaemia, thrombocytopenia) without compromising response •To increase or broaden the benefits seen with JAK inhibitors Potential combination strategies Class Immunomodulators mTOR inhibitors Hypomethylating agents Molecule In vitro study Clinical trial Selected References Pomalidomide Tefferi et al. JCO2009;27:4563-9. Lenalidomide Mesa et al. Blood 2010;116:4436-8 Everolimus Guglielmelli et al . Blood 2011;118:2069-76 Azacitidine Mesa et al. Leukemia 2009; 23:180-2 Decitabine Danilov et al. BJH 2009; 145:131-2 Givinostat Rambaldi et al. BJH 2010; 150:446-55 Panobinostat De Angelo et al (ASH annual Meeting Abstract). 2010;276 Obatoclax mesylate ABT-737 Lu et al. Blood.2010; 116:4284-7 PU-H71 Levine et al. JCI 2010; 120:3578-93 PEGASYS Parikh et al. Clin Lymph Myel Leuk 2010; 10:285-9 Kiladjian et al Blood 2010; 112, 1746 Panobinostat & Ruxolitinib Combo in mouse models of JAK2V617F-driven disease Effects on bioluminescence Baffert eta al Blood 2011, Abstract 798, ASH 201 Panobinostat & Ruxolitinib Combo in MF patients Phase Ib design 37 Combination with BMT?? - Splenomegaly is a negative risk factor for survival after Allo-BMT - Significant improvement in performance status rapid onset no major problem with drug withdrawal i.e. patients are fitter Favourable effects upon cytokine storm and potential effects upon GVHD Current MPN Trials in the UK Academic -open • PT-1 amended – Low risk – Intermediate risk closed expect results next year • MAJIC for HC resistant PV and ET • PEGASYS vs HC for newly diagnosed ET or PV Unfunded but in process • JAKi pre-BMT • SAR302503 + HDAC • Ruxolitinib + azacytadine in sAML Trials • SAR302503 JAKARTA phase 3 –------ Closed UK highest recruiter In ET/PV phase 2; 8 sites selected just reopening JAKARTA-2 in MF resistant of intolerant to ruxolitinib • Pacritinib SB1518 – PERSIST 1 and 2 Vs placebo in MF no lower limited for platelets count prior ruxolitinib allowed. • ?? CYT 387 phase III In Myelofibrosis • Phase 1 ruxolitinib MF low platelets • Phase 1 ruxolitinib PLUS panobinostat Phase 1 ruxolitinib PLUS PI3 kinase inhibitor • Phase 1 ruxolitinib PLUS smoothened inhibitor • To come smoothened inhibitor alone